Overview of Sclerotherapy
Sclerotherapy is a type of treatment that involves injecting certain substances into a blood vessel. These substances, known as sclerosing agents, cause irritation, damage to the vessel lining, inflammation, and finally the destruction of the vessel. This process is also known as endofibrosis. There are different types of sclerosing agents, which can include glycerin and hypertonic saline, polidocanol and sodium tetradecyl sulfate (STS), and iodinated substances.
This type of therapy is often used to treat problems with the veins, particularly varicose veins (large, bulging veins) in the lower legs. It can be a primary treatment or a complementary treatment to help with bothersome or painful veins. In some cases, it can also be used as a treatment for certain types of hemorrhoids (swollen veins in the rectum and anus).
For superficial varicose veins, reticular veins (small, bluish veins), and telangiectasia (clusters of tiny, dilated blood vessels), Sclerotherapy remains the top-tier treatment option.
The concept of treating problems with the veins dates back to ancient times, to physicians like Galen, Celsus, and Hippocrates. Modern-day sclerotherapy as we know it first emerged in the 1850s. Unfortunately, the early versions of this treatment had high infection rates. So, it was put on hold until the early 1900s when hypertonic saline was introduced as a sclerosing agent. Finally, the 1940s saw the arrival of STS as a sclerosing agent, marking the beginning of the modern era of sclerotherapy.
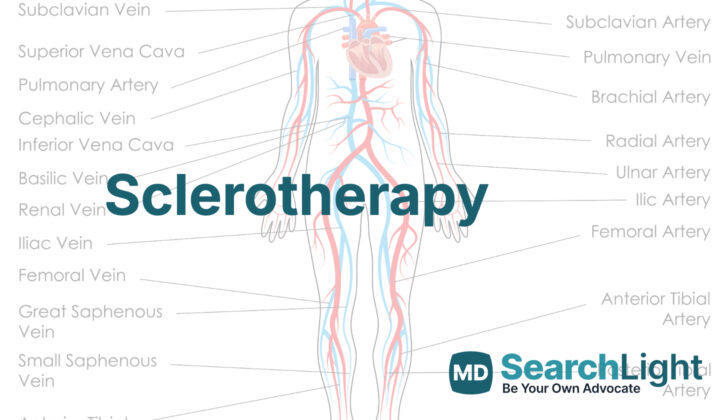
Anatomy and Physiology of Sclerotherapy
Varicose veins are large, twisted veins that often appear beneath the skin, causing the limbs to look bumpy. They’re usually located in the lower legs and can cause discomfort like itching, pain, swelling, and a heavy feeling. In some cases, they can even cause bleeding. Varicose veins are quite common, affecting around one-third of the population, with women being more likely to have them than men. The chances of developing them increase as we age.
These pulled, swelled veins usually happen because of problems with blood flow in the veins located under the skin or those deeper in the leg. When these veins don’t work properly, they can cause varicose veins that we see on the surface, or they can lead to swelling in the legs and changes in skin color and texture.
A strong family history is the most significant factor that makes one likely to develop varicose veins. However, anything that increases pressure in the abdomen and makes it difficult for blood to flow back to the heart, such as obesity, constipation, pregnancy, standing for long periods, and taking estrogen and progesterone can all contribute to the development of varicose veins. Varicose veins can even occur due to a reaction to sunlight or radiation damage.
Almost all of the blood drainage in the lower legs happens through the deep veins. Sometimes, the veins in this system don’t work properly, like if the valves fail to stop blood from flowing backwards. This can increase pressure on the veins nearer to the surface of the skin and increase the chance of developing varicose veins. The walls and valves of these veins become weakened due to an increase in collagen and a decrease in elastin, which is a protein that gives tissue its elasticity, and can become stretched out under increased pressure, especially when standing or walking.
Varicose veins are larger than 4 to 5 mm in diameter; reticular veins are smaller, measuring 1 to 4mm. There are also bluish branching veins, called telangiectasias, and reddish veins that are less than 1mm in size, known as spider veins.
Telangiectasias and varicose veins are signs of an issue in the vein system characterized by blood flow moving in the wrong direction, which leads to pressure build-up in the veins, increased vein diameter, and resulted in insufficient valves. This pressure leads to enlargement of the superficial veins and causes the small spider-like veins to grow. The increased pressure in the veins near the skin that happens when we move our lower limbs gets transmitted to these veins due to connections with the deep vein system.
Treatment of these veins might include medical therapies, changes in lifestyle like exercise to help muscles in the legs work better, weight loss to reduce pressure in the veins, elevating the limbs, and wearing compression garments. When treatment is necessary, it is determined based on the severity of the issue, with the options including surgical intervention like vein removal or tying off, minimally invasive procedures that use heat to damage the veins, or non-surgical treatments.
