What is Subchorionic Hemorrhage?
Vaginal bleeding during the first three months of pregnancy is quite common, occurring in about 16 to 25% of pregnancies. The most frequent reason for such bleeding in pregnant women between 10 to 20 weeks is conditions called subchorionic hemorrhage and subchorionic hematoma, which together account for about 11% of cases.
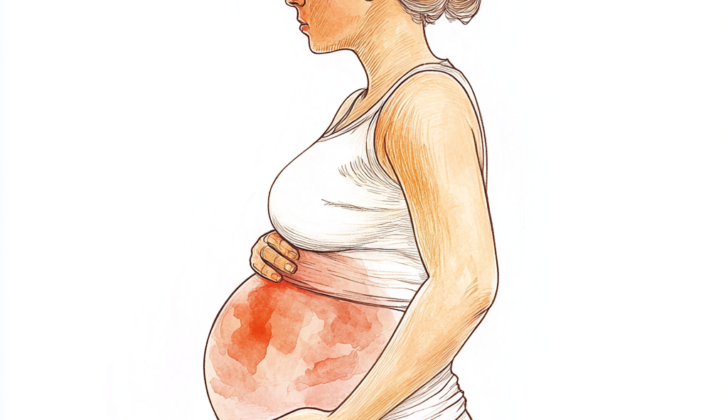
Subchorionic hemorrhage is bleeding that happens under the chorion membranes – these are the protective layers that surround the baby in the womb. This bleeding might happen due to the chorion membranes partially detaching from the womb’s inner wall.
Often, the term subchorionic hematoma is used interchangeably with subchorionic hemorrhage. Most of the time, women with these conditions experience light vaginal bleeding, but some women might not show any symptoms and the condition is only discovered during an ultrasound scan.
What Causes Subchorionic Hemorrhage?
The exact cause of subchorionic hematoma, a condition where blood accumulates between the uterus and the placenta during pregnancy, is still not fully understood. It seems that subchorionic hematomas occur due to partial separation of the chorionic membranes (layers of cells that develop into the placenta) from the wall of the uterus.
Having a malformed uterus, a history of multiple miscarriages, or infections in the pelvic area could possibly make a woman more likely to experience a subchorionic hemorrhage, which is bleeding in the same area as a hematoma.
Risk Factors and Frequency for Subchorionic Hemorrhage
Subchorionic hemorrhages are not unusual, particularly among women of childbearing age, often presenting as vaginal bleeding between the 9th to 20th weeks of pregnancy. It’s a topic that doctors have been studying since it was first identified in 1981 because the impacts on the pregnancy are debatable. Some research indicates that subchorionic hemorrhages could lead to negative issues during pregnancy, including high blood pressure disorders, the premature detachment of the placenta, and early birth.
However, contrasting studies have found no negative outcomes tied to subchorionic bleeding. There’s evidence to suggest that subchorionic hemorrhages are more common in women with a history of repeated pregnancy losses, those who’ve had more than one child, and women with known issues in the structure of their uterus.
Signs and Symptoms of Subchorionic Hemorrhage
Some people may not show any symptoms of certain gynecological issues, while others might experience vaginal bleeding. Typically, abdominal pain is not common, but a few might feel cramping or contractions. It’s important to know that about a quarter of all pregnancies have the complication of bleeding during the first three months. When someone has vaginal bleeding, it’s necessary to document specific characteristics, like how much bleeding there is, whether it’s constant or sporadic, and if it comes with abdominal pain or contractions. Also, it is crucial to get detailed information about the person’s medical history. This should include past pregnancies, gynecological history, like any sexually transmitted infections or pelvic inflammatory disease, and any risks related to serious conditions such as ectopic pregnancy.
It’s important to examine the abdomen, starting with gentle tapping in the area with the least pain. If a person shows up with vaginal bleeding, a vaginal exam using a speculum might be needed to assess the amount of bleeding and how the cervix looks. If there are any blood clots or tissue identified during the exam, this should be examined further and sent for lab tests. An abdominal or vaginal ultrasound should be done as well to check for any signs of hemorrhage within the uterus, as up to 22% of these cases show these symptoms on an ultrasound. If the pregnancy is somewhere between 10 to 12 weeks along, the fetus’s heartbeat must be checked, with a normal range being between 110 to 160 beats per minute.
Testing for Subchorionic Hemorrhage
When women of childbearing age come to the hospital with stomach pain, unusual menstrual cycles, or vaginal bleeding, doctors typically run tests to check if they’re pregnant. They do this by testing the urine and measuring a hormone called beta hCG.
If a woman is pregnant and experiences abdominal discomfort or vaginal bleeding, the doctor will want to make sure there are no severe issues. One of these issues could be an ectopic pregnancy, which is when the baby starts to grow outside the womb. To rule this out, doctors typically use ultrasound imaging.
Ultrasound is the best way to see what’s going on inside the body. In the early stages of pregnancy, it can help identify various conditions that may cause bleeding.
On an ultrasound, doctors might see a dark, moon-shaped area behind the fetal membrane (the outer layer that surrounds the fetus). This can even push up against the edge of the placenta (the organ that develops in the uterus during pregnancy to provide oxygen and nutrients to the baby).
However, it can sometimes be challenging to spot and identify a condition known as subchorionic hematoma. That’s because the hematoma (pool of blood) can blend in with other structures inside the uterus. If the hematoma is very dark on the ultrasound, it can be mistaken for amniotic fluid (the fluid that surrounds and cushions the baby). If it appears lighter, it can be confused with the muscular layer of the uterus. If it’s extra bright, it can look like placental tissue.
