Overview of Aortic Valve Replacement
Your aortic valve is a special type of valve with three flaps, which is located where your heart’s lower left chamber, the left ventricle, connects to the large blood vessel known as the aorta. Its function is to ensure that blood flows in one direction: from the left ventricle to the aorta and from there to the rest of your body. This seemingly delicate valve, through the complex processes of cells and molecules, can endure the powerful forces present in every heartbeat.
But, the right function of the valve can be affected by factors such as aging and inborn defects leading to a variety of complications. For instance, although bicuspid aortic valves (BAV), a condition where the valve has only two flaps instead of three, are common, the range of defects you can be born with can vary widely. This includes a missing aortic valve or narrowed sections before or after it. BAV affects 1 to 2% of people, more commonly men. If the proteins needed for the valve formation are missing, this can result in two flaps fusing into one. This condition is often linked with problems in the aorta such as widening or a narrowing known as coarctation. Over time, the flaps of the bicuspid aortic valve can worsen due to abnormal forces.
These defects, including BAV, can cause various problems with the aortic valve like aortic stenosis (a narrowed valve hole) and aortic regurgitation (a valve that doesn’t close properly). This can make them more likely to get infected, a condition known as infective endocarditis. BAV can often stay without causing symptoms until you are 50 to 60 years old unless the valve damage is severe.
Aortic stenosis is a condition that happens when the aortic valve becomes narrow, resulting in an increased workload for the heart’s left ventricle. Its prevalence increases with age, affecting up to 4.6% of people over 75 years old. Around 3.5 million people in England are expected to have this condition by 2020. This condition is often caused by calcium build-up which makes the valve stiff and restricts its movement. The lining of the valve can also be damaged by increased physical stress. This is most common in the posterior leaflets, or back flaps. However, in developing countries, rheumatic fever, an illness that causes inflammation of the heart’s leaflets, is still the most common cause of aortic stenosis.
Some people with aortic stenosis might not have any symptoms or they may experience fainting, chest pain, and heart failure. Severe aortic stenosis can be life-threatening, with a 50% death rate at 2 years. Current guidelines from the American College of Cardiology and the American Heart Association (ACC/AHA) state that aortic stenosis is considered severe if the valve opening is less than 1.0 cm, the average gradient is greater than 40 mmHg, or the blood flow speed is greater than 4 m/s. If left untreated, those with symptoms or severe cases don’t have a good survival outlook unless their valve is replaced. However, many older people, around 30% of those aged over 75, do not have surgical valve replacement due to technical problems such as a hardening of the aorta, being too weak or ill for surgery, not wanting surgery, or serious other illnesses. There is a 10% risk of dying in the operation in patients with heart dysfunction, chronic kidney disease, and older age. Thankfully, a newer treatment option called Trans-catheter Aortic Valve Replacement or Trans-catheter Aortic Valve Implantation (TAVR/TAVI) is a safer method for patients unfit for surgery.
Aortic regurgitation, on the other hand, is when blood flows back into the heart from the aorta when the valve flaps don’t close properly. Common reasons for this include inborn defects, calcium build-up, infective endocarditis, rheumatic fever, and injury. Over time, the left ventricle grows larger to take the increased volume of blood in order to continue pumping the normal amount of blood with each heartbeat, and maintain normal pressure. Hence, aortic regurgitation can remain without symptoms for many years. However, in acute cases, the heart doesn’t have enough time to grow to accommodate the increased volume of blood. This causes the heart to beat faster to maintain blood flow, but it’s not enough, which results in increased pressure in the left atrium, fluid in the lungs and shock caused by heart problems.
The sound of a heart murmur in aortic regurgitation is high-pitched and decreasing, beginning shortly after the ‘lub’ sound of the heartbeat. While there are other murmurs linked to this condition, some include rapid pushing out of blood overload from the left ventricle, partial closure of the heart’s mitral valve due to backward blood flow from the aorta, and a murmur caused by the coming together of an aortic murmur with the third heart sound due to the left ventricle filling with blood at the same time from the left atrium and the backward blood flow.
Modern knowledge has helped us come a long way in heart valve surgery. In 1912, Dr. Theodore Tuffier used his finger to separate the fused flaps of a narrowed aortic valve. Since the 1960s, 70 different artificial heart valves have been created. These can be made from human or animal tissue, known as bioprosthetic valves, or mechanical valves, made from durable materials. Bioprosthetic valves function similarly to the natural ones but don’t last as long, whereas, mechanical valves are more long-lasting but require medicine to prevent blood clots. Doctors decide between the two based on factors like the patient’s age and overall health.
