What is Hereditary Spherocytosis ?
Hereditary spherocytosis (HS) is the most common cause of a type of blood disorder known as hemolytic anemia, which results from an abnormal red blood cell membrane. This condition falls under the broader category of blood disorders that are present from birth, specifically known as congenital hemolytic anemia. The condition first came to light in the early 1900s, thanks to Oskar Minkowsky.
In those with HS, red blood cells can’t keep their usual shape due to changes in their genes. These genetic changes affect proteins within the cell, which are crucial for maintaining its shape. The affected proteins may include spectrin, ankyrin, band 3, and band 4.2. Each of these proteins is produced by different genes.
How this condition presents itself can vary quite a bit. It depends on how severe the disease is and the type of genetic mutation involved.
What Causes Hereditary Spherocytosis ?
Red blood cells, known as erythrocytes, have a unique, doughnut-like shape which is flexible and gives them the ability to adapt to small changes in the environment inside our blood vessels. Their structure is primarily made up of a fat layer called a lipid bilayer, and proteins that form a framework or “skeleton”. This structure helps them maintain their shape and allows the right amount of ions, tiny charged particles, to move in and out of the cells.
Hereditary spherocytosis is a condition where one or more of these essential proteins are missing. This causes the cell’s “skeleton” to be unable to properly support the lipid layer on the surface of the cell, causing it to take on a sphere-like shape instead. This abnormal shape reduces their flexibility and makes these red blood cells more fragile. It also makes it hard for them to adjust to changes in the environment inside our blood vessels, such as a drop in osmolarity, which refers to the concentration of particles in a solution.
Additionally, these sphere-shaped cells, referred to as spherocytes, also have an abnormality that causes more sodium ions to enter the cell. This leads to an increased energy demand, as the cell has to work harder to pump out the extra sodium. This process requires energy in the form of Adenosine Triphosphate (ATP).
Risk Factors and Frequency for Hereditary Spherocytosis
Hereditary spherocytosis is the most typical genetic disease that causes the destruction of red blood cells. It’s especially common in Northern Europe and North America, but can affect different racial groups. Roughly 1 in every 2000 people are diagnosed with this illness. However, plenty of cases might go unnoticed because they do not show obvious symptoms.
Signs and Symptoms of Hereditary Spherocytosis
Hereditary spherocytosis is a blood disorder that runs in families. This illness might be the cause if a child comes in with an enlarged spleen, anemia (low red blood cell count), and high bilirubin levels in the blood. Some patients may also have gallstones without any symptoms, especially if they have a family history.
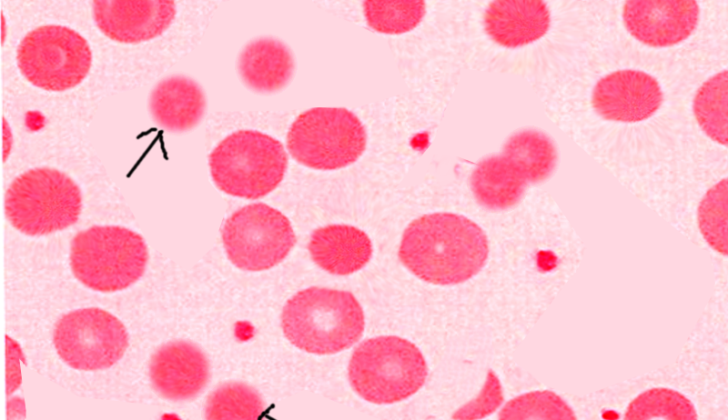
In newborns, signs of this disorder are different. The main symptom is often jaundice, or a yellowing of the skin and eyes caused by too much bilirubin. Newborns with unexplained jaundice could possibly have hereditary spherocytosis. Also, findings common in older infants or adults, such as spherocytes (misshapen red blood cells caused by hemolysis or breakdown of red blood cells), are less common in newborns.
Most newborns with hereditary spherocytosis have a family history of the disorder. So, if a newborn comes in with jaundice and no known cause, it can be helpful to know of any family history of hereditary spherocytosis in narrowing down the diagnosis.
