What is Ectopic Pregnancy?
Ectopic pregnancy is a common complication during pregnancy, and it can lead to serious health issues, even death, if not identified and treated quickly. Doctors should always be alert to the possibility of an ectopic pregnancy in their patients who are pregnant. These patients may complain about pain, vaginal bleeding, or less specific symptoms like nausea and vomiting.
For a successful pregnancy to occur in the womb, there’s a complex process that involves chemical reactions, hormonal changes, and certain physical conditions. While I won’t discuss all these elements in detail, it’s important to understand how the different parts of the female reproductive system – ovaries, fallopian tubes, egg, sperm, and uterus – play a role in our discussion.
Located on both sides of your uterus in your lower pelvic area, the ovaries are the organs in the female body responsible for releasing an egg each month. This egg has the possibility of being fertilized. The fallopian tubes are tubular structures that act like a pathway, allowing the egg to travel from the ovaries to the uterus. When sperm fertilizes the egg, it then forms an embryo, which implants into the endometrial tissue within the uterus.
An ectopic pregnancy happens when this embryo attaches itself somewhere outside the uterus, or to an abnormal or scarred part of the uterus.
What Causes Ectopic Pregnancy?
An ectopic pregnancy happens when a fertilized egg attaches itself in a place other than inside the uterus, often in the fallopian tubes. The fallopian tubes normally help move an egg from the ovaries to the uterus, thanks to smooth muscle contraction and tiny, hair-like structures called cilia. However, if the fallopian tubes are damaged, often due to inflammation, they might not work properly. This can lead to the egg getting stuck there.
There are many things that can cause this inflammation, such as toxins, infections, immune responses, and hormonal changes. Damage to the fallopian tubes causes an increase in molecules called pro-inflammatory cytokines, which can encourage the egg to implant and start growing in the tube. One of these molecules is called interleukin 1, which is produced during infections such as chlamydia. Interleukin 1 is crucial for normal embryo implantation in the womb, but it also recruits white blood cells called neutrophils, which could cause more damage to the fallopian tubes.
Something else that affects the fallopian tubes is the frequency of cilia beating, which can be reduced by smoking and infection. Changes in hormone levels throughout the menstrual cycle can also affect how frequently the cilia beat.
Sometimes, ectopic pregnancies can happen in other places than the fallopian tubes, such as the cervix, uterine cornea, myometrium, ovaries, or abdominal cavity. Women who have had a surgery that altered their fallopian tubes, like tubal ligation, are at higher risk for ectopic pregnancies because the surgery may have changed how the tubes work. There can even be cases where a woman has a normal pregnancy in the uterus at the same time as an ectopic pregnancy, which is known as a heterotopic pregnancy.
Risk Factors and Frequency for Ectopic Pregnancy
Ectopic pregnancy is a condition where the fertilized egg implants outside the womb, and it’s more common than you may think. It occurs in 1 to 2% of all pregnancies and in 2 to 5% of pregnancies with assisted reproductive technologies like IVF. However, only 10% of these pregnancies implant somewhere other than the fallopian tubes.
- Cesarean scar pregnancies (where the egg implants into a scar from a previous c-section) account for 4% of all ectopics and occur in 1 out of 500 women who’ve had at least one cesarean section before.
- Interstitial pregnancies (where the egg implants in the part of the fallopian tube that enters the uterus) make up about 4% of all ectopic pregnancies and are especially dangerous as they have up to 7-time higher fatality rates due to a high risk of severe bleeding.
- Intramural pregnancies (the egg implants within the uterine muscle) constitute 1% of ectopic pregnancies.
- Pregnancies that implant in the abdominal cavity make up about 1.3% of ectopic pregnancies and most commonly attach in the pouches in front of and behind the uterus but can also implant on the surfaces of ovaries or the uterus. They’ve even been found in more distant sites like the retroperitoneal area, spleen, and liver.
There are several risk factors that can raise your chance of having an ectopic pregnancy. Advanced maternal age, smoking, past ectopic pregnancies, damage or surgery on the fallopian tubes, previous pelvic infections, exposure to diethylstilbestrol (DES), intrauterine device (IUD) use, and assisted reproductive technologies all contribute to the risk. Women who had an ectopic pregnancy before are up to ten times more likely to have one again compared to other women. And interestingly, women who go through in vitro fertilization can sometimes end up with a rare condition called a heterotypic pregnancy, which is where they have one normal pregnancy in the uterus and one ectopic pregnancy simultaneously. This can happen in as many as 1 in 100 women undergoing IVF.
