What is Hemorrhagic Stroke?
A cerebrovascular accident (CVA), or stroke, ranks third in causing serious illness or death in many developed countries. Strokes occur in two forms: ischemic and hemorrhagic. Ischemic strokes happen when blood flow to certain parts of the brain is lost, making it a common type of stroke.
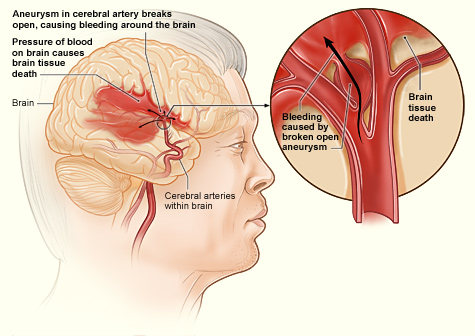
Hemorrhagic strokes, on the other hand, occur when a blood vessel ruptures and bleeds into the brain. These strokes can be further divided into intracerebral and subarachnoid hemorrhage. Intracerebral hemorrhage involves bleeding within the body of the brain itself, while subarachnoid hemorrhage refers to bleeding into the space surrounding the brain. Hemorrhagic stroke is serious and often fatal.
As a hemorrhagic stroke develops, the outcomes usually worsen with it. Early diagnosis and immediate treatment are crucial because as the bleeding expands, it typically causes a quick worsening of consciousness and neurological functions.
What Causes Hemorrhagic Stroke?
High blood pressure, or hypertension, is the leading cause of a type of stroke known as hemorrhagic stroke. Chronic high blood pressure can weaken and damage arteries, leading to a state where blood vessels develop abnormalities such as bulges (microaneurysms), dilations, and ruptures. These ruptures can occur in many places, from brain artery branches originating from basilar arteries or the anterior, middle, or posterior cerebral arteries.
Severe hypertension can cause a specific type of brain bleeding called a non-lobar intracranial hemorrhage. This can happen suddenly, as seen in a condition called eclampsia, which can cause brain bleeding after childbirth, known as postpartum intracranial hemorrhage.
A condition called cerebral amyloid angiopathy (CAA) is another significant cause of brain bleeding in older adults. This condition is characterized by a peptide called amyloid-β depositing in brain vessels, causing them to rupture and bleed. It is often linked with certain genetic variations and can also occur in a hereditary form due to mutations in the amyloid precursor protein gene. As a person ages, the chances of developing this condition grow, and by the age of 70, about half the population suffers from CAA. This can lead to recurrent episodes of bleeding.
Other major risk factors for brain bleeding include smoking, heavy drinking, chronic liver disease, decreased low-density lipoprotein cholesterol, and low triglycerides. Certain medicines, such as ones involving dual antiplatelet therapy, and drugs like cocaine, heroin, and amphetamines can also increase the risk. Conditions characterized by tiny brain bleeds (CMBs), linked with high blood pressure, diabetes, and smoking, could lead to a higher risk. Generally, the risk increases with age, especially after 55, and is higher in men.
Certain brain tumors, like glioblastoma, lymphoma, metastasis, meningioma, pituitary adenoma, and hemangioblastoma, are more likely to bleed.
Conditions like a ruptured aneurysm, arteriovenous malformation, vasculitis, cerebral artery dissection, dural sinus thrombosis, and pituitary apoplexy typically cause spontaneous subarachnoid hemorrhage. Factors like high blood pressure, oral contraceptive pills, substance abuse, and pregnancy can increase the risk of these conditions.
Finally, eclampsia, a pregnancy-related condition, might cause a type of brain hemorrhage (intracerebral or subarachnoid) due to loss of control over blood flow in the brain.
Risk Factors and Frequency for Hemorrhagic Stroke
Hemorrhagic stroke, a type of stroke involving bleeding in the brain, accounts for 10% to 20% of all strokes worldwide every year. The percentage of strokes that are hemorrhagic varies by country, with 8-15% in places like the U.S., the U.K., and Australia, and a higher range of about 18% to 24% in Japan and Korea.
- Every year, 12% to 15% of cases out of 100,000 are hemorrhagic strokes.
