Overview of Open Heart Massage
Cardiopulmonary resuscitation (CPR, a process to maintain blood flow to the heart and brain during cardiac arrest) is a widely studied and standardized medical procedure. Despite years of research, updated guidelines, and dedication by professionals worldwide, the survival rate for people who have cardiac arrest has not improved much. Today, only about 1 in 10 people survive and can leave the hospital after cardiac arrest.
Before the introduction of CPR with chest compressions in the early 1960s, open cardiac massage (OCM, a method of directly massaging the heart) was often used for cardiac arrest. OCM is typically performed in patients who are not responding to other treatments for severe chest trauma, or after cardiac arrest following chest surgery.
OCM was first described by Moritz Schiff, a 19th-century researcher, in lab animals after their heart function had stopped. The first use of OCM on a human was in 1880 by Niehans. The first successful use of OCM to address cardiac arrest was by Kristian Ingelsrud in 1901. By the 1920s, the technique was widely used. The preferred method for addressing cardiovascular collapse through the 20th century was OCM, especially after a reported overall survival rate of 25% across 99 cases.
In situations where a trauma patient arrives at a hospital in cardiac arrest, a last-minute measure called emergency resuscitative thoracotomy (ERT) is used. This involves OCM and placing a clamp on the aorta, which is the main blood vessel that leaves the heart. The goal of OCM in this setting is to restore proper blood flow to the heart and help the heart start beating again on its own. The clamp also plays a part in directing blood flow to the brain and the heart and can stop any bleeding in the section of the body below the diaphragm.
The survival rates following ERT with OCM are unfortunately quite low. Just around 15% survive after a penetrating trauma and only 1% to 2% after an impact trauma. Even if the heart starts beating again, the outcomes are often not good. Only about 27% of these patients wake up within 28 days. Half of the patients who regain heart function don’t survive to leave the hospital. The leading cause of death and disability is a brain injury from lack of oxygen, underscoring how important it is to stabilize the heart and lung functions and protect the brain during resuscitation after a trauma.
Anatomy and Physiology of Open Heart Massage
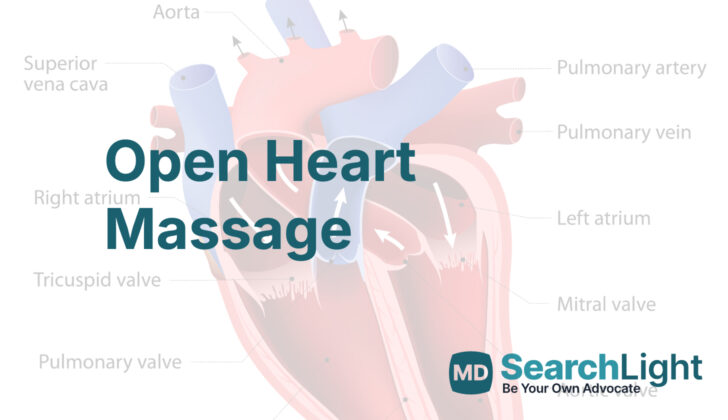
The Open Chest Massage (OCM) is a special heart-related procedure that needs a deep understanding of the anatomy around the chest area. In this procedure, the surgeon first makes a cut on the left side of the chest. The lungs are carefully put to the side to keep the operating area clear. Then, the surgeon gets access to the heart by cutting or clipping the breastbone. To gain full access to the heart, the protective covering of the heart, called the pericardium, is cut open. This procedure is also used to relieve pressure in cases of cardiac tamponade, a condition where pressure builds up around the heart and affects its function.
The surgeon must be careful during this process not to hurt the phrenic and intercostal nerves – located in the chest, and to avoid injuring blood vessels that are crucial for blood supply in the chest. Once the surgeon is inside the protective covering of the heart, they apply pressure on the left ventricle (one of the main pumping chambers of the heart) while making sure that the coronary arteries (vessels supplying blood to the heart muscle) are preserved to keep oxygen delivery to the heart muscles. As part of this procedure, the surgeon has to identify and separate the aorta (major blood vessel supplying oxygenated blood to the body) from the esophagus (food pipe) so that the aorta can be cross-clamped. Cross-clamping is a method that directs blood flow to the brain and heart.