Signs and Symptoms of Ectopic Pregnancy
When a woman experiences signs like pelvic discomfort, abdominal pain, nausea, fainting or light-headedness, and vaginal bleeding, it could indicate an ectopic pregnancy, especially if she’s of reproductive age. These symptoms might be more likely if she’s sexually active and has missed her last period or if she’s having unusual uterine bleeding. Other risk factors include a history of ectopic pregnancy, damaged fallopian tubes, or achieving pregnancy through fertility treatments.
Doctors start by getting a thorough medical history, followed by a detailed physical exam. Checking vital signs like heart rate and blood pressure helps understand if the patient’s body is responding normally. In the physical exam, doctors focus on any tenderness in the abdomen and around the pubic area and look for signs that might indicate internal fluid or other issues.
In cases of abdominal discomfort, knowing if the patient responds protectively (guarding) during the check can be informative. A physical check could also reveal pregnancy (gravid uterus), although this doesn’t rule out other problems like an advanced ectopic pregnancy or heterotopic pregnancy. If the woman is experiencing vaginal bleeding, a pelvic exam can be helpful both to look for signs of infection and to check the cervical opening (os). The bimanual aspect of the exam lets doctors feel for abnormalities or tenderness in the adnexa, or areas next to the uterus.
A thorough history and physical examination provide crucial information when looking into a possible ectopic pregnancy.
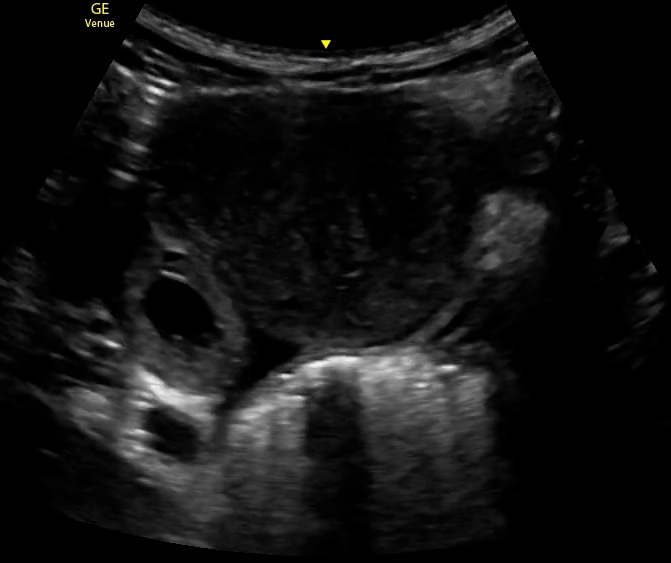
ultrasound.
Testing for Ectopic Pregnancy
Transvaginal ultrasound imaging, or taking images using an internal probe, is a critical tool for diagnosing suspected ectopic pregnancy, which is a pregnancy that occurs outside the womb. Confirming an ectopic pregnancy typically involves multiple ultrasound exams, measurements of a hormone called hCG in the blood, or both.
The first sign of a normal pregnancy seen on an ultrasound is a tiny sac located off-center in the inner uterine lining. This is usually surrounded by two rings of tissue, known as the “double decidual” sign. This sign generally appears during the 5th week of pregnancy on abdominal ultrasound images. The yolk sac, nourishing the embryo, will also become visible around this time, but its detection usually requires the transvaginal ultrasound imaging. By about six weeks into the pregnancy, an embryonic pole or the early structure of the embryo, becomes visible with this type of imaging.
However, certain factors like uterine fibroids (noncancerous growths in the uterus) or high body mass index can affect the accuracy of ultrasound imaging to identify an early pregnancy within the womb. In extreme situations, such as having large fibroids that obstruct the view, MRI imaging can be helpful. However, it’s important to consider that the accuracy of MRI and the possible risks associated with the use of a contrast agent called gadolinium need further study.
The most definitive way to confirm an ectopic pregnancy is by identifying a fetal heartbeat outside of the womb on an ultrasound. However, not all ectopic pregnancies develop a discernable fetal heartbeat, so its absence can be misleading. Other signs of ectopic pregnancy may include a pregnancy sac with or without a yolk sac located outside the uterus or an unusually complex mass in the adnexa, the area next to the uterus.
When imaging doesn’t adequately confirm an ectopic pregnancy, visual inspection of the suspicious mass can be done using a minimally invasive procedure known as laparoscopy. However, very small ectopic pregnancies, as well as those located in the cervix or previous cesarean section scars, might not be identified using laparoscopy.
