What is Gonorrhea?
Neisseria gonorrhoeae is a type of bacteria that only affects humans and is spread through sexual contact. This bacteria causes a disease called gonorrhea, which is a serious health concern around the world, regardless of a country’s wealth. Diagnosing and treating gonorrhea often leads to high costs each year. Like other sexually transmitted infections, gonorrhea especially affects young adults.
Interestingly, gonorrhea is an old disease that has been around for a very long time. It’s even written about in the Bible, specifically in the book of Leviticus. There are many slang names for gonorrhea, one of them being “the clap.” It’s believed that this term comes from the name of Les Clapiers, which was historically known as a red-light district in Paris.
What Causes Gonorrhea?
The bacterium N. gonorrhoeae, which only infects humans, typically causes urethritis in men and cervicitis in women. This bacterium is known as an “obligate pathogen,” meaning it needs to cause disease in order to move from one person to another. To survive, these bacteria must infect a host, as they can’t live outside of a host. If not diagnosed or treated, gonorrhea can move up through the genital tract and cause serious reproductive problems. This happens most often in women. Some of these problems can include inflammation of the uterus, pelvic inflammatory disease, infertility, and potentially life-threatening complications from ectopic pregnancies, where the fertilized egg implants outside the uterus.
Risk Factors and Frequency for Gonorrhea
Gonorrhea, caused by the bacterium N. gonorrhoeae, is a major concern for public health as it’s the second most common bacterial sexually transmitted infection worldwide. Every year, about 106 million new cases are recorded among adults worldwide, though many infections go unreported. In the United States, it’s the second most commonly reported sexually transmitted disease, with over 500,000 cases noted each year.
- Gonorrhea is slightly more common in males, partially because males are more likely to show symptoms related to the urinary and genital systems, and partially due to an increased number of diagnoses in men who have sex with men.
- The number of cases of this sexually transmitted infection has gone up over the past ten years because of increasing numbers of strains of the bacteria that are resistant to antibiotics.
Signs and Symptoms of Gonorrhea
For women, the bacteria N. gonorrhoeae often infects the cervix leading to cervicitis. A woman with this kind of infection may experience symptoms such as vaginal discharge, discomfort during urination, or pain in the lower abdomen. An infection in the Bartholin’s glands, which are located near the entrance of the vagina, can result in swelling, pain, and even an abscess. If unrecognized and untreated, this infection can spread to the upper reproductive tract causing diseases like salpingitis and pelvic inflammatory disease. Pelvic inflammatory disease can lead to pain in the pelvic area, infertility, and increased chances of ectopic pregnancy. Gonococcal infections during pregnancy can result in low weight babies and can even spread to newborns causing infections in the throat or eyes.
Interestingly, more than half of female patients with gonococcal cervix infections may not show any symptoms. On the other hand, more than 90% of men infected with urogenital gonorrhea will experience symptoms. Common signs of gonococcal disease in men can include discharge from the penis, discomfort during urination, and testicular discomfort. Complications in men can include conditions like inflammation of the testicles or epididymis, inflammation of penile lymph vessels, swelling of the penis, and narrowing of the urethra after infection. An increase in rectal and throat gonococcal infections has been noted among men who have sex with men.
Like in the cervix, a gonococcal infection affecting the throat, rectum, or the female urethra may not show symptoms or only display subtle ones. If untreated, a rectal infection can cause pain in rectal area, bleeding, discharge, and inflammation of the rectum. In rare cases, N. gonorrhoeae can manifest systemically as fever or sepsis, inflammation of the tendon sheaths, arthritis, and blood vessel inflammation.