Being able to thoroughly understand this complex anatomy helps the surgeon to perform effective procedures, prevent injuries caused unintentionally by medical treatment, and manage any complications that may arise. All of this contributes to better results for the patient.
This procedure may be monitored by looking at the level of end-tidal carbon dioxide (EtCO2) which is a waste product of body metabolism. Its presence shows that cells in our body are continuing to function because they’re getting enough oxygen. More comprehensive studies have shown that OCM often work better than some other resuscitation methods, especially in cases of traumatic cardiac arrest and in the operating room setting. OCM allows direct manual heart compression, which results in better blood flow to the heart and brain. Closed-chest compressions sometimes do not deliver the required blood flow especially in patients with chest injuries.
Different studies conducted over the years also support the fact that OCM is a more effective way of doing heart resuscitations. In a 1962 study conducted by Weale and team, they discovered that another method known as “closed-chest cardiac massage” was less effective. They recommended OCM over this. Robert Bartlet conducted another study in 1984 that compared three types of cardiac massage and found heart compression using OCM to be most effective. Another study by Artur Sanders and colleagues compared blood flow in the heart vessels during two methods of resuscitation and found OCM to have better outcomes.
In conclusion, OCM has been seen to provide better blood flow and oxygen supply to important organs such as the heart and brain, leading to better survival rates and recovery for the patient.
Why do People Need Open Heart Massage
When someone suffers a heart attack due to severe bleeding — whether from an injury or another cause — traditional chest compressions or CPR can actually make things worse. Not only does this increase the force of the heart’s pumping, possibly making the bleeding worse, it can also create further physical injury. Regular CPR isn’t usually suitable for heart attacks caused by severe bleeding or serious injuries to the blood vessels in the chest or stomach. In these instances, immediate transport to a hospital for Emergency Room Thoracotomy (ERT), a surgical procedure that involves opening the chest cavity, is often required.
According to medical guidelines from the American Heart Association, Eastern Association for the Surgery of Trauma, and the International Liaison Committee on Resuscitation, in certain cases where the heart has stopped due to a severe injury, a procedure called Open Chest Massage (OCM) might be used. ERT and methods such as thoracic aortic cross-clamping can be lifesaving in these critical circumstances because it allows doctors to control the bleeding.
In situations where there has been a severe injury to the chest and the heart has stopped, ERT with OCM can be successful up to 30 minutes after the heart has stopped, with survival rates of 10% to 15% and up to 20% for stab wounds. Additional situations that may require OCM include cardiac arrest following recent heart surgery and decompression of pericardial tamponade, a condition where fluid builds up in the sac around the heart and limits its ability to pump blood. OCM might also be recommended if standard advanced life support protocols don’t restore regular heart beat within 5 to 10 minutes. Other potential reasons for it being used include an abnormal chest wall anatomy that prevents effective chest compressions, a stubborn case of irregular heart rhythm, and a massive air embolism.
For severe injuries outside of the chest, like those involving the large blood vessels in the leg or serious trauma to the neck, death can occur within 5 to 10 minutes. In these cases, an ERT provides direct access to control the source of the bleeding, perform OCM, and quickly restore blood flow through a central vein or directly into the upper heart chambers. However, for cardiac arrest due to blunt trauma, an ERT is only effective if the patient arrives at the hospital within 10 minutes of the witnessed arrest and is receiving breathing support, or within 5 minutes if they are not receiving breathing support. Beyond these timeframes, the procedure often fails, with survival rates of only about 0.2% for blunt trauma cases.
When a Person Should Avoid Open Heart Massage
ERT (Emergency Room Thoracotomy) and OCM (Open Chest Massage) are serious medical procedures typically used in severe cases of a heart stopping due to injury, or extremely low blood pressure caused by serious bleeding, where there’s a reasonable chance of the patient surviving. There might be some reasons why these procedures cannot be done. For instance, OCM cannot be done if a person’s heart is still beating.
Other important reasons not to progress with these procedures involve a patient’s health wishes that exclude any revival attempts like a “do not try to revive” rule, or if a person shows no signs of life upon reaching the hospital. Patients suffering from an injury and not showing any heart activity or responses from the pupils (part of the eye that reacts to light) are not typically considered for ERT and OCM. This is due to their extremely small chance of survival, and the careful use of medical resources.
