What is Short-Term Insomnia?
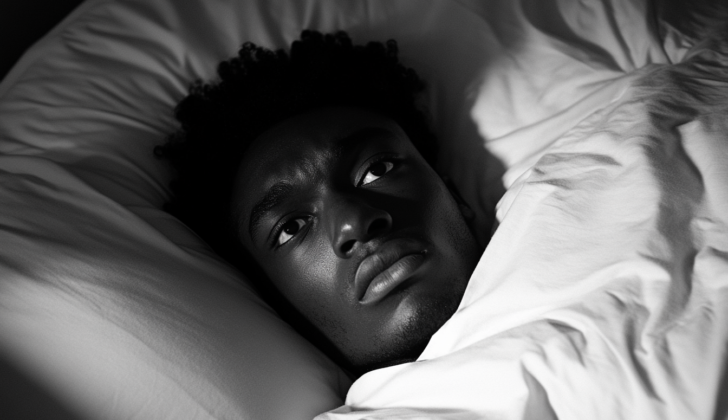
Many people are struggling with sleep issues in today’s busy world. Sleep disturbances like trouble falling asleep or staying asleep fall into a disturbing pattern called insomnia. Insomnia can be divided into two types: short-term and long-term, or chronic. This article mainly focuses on aspects of short-term insomnia.
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), insomnia is categorized as dissatisfaction with sleep quantity or quality due to difficulty falling asleep, staying asleep or inability to go back to sleep given enough time to do so. This problem brings about stress and affects daytime activities, leading to low energy, sleepiness during the day, difficulty focusing, mood swings, and other problems. These sleep troubles are not linked to another medical condition, substance use, or usage of any prescribed medications, and the symptoms must occur at least three nights per week for a minimum of three months.
Historically, insomnia was classified into various types such as primary and secondary insomnia. Recently, these categories have been revised to short-term insomnia, chronic insomnia, and other types of insomnia. Previously used subtypes that now fall under chronic insomnia include conditions like paradoxical insomnia, idiopathic insomnia, psychophysiological insomnia, and inadequate sleep hygiene, among others. These subtypes have recently been removed in the updated edition of the International Classification of Sleep Disorders (ICSD-III).
What Causes Short-Term Insomnia?
The exact cause of short-term insomnia, or difficulty sleeping, isn’t completely clear, and there isn’t just one root cause. Factors contributing to insomnia can vary, being a mix of environmental influences, genetic makeup, mental health, and behavior patterns. All these factors together can lead to a state of increased alertness, or hyperarousal, which makes it harder to sleep.
Risk Factors and Frequency for Short-Term Insomnia
A lot of people around the world are unhappy with their sleep, with about one-third reporting dissatisfaction. It is even more common among older adults and women. Half of seniors say they have trouble sleeping or suffer from insomnia. According to the standards from DSM-5, between 10% to 15% of adults could be considered to have short-term insomnia. Women are twice as likely as men of the same age to have insomnia.
- About one-third of the global population is dissatisfied with their sleep quality.
- This dissatisfaction rate is higher among older adults and women.
- Up to 50% of older adults report sleep disturbances and insomnia.
- Based on DSM-5 criteria, between 10% to 15% of adults could be labeled as having short-term insomnia.
- Women are two times more likely to have insomnia than men of the same age.
Signs and Symptoms of Short-Term Insomnia
Short-term insomnia is a sleep disorder where patients have trouble starting or maintaining sleep, waking up too early, and not being able to fall back asleep. This happens even though they have ample opportunity to get a good night’s sleep. A healthcare provider should take detailed medical and mental health histories from the patient. Maintaining a sleep diary for two to four weeks can also help understand the sleep patterns.
Insomnia doesn’t just ruin a good night’s sleep, but it also causes a domino effect of problems during the day, such as:
- A drop in productivity or performance at work or school
- Feeling tired or low on energy
- Taking frequent naps
- Difficulty in focusing or staying alert
- Increased chances of making mistakes or having accidents
- Difficulty in paying attention, concentrating, or memorizing things
- Changes in mood or feeling irritable
- Problems in social interactions or relationships
- A general feeling of poor quality of life
Questions must be asked to ensure that the patient doesn’t have other sleep disorders like sleep apnea, narcolepsy, or restless leg syndrome.
Recent studies suggest that insomnia might be a separate risk factor for severe depression. This means that a patient with insomnia might also feel persistently sad and lose interest in activities they once enjoyed.
Testing for Short-Term Insomnia
When a doctor wants to diagnose short-term insomnia, they first gather a detailed history of your sleep patterns. A diagnosis is usually achieved through this clinical examination, but it’s also important to rule out other causes of sleep problems. These might include factors like medication use, other health conditions, and mental health issues.
Specialized sleep tests are generally not used often for diagnosing short-term insomnia, but they can be helpful to rule out other sleep disorders like sleep apnea. What’s particularly useful is keeping a ‘sleep diary’ or ‘sleep log’. In these, patients record details about their sleep such as the time they go to bed, if they wake up during the night, how good they feel their sleep was, how long it takes them to fall asleep, and the total time they spend asleep. Usually, these details are recorded for between two to four weeks and used to help make a diagnosis.
Two main systems are used to classify insomnia: the International Classification of Sleep Disorders (third edition) and the Diagnostic and Statistical Manual (fifth edition). The former classifies insomnia into three categories: Chronic Insomnia, Short-term Insomnia, and Other Insomnia. The latter system categorizes insomnia based on how frequently and how long the symptoms persist.