- These strokes are more often seen in lower and middle-income countries, particularly in Asia. They also appear more frequently in men, and the rate increases with age.
- The global incidence of this type of stroke is on the rise, primarily in African and Asian countries.
- Research from Japan suggests that controlling blood pressure can lower the incidence of hemorrhagic stroke.
- The rate of fatality from these strokes varies by income. In high-income countries, around 25% to 30% of cases result in death. In lower to middle-income countries, the fatality rate jumps to 30% to 48%.
- The effectiveness of critical care for stroke patients greatly influences these fatality rates.
Signs and Symptoms of Hemorrhagic Stroke
A stroke can show up differently depending on the type and location. Common symptoms include difficulty speaking, muscle weakness on one side of the body, and facial drooping. In particular, a type of stroke called a hemorrhagic stroke tends to start suddenly and get worse quickly. This might cause symptoms like:
- Sudden, severe headache
- Vomiting
- Stiff neck
- High blood pressure
- Quickly developing neurological signs
Some more specific symptoms might happen depending on the location of the bleeding in the brain:
- Headaches are usually more common when there is a large area of bleeding
- Vomiting may happen when the pressure inside the head increases, especially with bleeding in the cerebellum
- Coma could happen if the bleeding involves a part of the brain called the reticular activating system
- Seizures, speech difficulties, and vision problems can happen with lobe-level bleeding. This could also be preceded by numbness, tingling, and weakness
If the bleeding happens in areas called the basal ganglia and thalamus, it might cause muscle weakness or complete loss of sensation on the opposite side of the body. Thalamic bleeding can sometimes extend to the midbrain and cause difficulties with eyelid lifting, eye movement, and pupil reactions. If bleeding happens in the brainstem, it could result in cranial nerve problems and muscle weakness on the opposite side of the body. Brainstem bleeding is also often seen in conjunction with pontine hematoma, which might lead to coma and weakness in all limbs.
Bleeding in the cerebellum could also cause symptoms of increased pressure inside the head, such as slowed heart rate, vomiting, and sluggishness. If these get progressively worse, it could be a sign that the bleeding is enlarging or edema (swelling in the brain) is increasing.
Subarachnoid hemorrhage, another type of stroke, often features extreme headache – described as a ‘thunderclap’, vomiting, fainting, light sensitivity, stiff neck, seizures, and reduced alertness. Other signs can include pain when straightening the knee with the thigh bent at 90 degrees (Kernig sign) or involuntary bending of the hip when the patient’s neck is bent (Brudzinski sign).
Testing for Hemorrhagic Stroke
A CT scan is usually the first step when it comes to investigating a brain bleed. This kind of scan is particularly good at spotting fresh bleeding, as it can show changes in blood density over time. However, certain conditions like anemia or blood clotting disorders can lower this density.
The sensitivity of MRI scans is similar to that of a CT when it comes to detecting fresh bleeding. Also, MRI scans are more precise than CT scans in identifying previous bleeding.
As time passes, the bleeding might blend in with the brain tissue on a CT scan. That’s when an MRI is necessary.
The size of the bleeding area can be determined using a specific formula, where larger bleedings (over 60 ml) can indicate a higher risk of mortality.
Other things that can point to a poor prognosis include the expansion of the bleeding, the bleed reaching into the cavities of the brain, an under-the-tent location, and a specific sign on the CT scan that shows accumulating contrast medium (the “spot sign”).
An MRI scan can be particularly helpful because it can pick up early signs of bleeding due to its sensitivity to a particular type of hemoglobin. Acts like a CT scan, it’s good at spotting fresh bleeding and it can help differentiate between a stroke caused by clotting and a primary bleed. An MRI can also detect the potential causes of secondary bleeding, such as a malformed blood vessel, a brain tumor, or a blocked cerebral vein.
A CT angiogram can show if there’s still ongoing bleeding. It can also rule out causes of secondary stroke caused by bleeding, such as malformed blood vessels, burst aneurysms, blocked cerebral veins, inflammation of blood vessels, and a particular type of blood vessel disorder called moyamoya disease.