Testing for Hereditary Spherocytosis
For doctors to diagnose a condition, they often rely on a patient’s medical history, current symptoms, and test results. In the case of a disease like hereditary spherocytosis, your doctor might order a blood test that includes a blood smear, reticulocyte count, complete blood count, bilirubin level, and red cell osmotic fragility tests.
In simple terms, a blood smear is a drop of blood spread thinly onto a glass slide that is then treated with a special stain and examined under a microscope by a pathologist. A reticulocyte count measures how fast red blood cells, also known as reticulocytes, are made by the bone marrow and released into the blood. A complete blood count measures various components of the blood, including red and white blood cells. Bilirubin level measures the amount of bilirubin, a yellow-orange substance made during the normal breakdown of red blood cells. Lastly, a red cell osmotic fragility test measures how resistant red blood cells are to bursting when exposed to changes in fluids.
Hereditary spherocytosis is considered likely in patients if their tests come back with Coombs-negative hemolysis, which means red blood cells are being destroyed in the bloodstream, and an increased mean corpuscular hemoglobin concentration (MCHC), which is the average amount of hemoglobin inside a single red blood cell. A positive medical history for hereditary spherocytosis, the presence of spherocytes, a specific type of red blood cell, on microscopic examination of the blood, or a positive result in a more specialized test can confirm the diagnosis. These specialized tests include osmotic fragility test, eosin-5-maleimide (EMA) binding test, or acidified glycerol lysis test (AGLT).
Hereditary spherocytosis varies in severity, and different patients will experience different symptoms. Doctors often categorize the severity based on levels of hemoglobin, which is a protein in red blood cells that carries oxygen. They consider the anemia (a shortage of red blood cells) as severe if the hemoglobin is less than 8 g/dL, moderate if it’s between 8 to 10 g/dL, or mild if it’s between 10 to 11.5 g/dL in women, or 10 to 13.5 g/dL in men.
Treatment Options for Hereditary Spherocytosis
In treating hereditary spherocytosis, our goal is to enhance the quality of life while trying to avoid the complications that can arise from the condition. If complications occur, it’s important to treat them appropriately. In children, we aim to maintain the hemoglobin level above 7 to 8 grams per deciliter (g/dL). However, for newborns, there’s no specific hemoglobin level at which we should start a red blood cell transfusion. Instead, the decision is primarily based on how well the newborn is maintaining a steady heartbeat and blood flow (hemodynamic stability) and the extent of red blood cell destruction (hemolysis).
According to a past study, treatment with a hormone called erythropoietin has proven beneficial for increasing hemoglobin levels in most infants with hereditary spherocytosis. This treatment could also lessen the need for red blood cell transfusions.
If a newborn with hereditary spherocytosis develops hyperbilirubinemia – a condition where there’s too much bilirubin in the blood, which can cause the skin, eyes, and other parts of the body to turn yellow (jaundice) – it’s crucial to treat it quickly to prevent a kind of brain damage known as kernicterus. The decision to carry out a blood exchange transfusion – a procedure that removes the patient’s blood and replaces it with fresh donor blood – depends on several factors like the baby’s age, level of indirect bilirubin, and how quickly this level is increasing.
Removing the spleen (a splenectomy) can significantly lessen symptoms in many patients. This is because the spleen is the main organ where red blood cells get destroyed, and extraction can slow this process. While a positive outcome is generally observed after splenectomy, a study has found that the effectiveness of this treatment can depend on the level of spectrin – a protein that helps red blood cells maintain their shape. The goal of splenectomy is primarily to improve one’s quality of life. While it’s generally recommended for patients with severe hereditary spherocytosis, the decision gets a little complex for those with a moderate form of the disease – it’s a subject of controversy within the medical community.
Patients with hereditary spherocytosis have a higher consumption of folate – a type of vitamin B that helps in the formation of red and white blood cells. This is due to an increase in the production of red blood cells (erythropoietic activity) compensating for their destruction (hemolysis). Therefore, particularly in patients with a moderate to severe form of the disease, it’s crucial that they get an ample amount of folate, either through their diet or via supplements.