There are also other special cases where these procedures are not performed. For example, if a patient was unconscious or showed no signs of life for a long period before reaching the hospital, these procedures might not be recommended because recovering normal brain function is unlikely. The effectiveness of ERT for trauma patients is generally tied to how quickly the procedure can be performed after cardiac arrest. If injuries are severe and irreversible—like serious brain damage, heart damage, or damage to major blood vessels—or involve other fatal trauma, these procedures are not recommended. ERT and OCM are also generally avoided in patients with serious pre-existing conditions that would limit their chances of survival, even if blood flow could be restarted (ROSC, Return Of Spontaneous Circulation). In severe instances of blood loss, such as extensive chest or stomach bleeding, these procedures may not be practical if the necessary resources and surgical abilities to address the bleeding aren’t available.
Equipment used for Open Heart Massage
An Emergency Room Thoracotomy (ERT) is a medical procedure that involves a quick access to your chest area to aid in severe situations such as a heart stoppage due to trauma. It’s crucial that they have all the necessary tools on hand. Here’s what’s usually included in such a setup:
* Clean surgical tools like
* Rib spreader (tools like Finochietto or Tuffier retractors are employed to create more space between the ribs)
* Scalpel and blades (for cutting)
* Heavy scissors (like Mayo or trauma scissors)
* Large needle and special thread (like 3-0 or 4-0 polypropylene used for mending the heart)
* Hemostats and large clamps for controlling blood flow (for example, Satinsky or DeBakey vascular clamps)
* Thoracotomy tools (specific tools for opening the chest)
* Tools for cutting ribs like rib shears, heavy scissors, or Gigli saw
* A suction device with enough tubing to clear blood and other fluids
* Tools for control of bleeding
* Vascular tourniquets (used to stop the flow of blood)
* Large cotton sponges or pads for operations
* Protective dressings
* Instruments for blocking blood flow in the aorta like a cross-clamp or aortic occlusion clamp for separating the descending aorta (often a Fogarty or Satinsky clamp)
* Necessary supplies for the chest drain kit with tubes for removing excess fluid if needed
* Internal heart shocker paddles (used if the heart needs to be shocked from within)
* Drugs for resuscitation like Epinephrine for direct heart or intravenous (IV) injection
* Monitoring and airway equipment
* Endotracheal intubation kit (for example, a tool to view the airway, laryngoscope, and tube to maintain an open airway, endotracheal tube)
* Suction catheter and suction unit for clearing airways or blood
* Personal protective equipment
* Gown, gloves, mask, and eye protection for everyone in the room to reduce contact with bloodborne pathogens during the opening of the chest
Who is needed to perform Open Heart Massage?
An Off-Pump Coronary Artery Bypass (OCM) is a serious surgery that needs to be done very quickly in an operating room. It requires a team of extremely skilled medical staff, each with a specific role, working together to ensure the best possible result for the patient. This crucial team normally includes:
- A specialist surgeon who is experienced in trauma or heart (cardiothoracic) surgery
- An anesthesiologist to manage your pain and consciousness during the surgery
- A surgical assistant to aid the surgeon during the procedure
- A scrub nurse or surgical technologist who handles the surgical tools
- A circulating nurse moving around the room to provide necessary supplies and assist as needed
When an OCM needs to be done urgently in the emergency room, the team is made up of fewer specialized members aimed at performing a rapid, life-saving medical procedure. The emergency team typically includes:
- A trauma surgeon or Emergency Room (ER) doctor
- A nurse specialized in emergency or trauma care
- An anesthesiologist if available to manage your pain and consciousness
- A respiratory therapist if available to aid with your breathing
- An ER technician or circulating nurse to provide necessary supplies and assist as needed
- Support staff to communicate with the blood bank and lab
Preparing for Open Heart Massage
In emergency situations where immediate medical attention is needed, it may not be practical for doctors to get permission from a patient before starting treatment. This is allowed because these actions are needed to save the patient’s life. However, as soon as they can, doctors should check any documents the patient might have that tells them what care the patient does or does not want. This could be a document telling doctors not to restart their heart if it stops beating. Checking these documents is an important legal requirement and ensures that a patient’s wishes are respected.