Treatment Options for Ectopic Pregnancy
If a woman, who is in overall stable health condition, is diagnosed with a non-ruptured ectopic pregnancy, two methods can be safely and effectively used as treatment. These are giving an injection of a medicine called methotrexate, or performing a minor surgery called laparoscopy. The choice between these methods depends on the individual situation of the patient, including her health condition, test results, and how her pregnancy looks on scans. Her personal choice, after being fully informed about the pros and cons of each treatment, is also important.
Methotrexate could be especially beneficial for patients with relatively low hCG levels (a hormone produced in early pregnancy). High hCG levels might need a second dose. Research suggests that treatment with methotrexate doesn’t harm future fertility or ovarian health. After using methotrexate, the hCG levels should be monitored until they drop to a non-pregnancy level.
Surgery might be necessary if certain conditions are met, such as signs of internal bleeding, symptoms indicating a ruptured ectopic mass, or serious health instability due to the ectopic pregnancy.
The surgical management could include a procedure called salpingostomy or salpingectomy, and this decision depends on the patient’s health, how damaged the fallopian tube is, and whether she wants to have children in the future. In simple terms, salpingectomy involves removing all or part of the fallopian tube. Salpingostomy, also known as salpingotomy, means cutting into the fallopian tube to remove the ectopic pregnancy but leaving the tube itself in place.
What else can Ectopic Pregnancy be?
When doctors are trying to determine a diagnosis based on a patient’s health history and physical exam findings, it’s crucial to consider all possible conditions. For example, when examining a case of potential ectopic pregnancy, doctors must consider other conditions that may cause similar symptoms. These can include:
- Ovarian torsion (twisting of the ovary)
- Tubo-Ovarian abscess (infection in the ovary or fallopian tube)
- Appendicitis (inflammation of the appendix)
- Bleeding in a corpus luteum (formation in the ovary)
- Ovarian cyst rupture (bursting of a fluid-filled sac in the ovary)
- Threatened miscarriage (signs of a potential miscarriage)
- Incomplete miscarriage (some pregnancy tissue remains in the uterus)
- Pelvic inflammatory disease (infection of female reproductive organs)
- Ureteral calculi (stones in the tubes from the kidneys to the bladder)
A patient’s health history and current health status can help doctors determine which tests are necessary and the order in which these conditions should be considered.
What to expect with Ectopic Pregnancy
Patients with a lower beta hCG level usually have more optimistic chances of successful treatment using a single dose of methotrexate. The more an ectopic pregnancy has developed, the less likely it is that a single dose of methotrexate will be enough.
Patients who are severely unwell or unstable when they come in have a higher risk of getting worse. For instance, they may face conditions like severe blood loss induced shock or complications during surgery. Thus, early detection and quick intervention play a crucial role in influencing the prognosis or outcome.
The impact of surgeries that aim to save the fallopian tubes on fertility outcomes is still uncertain. Some findings suggest there isn’t a significant difference in the rates of successful pregnancies within the womb when comparing tube removal to more conservative treatments of the tube.
Possible Complications When Diagnosed with Ectopic Pregnancy
If a woman comes in early in her pregnancy with signs of an ectopic pregnancy – a condition where the embryo attaches outside the uterus – she could risk the life of a healthy pregnancy inside the uterus if she receives treatment with a drug called Methotrexate. Methotrexate is usually given in a single dose, but it may not always work. If the level of a hormone called hCG doesn’t drop by 15% between the fourth and seventh day after administration, a second dose might be necessary.
In some situations, a woman who comes in with symptoms like vaginal bleeding and pelvic pain might be wrongly diagnosed as having a miscarriage, especially if the ectopic pregnancy is located at the cervical os – the narrow passage forming the lower end of the uterus. In these cases, the woman may actually have a cervical ectopic pregnancy. This could pose a significant risk of severe bleeding and potential instability in her circulatory system if a medical procedure known as dilation and curettage is performed.
Managing ectopic pregnancies can also lead to complications, especially if treatment fails. Women could experience a condition known as ‘hemodynamic instability’, which affects the flow of blood around the body, despite receiving early surgical treatment. This could potentially lead to life-threatening situations.
Preventing Ectopic Pregnancy
When getting treatment for an ectopic pregnancy, patients might need to talk with their doctor about what foods, supplements, and medications to avoid while taking a drug called methotrexate. This is because certain things might negatively interact with the drug and make it work less effectively. Methotrexate can also increase the effect of other medicines that reduce the body’s immune response, and it can cause other side effects.
If a patient needs surgery, it’s important to follow all advice from their surgeon. This reduces the chance of getting an infection or experiencing other complications after the operation.