Testing for Gonorrhea
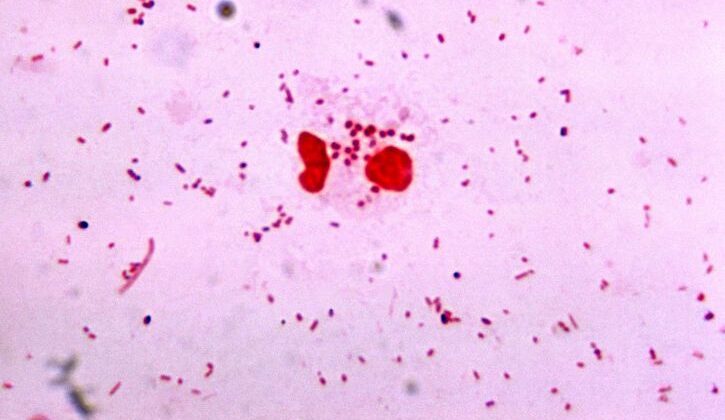
To confirm if a patient has gonorrhea, medical professionals use crucial laboratory tests. These involve detecting the gonorrhea-causing bacteria, N. gonorrhoeae, in urine or swabs taken from various areas like the genitals, anus, throat, or the eye.
In individuals who partake in specific sexual activities, such as anogenital sexual intercourse or insertive oral sex, screenings for gonorrhea are needed from the anus, throat, and genitals. The confirmation of gonorrhea relies on finding the N. gonorrhoeae bacteria or its DNA signature in these samples by methods like light microscopy, culture tests, or nucleic acid amplification tests (NAATs).
Using NAATs routinely to test those at risk of gonorrhea has shown that infections in the throat and rectum are not uncommon. NAATs generally demonstrate high sensitivity and specificity, above 95%, when used on males’ urine samples and swabs from the urethra or cervix.
While point-of-care tests for N. gonorrhoeae infection have helped to shorten the time between testing and treatment, their sensitivity isn’t always as high. This means that patients can get false-negative responses. The rate of such responses can vary widely, between 13% to more than 90%. Because of this variability, it’s often useful to perform repeat laboratory tests after treatment to ensure the infection has been successfully eliminated.
Luckily, advancements have led to the development of multiplex NAATs, which allow for the simultaneous screening of a broad range of sexually transmitted diseases alongside N. gonorrhoeae.
Treatment Options for Gonorrhea
If a doctor suspects you have a gonorrhoea infection because of symptoms like abnormal discharge or because you’ve had sexual contact with someone with an STI, you’re often treated right away. This is because it’s best to start treatment before the test results come in. For such infections, the most common treatment worldwide involves a single injection (either in the muscle or vein) of the antibiotic ceftriaxone. However, if a patient weighs over 150 kg, the dose is increased. If there’s a chance you might also have chlamydia, another STI, the doctor will prescribe another antibiotic, doxycycline, which you take orally twice a day for a week. However, if you are pregnant, a different treatment must be utilized.
In Canada, a slightly different initial treatment for gonorrhoea is used. A single dose of cefixime, which is taken orally, is given along with a single dose of the antibiotic azithromycin. Be aware that large doses of these drugs can cause unpleasant side effects like vomiting. Also, cefixime is not as effective as ceftriaxone for treating throat infections caused by gonorrhoea.
For more severe gonorrhoea infections, including pelvic inflammatory disease, epididymitis, and proctitis, the treatment is slightly different. The doctor may combine a single injection of ceftriaxone with a week’s worth of doxycycline taken orally. This is because doxycycline is more effective against other potential causes of these infections. To make sure you take all your medications properly and thus decrease the chances of the treatment not working, the World Health Organization recommends you take them under direct supervision.
It’s important to know that gonorrhoea bacteria have become increasingly resistant to antibiotics since the first treatments were introduced in the 1930s. In some parts of Asia and Europe, strains of gonorrhoea that are resistant to ceftriaxone have been found. If there’s a high chance you have one of these resistant strains, your doctor might treat you with a single dose of gentamicin, an injectable antibiotic, and a single dose of azithromycin taken orally.
If you have a serious allergy to cephalosporins or B-lactam antibiotics, your doctor could use aztreonam to treat your gonorrhoea infection. Aztreonam is given intravenously and treats urogenital gonorrhoea. Higher doses can also be effective for throat and rectal infections caused by gonorrhoea.
What else can Gonorrhea be?