Below is a table explaining the stages of venous insufficiency:
CEAP Classification
- C1: Spider or reticular veins, treatment is usually for cosmetic reasons
- C2a: Varicose veins without symptoms
- C2b: Varicose veins with symptoms like itching, pain, clotting, or bleeding
- C3: Leg swelling due to varicose veins
- C4: Changes in skin such as hardening or darkening
- C5: Healed vein ulcers
- C6: Active vein ulcers
The most common treatments typically involve an agent called a sclerosant, which damages the veins’ lining and underlying tissue. It works through direct cell damage or disruption of connections between cells. The most commonly used ones are hypertonic saline, a very salty solution, and detergents like STS and polidocanol.
A technique involving the use of foam sclerosants, wherein air-based foam is generated and mixed with the sclerosant to be injected into the veins, is gaining popularity. The foam formulation increases the efficacy of the sclerosant by allowing it to stay in contact with the vein walls for longer and over a larger area without being diluted in the blood. Foam also causes the veins to contract, which makes the vein walls come together, assisting in complete closure of the vein.
Why do People Need Sclerotherapy
Sclerotherapy is a treatment method used for treating swollen veins known as varicosities, and certain types of hemorrhoids. Different substances called sclerosants are used for this purpose.
This therapy can be administered as a liquid or foam, and is used for treating unsightly or bothersome swollen veins, including varicose veins, spider veins, reticular veins, and small red skin blemishes known as telangiectasias. Doctors also use sclerotherapy for treating reflux or backward flow in the saphenous vein (a large vein running along the inner side of the leg), enlarged offshoot and connecting veins, and deformities in the blood vessels.
A study of foam sclerotherapy for treatment of venous ulcers or vein insufficiency in the stages C5-C6 showed that it might be more effective than just compression therapy. However, more research is needed since the reviewed studies varied significantly.
Using ultrasound guidance during sclerotherapy for vein insufficiency is an efficient, targeted way to treat deep vein insufficiency. Studies have shown very high patient satisfaction with this method. One study reported 100% patient satisfaction, and over 90% reported improved life quality and physical appearance of the treated limb. This method is especially useful with patients with obesity, those with great saphenous vein insufficiency, and those who have other health conditions that make surgery too risky.
Sclerotherapy is also used to treat hemorrhoids, particularly for patients who are bleeding, at risk of major bleeding, or who have HIV or AIDS. Phenol in almond oil and 3% polidocanol are recommended for treating grades 1 through 3 hemorrhoids. For treating grades 2 through 4 hemorrhoids, the recommended treatments include Aluminum Potassium Sulfate and Tannic Acid (ALTA).
When a Person Should Avoid Sclerotherapy
There are certain reasons why a person might not be able to undergo sclerotherapy, a procedure to treat enlarged veins or varicose veins. Depending on these reasons, these people might have to consider other treatment methods, such as stab phlebectomy, which is another way of removing varicose veins.
People cannot have sclerotherapy if they have specific allergic reactions to the substances (sclerosants) used in the treatment, if they have a current infection in their body or specific to the area to be treated, or if they previously had conditions like deep vein blood clots, severe peripheral arterial disease (narrowing of arteries), severe collagen vascular diseases (diseases that affect your connective tissues), or heart or brain complications following injection of a sclerosant. These are known as absolute contraindications.
In other situations, sclerotherapy may still be possible, but with caution. For example, people who have difficulty moving around, have a history of severe allergies, have asthma, have significant issues with deep veins, or have thrombophilia (a condition that increases blood clot chances), may only undergo the procedure with care. Also, those who are currently pregnant or breastfeeding might be advised not to have sclerotherapy. There are occasions where “foam” sclerotherapy has caused visual disturbances and brief losses of sufficient blood supply to the brain in patients with a pre-existing heart condition known as patent foramen ovale where a small hole exists in the heart. Larger varicose veins may also make sclerotherapy risky as it increases chances of veins reopening.
When it comes to sclerotherapy for hemorrhoids (swollen veins in the lower part of the rectum and anus), this treatment is not suitable for people with blood clots in the hemorrhoids, a personal history of asthma, specific allergies to the substances (sclerosants) used in the treatment, thrombophilia, inflammatory bowel disease, and heart, kidney, or liver problems.
Equipment used for Sclerotherapy
To carry out a procedure known as sclerotherapy, the doctor will need the following tools:
- A very thin needle, about 30-gauge or even smaller
- Several 5-mL syringes
- The type of sclerosant that the doctor has chosen (this is a special medication that is used to close off the unwanted vein)
- A local anesthetic to numb the area where the procedure will be done
- Gauze dressings to cover the area after the procedure
- Compressive bandages to apply pressure to the area after the procedure
- An ultrasound machine, if the doctor is doing a type of sclerotherapy that is guided by ultrasound (this type of machine uses sound waves to create a picture of the inside of your body and can help the doctor to see exactly where to inject the sclerosant)
Who is needed to perform Sclerotherapy?
If you’re going to have sclerotherapy (a treatment to remove veins) done in a doctor’s office, typically the team will be a clinician (a doctor or nurse who has been trained in this procedure) and an assistant.
However, if this treatment is done in a hospital, usually as part of a bigger procedure, the team will include a clinician skilled in sclerotherapy, a surgical technician or nurse that works in the operating room, another nurse that helps keep the operating room running smoothly (called a circulating or operating room nurse), and staff that will ensure you don’t feel any pain during the procedure (anesthesia personnel).