Brain scans can also provide clues about the underlying disease. For example, older bleeding in the parietal and occipital lobes may indicate a condition called cerebral amyloid angiopathy. Meanwhile, bleeding in a particular artery could suggest a stroke caused by clotting.
If there’s a possibility of a subarachnoid hemorrhage (a type of stroke caused by bleeding into the space around the brain), a four-vessel angiography is necessary. If this test comes back negative for an aneurysm, it should be repeated after one week and again after six weeks.
Signs on a CT scan that may indicate malformed blood vessels could include an unusual shape or location of the hemorrhage, abnormally large blood vessels or calcifications at the bleed’s margins, abnormally high blood density within a venous sinus, and the presence of too much swelling relative to the time of the presumed bleed.
An additional MRI scan may be helpful in detecting secondary causes for these types of strokes if the bleed’s location is lobar, the patient is younger than 55, or there’s no history of high blood pressure. An MRI or CT venography could be indicated if there’s a suspicion of cerebral venous thrombosis, which refers to a blood clot present in the brain’s dural venous sinuses.
Blood tests like bleeding time, clotting time, platelet count, peripheral smear, prothrombin time, and activated partial thromboplastin time can reveal any abnormalities related to bleeding or blood clotting and any blood disorders which can cause a bleed. Liver and kidney function tests are also important to rule out any dysfunction in these functioning areas as a potential cause. Tests for vasculitis include the evaluation of certain antibodies and other blood components related to the immune system.
Treatment Options for Hemorrhagic Stroke
The best way to treat a stroke that involves bleeding in the brain, also known as a hemorrhagic stroke, is a topic with varying opinions. There are several major studies, such as ATACH, INTERACT, FAST, and STICH that aim to determine the best approach.
When a person experiences a hemorrhagic stroke, their blood pressure needs to be carefully controlled. Doctors try to gradually lower blood pressure to 150/90 mmHg using medications like beta-blockers, ACE inhibitors, calcium channel blockers, or hydralazine. Various studies have shown differing results on the effect of this blood pressure reduction; some have shown it to affect the growth of the bleed in the brain and outcomes after three months, while others found it had no significant impact.
In addition to managing blood pressure, doctors must also control increased intracranial pressure (ICP) – the pressure inside the skull. This can be done by raising the head of the bed, giving the patient medications called osmotic agents, and providing oxygen after intubation and sedation.
To prevent the bleed in the brain from increasing in size, treatments known as hemostatic therapy are given. Patients taking blood-thinning medications may need additional treatments to help their blood clot normally.
Seizures can occur following a hemorrhagic stroke. Patients who show seizure activity on an EEG, or who have observable seizures, are treated with anti-seizure medications.
There are a variety of surgical treatments for hemorrhagic stroke, including craniotomy, decompressive craniectomy, and several types of aspiration techniques. However, these treatments don’t always improve outcomes and can even be harmful in some cases. The decision to use surgery depends on the size and location of the bleeding in the brain and the patient’s condition. For example, surgery is often necessary for patients with large cerebellar hemorrhages (bleeding in the brain’s cerebellum).
Lastly, good medical care, nursing, and rehabilitation are crucial parts of recovery from a hemorrhagic stroke. These strokes often cause problems such as difficulty swallowing, irregular heartbeat, kidney problems, and others, so patients need to be closely monitored and treated for these conditions. Additionally, efforts are also made to maintain a patient’s blood glucose at an appropriate level.
Overall, determining the best way to treat a hemorrhagic stroke often depends on the individual patient’s condition and requires careful consideration of various treatment options.
What else can Hemorrhagic Stroke be?