When a patient needs immediate care, everything moves quickly and everyone involved in the patient’s care needs to be well prepared and communicate effectively. Here are some of the necessary steps:
First, every team member needs to understand their role. The person in charge, usually a surgeon, coordinates everyone. Other team members, such as nurses and anesthesia providers, each have their own tasks which could include managing the patient’s breathing, monitoring their condition, or providing the necessary blood products.
The next step is to gather all the necessary equipment and medication. Fast access to sterile instruments is critical, along with sutures (long, thin pieces of material used to sew body tissues together), hemostatic agents (medication that stops bleeding), and other medications. Having immediate access to blood products, fluids, and emergency drugs is also important.
Patients are usually positioned face up, allowing the team to access the chest area. Often, due to the urgency, full sterilization procedures aren’t possible, so a quick application of a skin cleanser is used instead. The patient’s breathway is kept open so they can receive enough oxygen and a skilled doctor or nurse manages this.
Doctors continuously monitor the patient’s vital signs to keep real time updates on their condition. They also set up good access for giving IV fluids, drugs and blood products. Specialized lines might be put in to give even more detailed information about the patient’s condition. Immediate communication with the blood bank ensures that blood products for transfusion are readily available, as many patients needing this type of care lose a lot of blood. The lab team is also on standby to quickly run important tests.
Finally, if a patient becomes stable, they can be moved to an operating room for more specialized care. The surgical team can then take over patient resuscitation in a more controlled environment.
How is Open Heart Massage performed
Accessing the heart is usually done through surgery on the left side of your chest. This can be done very quickly, under a minute, if there’s a trained team present. An experienced heart surgeon is usually preferred for this technique as they are trained to do such surgeries in under 2 minutes. It might take a non-specialist surgeon slightly longer, about 2-3 minutes, to do the procedure.
There are three primary ways to reach the heart when a patient requires ongoing chest compressions (OCM), which are described below:
Left Anterolateral Thoracotomy
In this method, the patient lays flat on their back or slightly on their left side, and if there’s time, the left arm is raised. A cut is made on the left side of the chest along the space between the fourth or fifth ribs, extending from the sternum (midline of the chest) to the side. The surgeon uses retractors (medical tools to hold the cut open) to separate the ribs carefully. The surgeon may also need to tie off the internal mammary artery (a blood vessel that supplies blood to the chest) to get better access and move the left lung aside. The pericardium, a protective sac around the heart, is opened carefully, ensuring not to harm any surrounding nerves. Once the heart is exposed, the surgeon performs OCM, a medical term for manually compressing the heart. If necessary, a clamp might be placed on the descending thoracic aorta (the large artery leading from the heart) to stop further bleeding and improve heart function.
Bilateral Anterior Thoracotomy Approach (Clamshell)
The patient lies flat on their back with both arms extended and secured. The incision is made from one side of the chest to the other, along the midline, across the fourth or fifth intercostal space. The sternum is divided horizontally, usually using heavy scissors or a special saw, to provide a wide view of the chest. After the cut, rib retractors are used to widen the gap beteeen the ribs, providing broad visibility to the thoracic cavity. Both lungs are gently moved aside to allow better visibility for the subsequent steps. The pericardium is cut in the middle to access the heart and avoid injury to the nerves around it. Once the heart is visible, OCM is performed.
Median Sternotomy
In this method, the patient lies flat on their back with both arms extended. A midline incision is made directly over the sternum (the breastbone). Access to the sternum is achieved using a saw or shears to split the breastbone lengthways. This requires precision to avoid damaging underlying structures. A retractor is used to separate the two halves of the sternum, providing full visibility to the area around the heart. Retraction of the lungs and other tissues is performed to provide a clear field for accessing the heart. The pericardium is then cut in the middle, and the cut edges are pulled aside for better visibility. Once the heart is exposed, OCM is performed.