Preparing for Sclerotherapy
Before going through a procedure, the patient and the main doctor should discuss and understand the potential outcomes. There may be some unwanted effects and the risk of issues like skin color changes and the appearance of small, widened blood vessels (often referred to as hyperpigmentation and telangiectatic matting). These risks are higher if the patient is taking certain medications like combined oral contraceptives, disulfiram, or minocycline.
The procedure usually known as sclerotherapy, is typically carried out with the patient lying down or seated. This depends on what gives the best view of the blood vessels being targeted. The areas for the procedure are cleaned and covered in a sterile way for hygiene. If an ultrasound machine is used for guidance, the machine is set to ‘vascular mode’. The chemical substances used in the therapy, known as detergent sclerosants, are made into foam with air using certain techniques (like the Tessari or double-syringe technique). This image shows how the Tessari technique works.
How is Sclerotherapy performed
The procedure of injecting a sclerosant, often used to treat varicose veins, involves a step-by-step approach. It starts from the largest veins going towards the smallest ones. It’s done this way to ensure that the medicine (sclerosant) flows correctly from where it’s injected to the other veins that need treatment. The goal is to treat all the affected veins in one leg at a time to prevent the veins from reopening or darkening of the skin due to the leakage of red blood cells from the treated vein.
A small needle, 30-gauge size or even smaller, is used to insert into the target vein. The doctor will make sure that the needle is in the right place inside the vein by withdrawing some blood. Once confirmed, the doctor will inject enough of the medicine to replace the blood in the vein. To treat smaller veins (reticular veins), vein networks (spider veins), and tiny blood vessels (telangiectasias), the doctor will inject the right amount of medication to make the vein wall whiten (blanching), and it’s a sign that the treatment was successful.
It’s important to use the smallest possible amount and concentration of medication for the injection to reduce the risk of new tiny blood vessels forming around the treated area.
After the injection, patients will need to stay lying down or seated for a few minutes. The treated leg will then be wrapped with a bandage or fitted with a compression stocking, which should not be removed for a week. This helps to put pressure on the treated veins. Applying pressure right after the treatment helps to prevent blood clots. Furthermore, patients will be encouraged to walk around while wearing this compression wrap or garment to enhance the recovery process.
Possible Complications of Sclerotherapy
Sclerotherapy is a treatment commonly used for varicose veins, but like any treatment, it may bring about some side effects. Locally, where the treatment is applied, you might experience discomfort during or after the injection, redness, swelling, itchiness, sores, increased hair growth, or small, fine red veins appearing in the treated area. These local effects are particularly frequent when the substances used for the treatment are HTS and glycerin. Additionally, around 30% of patients might notice skin darkening in the treated area roughly 6 to 8 weeks after the treatment due to an accumulation of a substance called hemosiderin. The darkening is more common when the treatment focuses on superficial veins and when higher concentrations of the substance called polidocanol are used.
There can also be effects that are felt systemically, throughout the body. These can include chest tightness, visual disturbances, temporary blockages in the brain’s blood flow (transient ischemic attacks), dizziness, or migraine headaches. If you have a history of migraines, you may be more susceptible to these headaches. These systemic side effects are more common when deeper veins are unintentionally treated, especially under ultrasound guidance.
It’s possible that after the treatment the target vein isn’t completely destroyed and could reopen, requiring further treatments. Wearing compression stockings or devices on the treated limb can aid in its healing and reduce the risk of the vein reopening.
The substances HTS and glycerin that are used in the treatment carry a higher risk of causing damage or sores to the surrounding tissues if they leak out of the vein or are mistakenly injected into a tiny artery. If these substances are injected into an artery, it can lead to a serious condition called acute limb ischemia that might require amputation. Glycerin can also cause slight blood in urine, although this can be lessened by adding chromated alum to the glycerin, which also makes it more effective.
If you’re having sclerotherapy for hemorrhoids, the most common complication is a simple localized infection that can be easily treated. However, improper or excessive use of the injectable solution could lead to serious infections and damage to the surrounding tissues.
What Else Should I Know About Sclerotherapy?
Sclerotherapy is a treatment method that doctors use for issues with your veins, specifically for problems like varicose veins (large, swollen veins), spider veins (small, damaged veins), and telangiectasia (tiny blood vessels visible on the skin). This procedure is relatively simple and doesn’t require surgery, making it a good option for people who are either not candidates for, or are worried about, surgical procedures.
During sclerotherapy, your doctor injects a solution into the affected veins, which causes them to shrink and eventually go away. The procedure is usually done on an outpatient basis, meaning you can go home on the same day, and doesn’t require a long recovery time.
One of the main advantages of this method is that not only does it improve the look of your veins (making you feel better about your appearance), but it can also help with symptoms caused by unhealthy veins, such as discomfort, swelling, and pain. This makes sclerotherapy a great choice for people with vein problems looking to improve their overall quality of life and vascular health.
Recent advances in the materials used for the procedure and how it’s carried out have made sclerotherapy safer and more effective. These improvements have led to the treatment becoming a common method for managing unhealthy veins.