For women with severe vaginal bleeding, additional tests should be conducted. These include checking the levels of red blood cells, assessing the blood’s clotting ability, and determining the blood type. Quick action can prevent complications in patients who are experiencing heavy blood loss and showing signs of instability. This can happen when the body loses too much blood, and the heart can’t pump enough blood to the body.
Treatment Options for Subchorionic Hemorrhage
The treatment and management of a condition known as subchorionic hemorrhage, which sometimes happens during pregnancy, depend on various factors. These factors include the patient’s specific symptoms, the gestational stage of the pregnancy (how far into the pregnancy they are), and their overall health condition.
If the patient comes to the hospital because of vaginal bleeding, which is a common symptom in cases of subchorionic hemorrhage, treatment needs to start quickly. If the patient’s blood type is RhD negative, they should get a medication called anti-D immune globulin. This medicine helps protect against a condition called alloimmunization in future pregnancies. Alloimmunization is when the mother’s immune system reacts against the baby’s blood cells, mistaking them for foreign bodies. The treatment will be personalized based on the patient’s specific situation, including the type and severity of their symptoms, and the size and location of the blood clot, or hematoma.
Some health resources recommend giving patients with first-trimester vaginal bleeding a supplement called vaginal progesterone. However, this has not been proven to increase the likelihood of a successful, full-term birth, so it’s not routinely recommended. Some studies have suggested that bed rest may be beneficial for patients, resulting in fewer miscarriages and a higher rate of full-term pregnancies. However, these studies have not been robust enough to influence current treatment guidelines. Therefore, if both the mother and baby are stable and there is no sign of a large amount of blood loss, it is generally sufficient to manage the condition conservatively, with follow-up ultrasound scans to check on the progress of the pregnancy.
What else can Subchorionic Hemorrhage be?
When a woman of childbearing age presents with abdominal pain or vaginal bleeding, there could be many possible causes. It’s important to figure out if these symptoms indicate a serious or life-threatening condition. If the woman is pregnant or thought to be, an ultrasound should be done to confirm that the pregnancy is inside the uterus, removing the possibility of a potentially dangerous ectopic pregnancy, which is a pregnancy that is growing outside of the uterus.
Other potential causes could be:
- Early pregnancy loss (otherwise known as a miscarriage or spontaneous abortion)
- Threatened miscarriage
- Bleeding from the implantation of the embryo into the uterus
- Problems with the placenta such as placental abruption, placenta previa, or vasa previa
- A condition called gestational trophoblastic disease
- A tear in the uterus, known as uterine rupture
- Ovarian torsion, which is when an ovary twists around the ligaments that hold it in place
- A tubo-ovarian abscess, which is an infection in the fallopian tube and ovary
What to expect with Subchorionic Hemorrhage
For women who have a sonogram that identifies a condition called subchorionic hematoma, or a blood clot next to the pregnancy sac, the health outcomes for the fetus depend on factors such as the size of the clot, the woman’s age, and how far along the pregnancy is. If this clot takes up 25% or more of the pregnancy sac, there could be an increased risk of pregnancy loss. The clot’s location also matters. For instance, if it’s behind the placenta rather than at the edge, it can lead to worse outcomes.
The earlier a subchorionic hematoma is discovered in a pregnancy, the higher the risk of pregnancy failure. However, this condition can increase the risk of spontaneous miscarriage. If the pregnancy continues, the risk doesn’t affect premature birth rates or the type of delivery (like vaginal birth or c-section).
It’s also worth remembering that subchorionic hematomas found in the first three months of pregnancy aren’t linked to negative outcomes after 20 weeks of pregnancy. However, when the clot is larger compared to the size of the pregnancy sac, especially when paired with general pelvic pain, this can extend the hospital stay and increase the likelihood of losing the pregnancy.
Possible Complications When Diagnosed with Subchorionic Hemorrhage
Pregnant women diagnosed with subchorionic hematoma (SCH), which is a condition where blood collects between the uterus and the placenta, face a higher risk of miscarriage or early pregnancy loss. They are also five times more likely to experience placental abruption, a serious condition where the placenta separates from the uterus. Other risks include preterm labor, where the baby is born before 37 weeks of pregnancy, premature rupture of membranes, which is when the water breaks before labor starts, and both early and late pregnancy loss.
There’s also a link between a subchorionic hematoma diagnosis in early pregnancy and the development of high blood pressure in the third trimester, also known as pregnancy-induced hypertension. However, having SCH early in the pregnancy doesn’t affect the mode of delivery or make any adverse outcomes in the pregnancy more likely.
- Increased risk of miscarriage or early pregnancy loss
- Higher chance of placental abruption
- Potential preterm labor
- The possibility of premature rupture of membranes
- Risk of both early and late pregnancy loss
- Potential development of pregnancy-induced hypertension in the third trimester
Preventing Subchorionic Hemorrhage
A subchorionic hematoma is a medical term for a type of blood clot that sometimes forms in the womb during pregnancy. It’s not something that typically happens, but it’s not rare either. The presence of this clot doesn’t mean you’re going to lose your baby. In fact, many women with this condition go on to have healthy babies, as long as they are carefully monitored.
Having subchorionic bleeding, the medical term for bleeding caused by the clot, doesn’t mean your pregnancy is immediately at risk. However, it’s crucial that you stay in touch with your doctor, so they can keep track of your situation. It’s also important for you to know when you should take special care and when you should get back to the hospital.
You should be aware of certain warning signs and take precautions accordingly. This includes, but isn’t limited to, experiencing vaginal bleeding or spotting, as well as any abdominal pain. If these symptoms occur, it’s important that you reach out to healthcare professionals right away.