Performing OCM effectively requires careful techniques to restore circulation while minimizing any damage to the heart. The two main methods used for this are the 2-handed and single-hand techniques:
OCM Techniques
In the 2-handed technique, one flat hand is placed underneath the heart, and the other on the top of the heart. The heart is then gently squeezed from the bottom to the top, about 100 times per minute, aligning with standard guidelines. This method requires the use of the flat hands, not the fingertips, as they increase the risk of injuring the heart. Alternatively, a single-hand technique can be employed if the doctor’s hand is large enough. In this approach, the doctor’s fingers are positioned on the bottom of the heart, with the thumb on the top. It’s important that the heart is kept horizontally during OCM; lifting it could interfere with its function. Additionally, an assistant may compress the descending aorta to improve blood flow to the coronary arteries and the brain.
If the patient’s heart starts beating again on its own, the cut is covered with sterile, saline-dampened gauze, and antibiotics targeting skin bacteria are administered. Ideally, the cut should be closed by a heart surgeon as soon as possible.
Possible Complications of Open Heart Massage
Open chest massage (OCM) is a complex medical procedure usually done as part of emergency resuscitation therapy (ERT). This operation carries significant risks similar to other chest-opening surgeries. For example, it might injure various areas like the minor blood vessels between your ribs (intercostal vessels), the nerves in your lungs, the sac that contains your heart (pericardium), and the muscles in your heart. There’s also a risk that major vessels like your internal chest vein, lung veins, and heart vessels become injured, leading to severe bleeding.
Another concern is pneumothorax, which can occur if lung tissue gets damaged during surgery. This is a condition where air leaks into the space between your lungs and chest wall. After open chest massage, a number of complications are possible, like wound infections or heart injuries. In fact, post-surgery wound infection rates may be as high as 9.1%, and mechanical damage to the heart was found in up to 1.4% of cases.
A 2011 study of 123 OCM procedures showed that more than half were unlikely to benefit the patient due to a poor chance of survival. Despite temporarily reviving some patients, all of these individuals eventually passed away in the intensive care unit. This research underscores the importance of carefully selecting patients for such procedures to avoid unnecessary interventions.
Since OCM is quite invasive, neighboring structures like nerves around your lungs and ribcage, and various blood vessels, are prone to injury. Direct manipulation could also lead to heart damage, increasing complications. For cases needing clot-dissolving therapy due to complications like a large lung clot or stroke, OCM can make things more complex as the cut made during surgery could cause more issues. In these circumstances, other treatment methods should be considered.
Even if a patient recovers from the procedure, there’s still a high risk of infection as emergency chest-opening surgeries may not follow the full set of sanitary practices. Hence, managing the surgical wound and aftercare are crucial to reducing the risk of severe infections.
Lastly, there’s a risk of brain-related problems after OCM, particularly if blood flow to the brain is compromised. This could lead to poor mental outcomes, even if circulation is revived. Current revival methods may not be sufficient to prevent this, so new techniques that target blood flow to the brain must be explored. While OCM can save lives, it does have a range of complications that need careful handling to optimize patient recovery.
What Else Should I Know About Open Heart Massage?
Open chest massage (OCM) is a crucial emergency procedure, often used for serious trauma and cardiac arrests. It’s particularly useful in situations where regular chest compressions aren’t working well enough. In the past, before we began to use the less invasive closed-chest compressions, doctors mainly used OCM to keep the blood circulating when a patient’s heart stopped.
Some research suggests that OCM may be better at maintaining circulation than regular compressions. For instance, a study done in 1953 found that 28% of patients who received OCM recovered. And further research showed that if a doctor performed OCM within four minutes of the heart stopping, up to 58% of patients recovered and were often in good mental health afterwards. But more recent studies have shown mixed results.
One new method that researchers are looking into involves going through the diaphragm to perform OCM during surgery. They tried this method on 6 patients who went into cardiac arrest during operations (4 of them were getting liver transplants, and 2 were trauma cases). By making an incision in the diaphragm and reaching the heart that way, they managed to bring 3 patients back to a healthy heart rhythm, 2 of whom survived the transfer to the intensive care unit, and 1 eventually got out of the hospital.
While OCM has its limitations because of how invasive it is and the associated risks, including potential damage to the chest and an increased chance of infection, it can ultimately be a lifesaver in the right situations—like when a patient needs quick surgical intervention.
Studies suggest that OCM could be very beneficial in certain specific conditions, especially when applied early and by experienced surgical teams.