What is Burn Evaluation and Management?
Treating burns involves several considerations. First, doctors look at the type of burn. Burns can be caused by heat, chemicals, electricity, or radiation. Then, they consider how much of the body is burned, usually described as a percentage of the total body surface area (%TBSA). They also take into account how deep the burn is: a first-degree burn is minor and affects only the top layer of skin, a second-degree burn is more severe and affects the layers beneath, while a third-degree burn is the most severe and affects the deepest layers of skin.
Last but not least, they consider certain specifics about the patient. This includes the person’s age (especially if they are very young or older than 50), any existing health issues, whether the burn is on a vital part of the body such as face, eyes, ears, nose, hands, feet, or the genital area, and lastly, if the burn happened along with other injuries (for example when someone has inhaled smoke or suffered additional physical trauma).
What Causes Burn Evaluation and Management?
Burns can happen due to a variety of causes. Some of these are:
- Abuse
- Harsh substances like powerful acids, substances used to clean drains (lye), substances used to thin paint, or even gasoline
- Electric shocks
- Exposure to fire
- Pouring of boiling liquids
- Touching very hot items like metals, glass, or other heated objects
- Steam
- Exposure to radiation, like from x-ray machines
- Excessive sunlight or lights that emit ultraviolet rays
Risk Factors and Frequency for Burn Evaluation and Management
Burns, affecting around 86% of individuals, are largely caused by thermal injuries, such as exposure to extreme heat or fire. Comparatively, only about 4% and 3% are caused by electrical mishaps or chemical exposure, respectively. Different types of burns are more common among certain age groups. For instance, flame burns are more frequently seen in adults, whereas scald burns, like hot liquids or steam, are more commonly seen in children under five years old. It’s worth noting that people belonging to low and middle-income groups, as well as those living in low-income countries, are more likely to experience burn injuries.
Signs and Symptoms of Burn Evaluation and Management
Most burns are minor and small, so doctors would usually proceed with a normal examination. However, for severe burns, the patient should be handled like someone with serious injuries, as explained in the chapter on ‘Burns, Resuscitation, and Management’. When reviewing the patient’s situation, it’s important to consider the nature of the burn, the possibility of injuries from inhaling harmful substances, and any other related traumatic injuries. Emergency service providers might be able to provide information on whether the patient was exposed to smoke for a long time (which could lead to carbon monoxide or cyanide poisoning or lung damage), or if the patient may have sustained other injuries from things like explosions, falling, or jumping to safety. The patient’s burn assessment can be done during a secondary survey where the healthcare professional will remove the patient’s clothes and examine them thoroughly in a warm room.
Testing for Burn Evaluation and Management
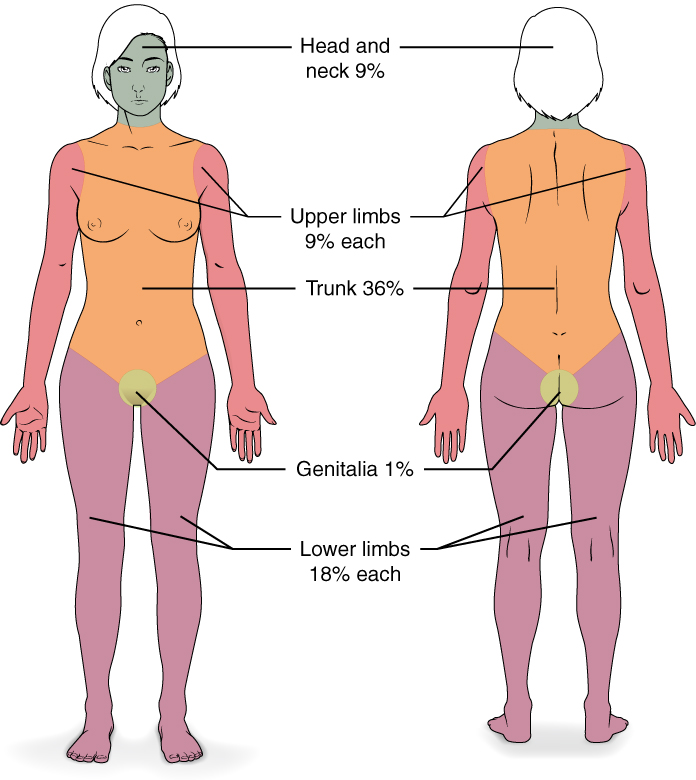
When assessing a burn, doctors look at two important aspects. First, how much of the person’s skin is burned, usually measured by what proportion of their total skin surface area (%) is affected. As an example, if you’ve been burned on both your arms and your chest, health professionals would say that approximately 36% of your body is affected (18% for each arm and 18% for your chest). Second, they consider how deep the burns go into the skin.