Gonorrhea, a sexually transmitted infection, causes symptoms similar to other illnesses, including sexually and non-sexually transmitted ones. Other sexually transmitted infections that may result in painful urination, penile or abnormal vaginal discharge, and pelvic pain include Chlamydia, Trichomonas vaginalis, Treponema pallidum, Mycoplasma genitalium, and herpes simplex virus.
Gonorrhea can affect various parts of the body. It’s important to remember that both infectious and non-infectious diseases can lead to inflammation of the urethra, cervix, rectum, eyes, throat, and joints. So, when patients show symptoms that suggest gonorrhea, doctors also consider other causes such as autoimmune diseases, cancer, injuries, and certain forms of poisonings. Additionally, gonorrhea can trigger autoimmune responses like reactive arthritis, which happens along with inflammation of the urethra and eyes.
What to expect with Gonorrhea
The number of people suffering from gonorrhea has increased over the last 20 years. This increase is mainly due to the development of antibiotic resistance.
Possible Complications When Diagnosed with Gonorrhea
Gonorrhea can lead to serious health and financial issues. If not caught or properly treated, gonorrhea can cause severe complications, particularly impacting a woman’s reproductive health. Some of these problems include pelvic inflammation, constant pelvic pain, infertility, abortion in the first three months of pregnancy, and pregnancies developing outside the womb. In rare cases, gonorrhea can spread throughout the body resulting in inflamed joints or heart valve infections. Gonorrhea can also lead to Fitz-Hugh-Curtis syndrome, an inflammation of the capsule surrounding the liver, resulting in the development of adhesions within the abdomen in women, and infertility in men.
Men, specifically, can suffer from additional complications including inflammation of the epididymis, prostate, or rectum. Immune system-related complications after a gonorrhea infection can result in the combination of reactive arthritis, urethritis, and eye inflammation. Babies can get infected with gonorrhea during birth if they come into contact with infected genital secretions, which can result in a type of eye inflammation that might advance to blindness. Being infected with gonorrhea also increases the risk of transmitting HIV/AIDS during sexual intercourse.
A global concern linked to gonorrhea is the development of gonorrhea strains that resist antibiotic treatment, affecting communities differently. Generally, the emergence of antibiotic resistance is related to the amount of antibiotic usage at local, regional, and national levels. For example, countries like Holland which have lower consumption of certain antibiotics like cephalosporins, macrolides, and fluoroquinolones, have fewer cases of antibiotic-resistant gonorrhea compared to countries with high antibiotic consumption patterns.
Complications of Gonorrhea:
- Pelvic inflammation
- Chronic pelvic pain
- Infertility
- First-trimester abortion
- Ectopic pregnancy
- Septic arthritis or endocarditis
- Fitz-Hugh-Curtis syndrome
- Male infertility
- Epididymitis, prostatitis, and proctitis in men
- Reactive arthritis, urethritis, and conjunctivitis
- Gonococcal conjunctivitis in newborns, risking blindness
- Increased risk of HIV/AIDS transmission by sexual activity
- Development of antibiotic-resistant gonorrhea strains
Preventing Gonorrhea
Managing public health concerns like gonorrhea relies on a combination of various strategies. This includes appropriate medication, widespread and specific preventive measures, precise diagnostic tests, alerting potential partners, and ongoing disease monitoring. The key goal of using antibiotics is to clear up individual instances of the infection. This not only helps to lower the risk of complications but also prevents spreading the disease further.
Patients are also advised to avoid any sexual activity for one week after starting the antibiotic treatment. If patients are treated with alternative therapies, if they have other medical conditions such as HIV, or if their symptoms continue, it’s crucial that they check to make sure that the gonorrhea infection is completely gone. This follow-up testing can provide valuable information to prevent unsuccessful treatments. It’s also essential to know that people with gonorrhea have a higher chance of getting other sexually transmitted diseases – like HIV. In fact, nearly 27% of patients who were diagnosed with HIV had also been diagnosed with gonorrhea within the previous year.