Anatomy and Physiology of Aortic Valve Replacement
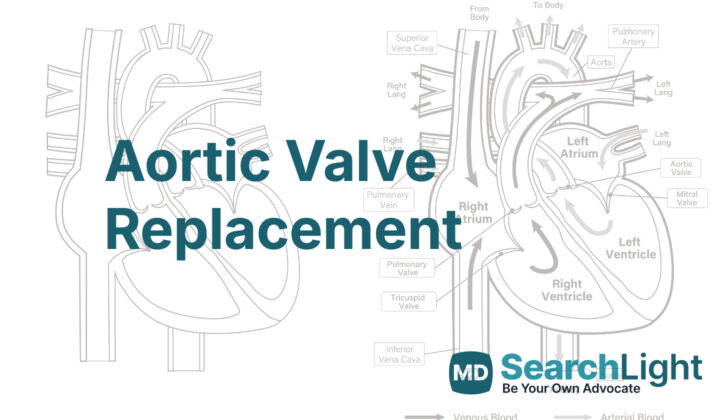
The heart is made up of four parts or “chambers” – the right atrium, right ventricle, left atrium, and left ventricle. It also has four valves that control how blood flows through these chambers. These valves are called the tricuspid, pulmonary, mitral, and aortic valves. The valves that sit between the atriums (upper chambers) and ventricles (lower chambers) of the heart are referred to as “atrioventricular” valves. These are the tricuspid and mitral valves. The valves that connect the ventricles to the arteries (large blood vessels that carry blood away from the heart) are named “arterioventricular” valves, which include the aortic and pulmonary valves.
The aortic and pulmonary valves are also called “semilunar” valves because they are shaped a bit like half-moons. Unlike semilunar valves, atrioventricular valves are connected to the heart muscle through tissue strands called papillary muscles and fibrous cords. This connection allows these valves to respond when the heart muscle, or myocardium, contracts. Although semilunar valves do not have such direct connections, they are not just passive structures. Research now shows that their complex design and cellular makeup is crucial for their proper function.
The aortic valve is one of these valves and its job is to let blood flow in one direction only – from the left ventricle into a major artery called the aorta. Amazingly, it can open and close more than 100,000 times a day, adding up to about 3.7 billion times in an entire lifetime. The aortic valve has three segments, also known as leaflets, and three spaces behind these leaflets, called sinuses. Two of these sinuses are openings for the right and left coronary arteries, blood vessels that supply the heart muscle with blood. These are named the right and left coronary sinuses. The third sinus does not connect to anything and is therefore termed the non-coronary or posterior sinus.
Why do People Need Aortic Valve Replacement
Valvular disease, a condition where the heart’s valves don’t open correctly, is really hard to prevent or delay with medical treatment. The best treatment is usually replacing the valve with surgery. A procedure called a balloon valvotomy may be performed to temporarily ease symptoms, but it isn’t meant to replace the need for surgery.
Valvular disease is classified according to several factors, including how much the affected valve can open (orifice area), the speed of blood flow, and the difference in blood pressure across the valve. An echocardiograph, a type of ultrasound, is typically used for this classification. However, sometimes it may overestimate how severe the condition is, which could lead to unnecessary treatment.
Thankfully, the increasing success of Transcatheter Aortic Valve Replacement (TAVR) has changed the guidelines for treating this condition. TAVR is now the recommended treatment in certain cases, such as for patients who might not survive traditional surgery or those considered to be at high risk.
Traditional Aortic Valve Replacement (AVR) surgery carries a risk, with a mortality rate of 2.8%, and it is not suitable for everyone. For example, some elderly patients with severe valvular disease aren’t good candidates for AVR. Similarly, children and newborns may require frequent replacement surgeries as they grow, and currently available mechanical valves can be too big for them.
TAVR offers numerous advantages. For example, it can be performed without the need for open-heart surgery, which is a major breakthrough for patients who were previously considered too high-risk for surgery. Successful TAVR procedures are also very high, with approximately 92% of cases deemed successful. However, TAVR isn’t without potential complications, which can include leaks around the implanted valve, movement of the implanted valve, abnormal heart rhythms, and stroke.
Some potential complications of TAVR are managed through techniques like post-dilation, careful selection of valve size, and the use of newer valve designs. Performing a follow-up CT scan on all TAVR patients is also typically required to look for signs of possible problems with the movement of the implanted valve leaflets (bits of the valve that open and close to control blood flow).
In conclusion, AVR and TAVR are both techniques used to manage valvular disease. They each have their own pros and cons, and the choice of technique is usually determined based on the patient’s individual clinical situation and risk factors.
What Else Should I Know About Aortic Valve Replacement?
Replacing the aortic valve is a procedure that can save lives. The aortic valve is a key part of your heart, but it can have problems. Sometimes it can become leaky, which is known as “aortic insufficiency.” Other times, it can become partially blocked or narrowed – a condition called “aortic stenosis.”
There are several ways to fix these problems. One option is a sternotomy, which is a type of surgery where they open your chest. Another is minimally invasive cardiac surgery, where they make a smaller cut and use special tools to perform the surgery. There’s also a procedure called transcatheter aortic valve replacement, which is where they replace your aortic valve through a small tube (or catheter) inserted into a blood vessel.