Questionnaires are also useful tools for diagnosing insomnia. The Insomnia Severity Index (ISI) and the Pittsburgh Sleep Quality Index (PSQI) are two examples. The ISI questionnaire consists of seven questions, and each has a score between 1-4. The maximum total score is 28. The higher the score, the worse the insomnia. A score above 14 indicates a clinical insomnia condition. The PSQI questionnaire, on the other hand, helps differentiate between various sleep-related disorders. It involves 19 questions and tracks different aspects of sleep over a month.
There are also ways to objectively measure sleep activity. Actigraphy, a technique that involves wearing a device on the wrist or ankle to measure limb movement, helps record sleep and wakefulness patterns. This data can reveal sleep latency (how quickly you fall asleep), sleep efficiency, total sleep time, and the time spent awake after initially falling asleep. Polysomnography, a more comprehensive sleep study typically performed in a lab, is considered the ‘gold standard’ for diagnosing sleep disorders, but it is generally not used for routine insomnia evaluations. It’s typically reserved for cases where other sleep disorders are suspected, such as sleep apnea or sleep-related movement disorders.
Treatment Options for Short-Term Insomnia
When treating short-term insomnia, there are two primary methods: non-drug treatments and drug treatments. Usually, non-drug treatments are tried first, as they are usually more affordable and have fewer side effects. They have been shown to be just as effective as drug treatments. However, in certain cases where a person has a long history of struggling with sleep, a mix of non-drug and drug-based treatments may be used.
Non-drug treatments for sleep issues can include cognitive therapies, sleep restriction, stimulus control, and sleep hygiene education.
Cognitive therapies involve helping people identify and change thoughts or attitudes that might be causing their sleep issues, such as anxiety or distress. This can often involve changing harmful beliefs, such as worrying too much about not getting enough sleep.
Sleep restriction therapy means limiting the amount of time you spend in bed to the actual amount of time you sleep, which can help improve your sleep efficiency and limit early-morning wake-ups.
Stimulus control therapy aims to only associate the bed with sleep, which means only going to bed when you’re sleepy and not using the bed for anything other than sleep or sexual activity.
Lastly, sleep hygiene education involves understanding and changing behaviors that may be affecting sleep negatively, such as limiting caffeine usage, not napping during the day, and avoiding eating, vigorous exercise, drinking alcohol or smoking near bedtime.
There are also many drug treatments available for treating insomnia, from herbal remedies and over-the-counter melatonin pills to prescribed medications.
Melatonin is a hormone naturally produced by our bodies that helps regulate sleep. Over-the-counter melatonin supplements have shown mild effects on aiding sleep.
There are also many herbs used for relaxation and promoting sleep, such as valerian root, kava-kava, chamomile, and lavender. Each of these herbs works in different ways to support relaxation and sleep.
While the decision to prescribe specific medications is typically based on each individual’s situation, the American Academy for Sleep Medicine (AASM) does provide some guidance. They list a range of different prescription medications that can be used to help manage insomnia.
However, it should be noted that all prescription medications come with potential side effects, which can include addiction, withdrawal symptoms, and a buildup of tolerance. These medications should typically only be used for a short period of time, and only if they are effective.
In treating elderly patients, it’s also important to follow the Beers criteria, a guiding principle for prescribing drugs to seniors. Certain drugs, like benzodiazepines, antihistamines, and tricyclic antidepressants, should generally be avoided in older adults due to their potential side effects.
What else can Short-Term Insomnia be?
Before a diagnosis of short-term insomnia can be made, several other possibilities should be considered and excluded. These include:
- Insomnia caused by the use of certain substances or medications
- Insomnia as a result of a medical condition, such as pain or mental health issues
- Obstructive or central sleep apnea, which are sleep disorders that involve stopped or shallow breathing
- Restless leg syndrome, a condition characterized by an irresistible urge to move the legs
- Narcolepsy, a neurological disorder that affects the control of sleep and wakefulness
- Sleepwalking or sleep nightmares disorder, which are sleep disorders that result in episodes of walking or causing a disturbance during sleep
- Depression and anxiety, both mental health conditions that can affect sleep
- Circadian misalignment from delayed sleep phase disorder, a condition in which a person’s sleep is delayed by two hours or more beyond what is considered an acceptable bedtime
- Shift work sleep disorder, a sleep disorder that affects people who frequently rotate shifts or work at night
What to expect with Short-Term Insomnia
Sleep is a critical element to a person’s overall wellbeing. Research has suggested that problems with sleep and cases of insomnia can potentially increase the risk of heart conditions, metabolic diseases and even early death. When a person has insomnia, their state of being overly attentive or “hyperaroused” can lead to a higher rate of high blood pressure, type 2 diabetes, and heart attacks. This is mainly because insomnia can increase the levels of cortisol, a hormone that the body produces in response to stress.
Further studies have found a link between insomnia and a decline in brain functions. This includes challenges with memory, decision-making abilities, and maintaining attention. Over time, these types of impairments can contribute to the development of mental health conditions, such as depression or anxiety, and might even lead to suicide.
However, if short-term insomnia is treated accurately and on time, the long-term outlook is excellent. This drives home the importance of timely and appropriate interventions and treatments for insomnia.
Possible Complications When Diagnosed with Short-Term Insomnia
Ignoring or not treating short-term insomnia can lead to a variety of problems. Therefore, it’s important for healthcare providers to know about these possible complications. Here are some complications that may arise due to untreated short-term insomnia:
- Reliance on medication for sleep
- Mental health issues, like anxiety and depression
- Heart disease
- High blood pressure
- Type 2 diabetes
Preventing Short-Term Insomnia
In order to understand short-term insomnia, it’s helpful to learn about how sleep functions. Education about good sleep habits and retraining oneself to sleep properly are key aspects in managing insomnia. It’s important to realize that short-term insomnia didn’t just happen all of a sudden. Therefore, treating it will take time and involve making changes to your behavior, habits, and surroundings.