What else can Hereditary Spherocytosis be?
If someone has hereditary spherocytosis, which is a condition affecting red blood cells, doctors also consider other conditions that affect red blood cells as possible causes of their symptoms. This includes:
- Elliptocytosis and its variants
- Hereditary stomatocytosis
- Pyropoikilocytosis
- Ovalocytosis
They would also consider conditions that involve enzymes in the red blood cells, such as:
- Glucose-6-phosphate dehydrogenase (G6PD) deficiency
- Pyruvate kinase deficiency
Autoimmune hemolytic anemia (AIHA) is another condition doctors would consider, especially in adult patients. AIHA is a common cause of the breakdown of red blood cells, but it’s typically identified by a positive Coombs test and doesn’t often run in families like elliptocytosis does.
What to expect with Hereditary Spherocytosis
The general outlook for people with hereditary spherocytosis, a condition where the red blood cells become sphere-shaped, is usually good. However, it can differ based on how severe the disease is.
Possible Complications When Diagnosed with Hereditary Spherocytosis
Around half of the people with the hereditary spherocytosis genetic blood disorder experience anemia, and 10 to 15% may have an enlarged spleen or yellowish skin and eyes due to jaundice. The majority of these patients usually have partial hemolysis, or destruction of red blood cells, along with mild anemia.
Patients who have their spleen removed are at risk of getting sepsis, a serious infection that can spread throughout the body. The most common organisms causing sepsis are encapsulated bacteria like Streptococcus pneumoniae, Neisseria meningitides, and Haemophilus influenzae. The chance of getting sepsis is tied with the patient’s age.
Gallstones, or Cholelithiasis, is one of the most common complications in people with hereditary spherocytosis, especially in those between the ages of 10 and 30. However, even younger patients can also get gallstones.
Patients with this condition may go through different types of blood crises, such as hemolytic, aplastic, or megaloblastic. The most common is the hemolytic crisis, where red blood cells are destroyed rapidly. This type of crisis is usually associated with fever and can be triggered by viral infections or might occur randomly.
Aplastic crises, a blood cell or bone marrow disorder, can be more severe than hemolytic crises and could lead to acute heart failure. They are often associated with parvovirus B19. Symptoms in children include chills, fever, stomach pain, muscle aches, and a generalized red or pink rash. This condition typically begins with a decrease in hemoglobin and reticulocytes, a type of immature red blood cells, followed by a reduction in bone marrow erythroblasts and bilirubin. Recovery usually sees an increase in neutrophils and platelets first, then by reticulocytosis and a gradual increase in hemoglobin levels.
Megaloblastic crises, which are not very common, are usually caused by a deficiency in folate levels. These can be treated with adequate folate supplementation.
Common Health Risks
- Anemia
- Enlarged spleen or jaundice
- Sepsis following spleen removal
- Gallstones
- Hemolytic crisis
- Aplastic crisis potentially leading to acute heart failure
- Megaloblastic crisis due to folate deficiency
Preventing Hereditary Spherocytosis
If you or your child have a condition called hereditary spherocytosis, it’s very important to receive clear educational information about this disease. Regular medical check-ups and close monitoring are essential. Plus, you should learn early warning signs of potential complications from the disease, like aplastic crises (a serious condition where the body stops producing enough new blood cells) or cholelithiasis (the formation of gallstones).
For those who’ve had surgery to remove the spleen as part of their treatment (a procedure called a splenectomy), they will need additional preventative vaccinations against certain infections. This is because removing the spleen can make the body more prone to some types of bacterial infections. Regular follow-ups are important to watch for any potential complications from the surgical procedure.
When it comes to people with moderate forms of hereditary spherocytosis, deciding whether or not to perform a splenectomy can be a complex decision. Detailed discussions, educational counselling, and a comprehensive plan are needed before making a final decision. Everyone involved, including the patient, the family, and the doctors, should be in agreement.