When trying to diagnose a hemorrhagic stroke (a type of stroke that occurs when a blood vessel in the brain bursts or leaks), doctors may consider several other health conditions that may cause similar symptoms. These include:
- A sudden and severe increase in blood pressure (acute hypertensive crisis)
- Emergency disorder of the pituitary gland (pituitary apoplexy)
- Clots in the brain’s blood vessels (cerebral venous thrombosis or dural sinus thrombosis)
- A tear in the outer layer of an artery in the neck (cervical artery dissection)
- Constrictive syndrome of the brain’s arteries that can resolve (reversible cerebral vasoconstrictive syndrome)
- Blood-filled tumors (hemorrhagic neoplasms)
- Abnormal connections between arteries and veins (arterio-venous malformations)
- Swelling of the protective membranes covering the brain and spinal cord (meningitis)
- A hematoma, or collection of blood, beneath the dura mater, the outermost layer covering the brain (acute subdural hematoma)
- Bleeding in an area of previous stroke (hemorrhagic infarct)
Doctors often use imaging studies, like CT scans or MRI, to accurately diagnose these conditions and rule them out.
What to expect with Hemorrhagic Stroke
Several factors indicate a poor prognosis in the context of a brain hemorrhage. These include entering a state of coma, having a large hematoma (a collection of blood, in this case in the brain) larger than 30ml, bleeding within the brain’s ventricles or in the back of the brain, being over 80 years old, having high blood sugar, and suffering from chronic kidney disease. Unfortunately, early deterioration and death are common issues with brain hemorrhages. Coma at the time of diagnosis indicates a particularly bad prognosis.
The American Stroke Association recommends that patients with a brain hemorrhage should be monitored and managed in a specialized stroke unit. Only about 20 percent of patients retain their independence six months after the incident. Those who survive may enter into a state of unresponsive wakefulness or locked-in syndrome, particularly if the damage is extensive or located in the brainstem.
A scoring system known as the ICH score, established by Hemphill et al., can help predict mortality following a brain hemorrhage. The score assigns points based on the state of the patient following a stroke. Variables include the patient’s mental status, age, location of the hemorrhage, size of the hematoma and the presence of intraventricular hemorrhage. The 30-day mortality rate increases drastically as the score increases, starting from 0% for score 0 and rising to 100% for scores 5 and 6.
Possible Complications When Diagnosed with Hemorrhagic Stroke
People with Intracerebral Hemorrhage (ICH) can experience several complications, including:
- Brain swelling (Cerebral edema)
- Increase in pressure within the brain (Increased intracranial pressure)
- Accumulation of fluid in the brain (Hydrocephalus)
- Seizures
- Blood clots in the veins (Venous thrombotic events)
- Increased blood sugar levels (Hyperglycemia)
- High blood pressure
- Fever, and infections
- Lung complications like pneumonia, difficulty in swallowing leading to aspiration, fluid in lungs (Pulmonary edema), failure in the function of the respiratory system, and distress in breathing. This happens in about one-third of the patients, especially women
- Heart problems, such as heart attack (myocardial infarction), irregular heartbeat (atrial fibrillation, ventricular fibrillation, ventricular tachycardia), heart damage due to severe emotional distress (stress-induced cardiomyopathy), and sudden heart failure. This occurs in about 4% of the patients.
Similar complications can occur in Subarachnoid Hemorrhage (SAH), such as:
- Narrowing of blood vessels (Vasospasm)
- Insufficient blood supply to the brain (Ischemia)
- New bleeding points (Rebleeding)
- Seizures
- Low sodium levels in the blood (Hyponatremia)
- Fluid accumulation in the brain (Hydrocephalus)
- Increase in fluid in the lungs, including the space around the lung tissue (interstitial) and in the air sacs (alveolar). This condition, referred to as Neurogenic Pulmonary Edema, commonly occurs in Subarachnoid Hemorrhage.
Preventing Hemorrhagic Stroke
There’s a risk that ICH (intracerebral hemorrhage) could happen again. High blood pressure and old age could increase this risk. To help prevent recurrence, it’s important to keep blood pressure under check. Changing certain lifestyle habits can also be beneficial, such as avoiding alcoholic drinks, smoking, and illegal drugs. Ongoing rehabilitation involving various health professionals is also recommended.
There are some factors that could possibly increase the risk of having another ICH. These include:
- The first ICH happening in a part of the brain called the lobe
- Being older in age
- Having small, usually harmless, bleedings detected by a type of brain scan called gradient echo MRI
- Currently taking anticoagulant medications (blood thinners)
- Having certain genetic variations (known as apolipoprotein E epsilon 2 or epsilon 4 alleles)