Burns can be superficial like a sunburn, which is usually warm, painful, red, and turns white (blanches) if you touch it. They also might blister.
Burns can be partial-thickness which goes further into the skin, causing pain, redness, blisters, and moistness. They still blanch when you touch them. You might get these types of burn from hot surfaces, hot liquids, or fires.
Burns can also be full-thickness which goes even further, reaching the fat layer beneath the skin or further. These burns typically involve less pain because the nerve endings are damaged. The burned area might look white, brown, or charred, feels hard and leathery, and doesn’t turn white when you touch it. In most cases, these types of burn come from a flame, hot liquids, or high-temperature gases.
When doctors calculate what proportion of the body is affected by a burn, they generally don’t include superficial burns – only partial-thickness and full-thickness burns are counted.
There are several methods used to estimate how much of a person’s skin is burned.
The Rule of Nines estimates the percentage based on key body parts. For example, each arm is assumed to represent 9% of the body, the chest and stomach represent 18%, and each leg makes up 18%.
The Lund and Browder Chart is a more accurate method, especially for children.
In the case of small burns, doctors might use the size of the patient’s hand to estimate the burn area. For example, excluding the fingers, the palm of your hand represents about 0.5% of your body’s skin surface. The entire hand, including the fingers, accounts for approximately 1% of your skin surface area.

foot, with a total body surface area of less than 1%.
Treatment Options for Burn Evaluation and Management
The American Burn Association suggests that individuals with specific types of burns should seek treatment at a specialized burn center. These include people with burns covering more than 10% of their body, or with full-thickness burns. Special care should also be taken with burns affecting the face, hands, feet, genitals, or major joints. Those with chemical, electrical or lightning strike injuries, significant inhalation injuries, or burns along with multiple medical disorders or other traumatic injuries, should also visit a burn center.
If someone is sent to a burn center, they don’t need extensive cleaning or special antibiotic creams before they are transferred. If you are helping someone in this situation, it’s best to contact the burn center before beginning more rigorous burn treatments.
When it comes to minor burns that you’re able to treat at home, remember the “C” steps of burn care:
1. Cooling: Small burns can be cooled down with tap water or saline solution. This can stop the burn from getting worse and can also lessen pain.
2. Cleaning: Gently clean the burn with mild soap, water, or an antibacterial wash. There’s ongoing discussion about the best way to treat blisters. Usually, big blisters are cleaned and any loose skin is removed, while small blisters and those on the palms or soles are left alone.
3. Covering: Apply a topical antibiotic cream and cover the area with a bandage or specialized burn dressing.
4. Comfort: Over-the-counter pain relievers might help, and in some cases, prescription pain medication might be necessary. Splints could provide extra support and comfort for some types of burns.
For serious burns (covering more than 20% of the body), it’s important to keep the person hydrated to maintain healthy urine output. The exact amount of fluid needed will depend on factors like the patient’s weight and the severity of the burn.
In cases of moderate to severe burns caused by fire, with suspected inhalation injury, it’s important to check the level of carbon monoxide in the patient’s bloodstream. High amounts of oxygen should be supplied until you’re sure there’s no carbon monoxide poisoning. If poisoning is confirmed, continue supplying oxygen and consider specialized treatments in some cases. Cyanide poisoning can also occur from smoke inhalation, but this can be treated with a specific medication.
What else can Burn Evaluation and Management be?
When examining a thermal burn injury, two other conditions closely resemble this type of injury and must be ruled out:
- Cellulitis
- Toxic epidermal necrolysis












