What is Microcytic Hypochromic Anemia?
Anemia is a common condition that occurs when the number of red blood cells in your body is lower than normal. Red blood cells contain a protein called hemoglobin, composed of four chains of proteins and a ring structure that holds iron. This iron is an integral part of hemoglobin and is mainly responsible for carrying oxygen. A shortage of iron in the body can affect the production of hemoglobin, which in turn, impacts the distribution of oxygen to different parts of the body. This reduction in the ability of the blood to carry oxygen can result in less oxygen reaching the tissues in your body, a condition known as tissue hypoxia. The diagnosis of anemia usually involves measuring hematocrit (the ratio of red blood cells to the total blood volume) and checking the concentration of hemoglobin.
What Causes Microcytic Hypochromic Anemia?
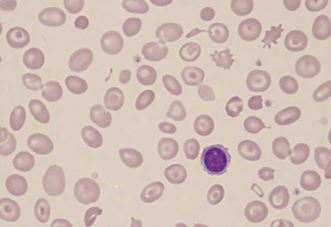
Microcytic, hypochromic anemia is a type of anemia where your red blood cells are smaller (microcytic) and paler (hypochromic) than normal. This usually happens when your body doesn’t have enough iron. This can be due to various reasons. You may not be getting enough iron in your diet, your body might not be absorbing iron well from the food you eat, or you may be losing blood, either slowly over time or suddenly due to an injury. Other times, you might need more iron than usual, such as during pregnancy or recover from major traumas or surgeries.
Risk Factors and Frequency for Microcytic Hypochromic Anemia
Anemia, a condition where your body lacks enough healthy red blood cells, is a common problem worldwide. The World Health Organization (WHO) reveals that nearly 1 in 4 people globally are currently living with anemia, and a lot of these cases are due to an insufficient intake of iron.
Women, particularly those in their childbearing years, are often more affected. This is largely due to the blood loss they experience every menstrual cycle. Interestingly, about 41% of pregnant women around the world are dealing with anemia. Non-pregnant women in the pre-menopause stage are not far behind, with nearly 30% experiencing anemia.
Men, on the other hand, are less susceptible to anemia because of their testosterone levels. Yet, about 12.7% of adult men across the globe are still coping with this condition. After women, pre-school-aged kids are next most prone to anemia. This happens mostly because of a low iron content in their diet. Despite containing more iron than human milk, cow’s milk still doesn’t provide enough because the iron it contains is hard for our bodies to use efficiently.
- Nearly a quarter of the world’s population is affected by anemia, with many of these cases due to lack of iron.
- An estimated 41% of pregnant women and 30% of non-pregnant women in the pre-menopausal phase have anemia.
- About 12.7% of men worldwide also deal with anemia despite being generally less prone to the condition.
- After women, pre-school-aged kids are the next group most affected by anemia, often due to a lack of iron in their diet.
- Cow’s milk has more iron than human milk, but our bodies can’t use it efficiently.
Signs and Symptoms of Microcytic Hypochromic Anemia
Iron deficiency can reveal itself through several tell-tale signs. Some common causes include:
- Not consuming enough iron-rich foods
- Heavy menstrual periods that cause blood loss
- Blood loss from stomach or small intestine ulcers
- Cancer in the large intestine
- Severe injury which depletes iron stores.
Some people with iron deficiency might also have odd cravings to eat non-food items, such as clay, ice, or flour. This is known as pica. In certain cases, people may have difficulty swallowing because food feels stuck in the chest. This, along with a swollen tongue and anemia, is called Plummer-Vinson syndrome, a rare outcome of iron deficiency.
In a doctor’s examination, a person might show signs like:
- Pale skin, especially on hands
- Bright redness in the inner eyelids
- Fast heartrate
- Rapid breathing
- Extreme tiredness
- Spoon-shaped nails (koilonychia)
If the iron deficiency is severe, it may even cause signs and symptoms of chest pain due to an insufficient supply of oxygen to the heart muscles.
Testing for Microcytic Hypochromic Anemia
When a doctor suspects anemia, the first step is usually a complete blood count, or CBC. This blood test not only identifies anemia, but also gives details about the red blood cells, such as their volume and the amount of hemoglobin they contain. When anemia is due to a lack of iron, these cells are often smaller and have less hemoglobin than usual.
Next, the doctor may order iron studies. These tests look at transferrin saturation, total iron-binding capacity, and ferritin levels. In cases of iron deficiency anemia, the transferrin saturation is usually very low, indicating less iron is being transported to your body’s cells. At the same time, total iron binding capacity is often increased, which shows that your body is trying to grab onto as much iron as it can.
Ferritin, a protein that stores iron, is typically low in people with iron deficiency anemia. However, ferritin levels can increase during infections, so a low or normal ferritin level does not always represent an absence of iron deficiency anemia.
Finally, a look at a sample of your blood under a microscope can show small, pallid red blood cells with a thin rim of hemoglobin. These “pencil cells” are a common sign of iron deficiency anemia.
Treatment Options for Microcytic Hypochromic Anemia
Once hypochromic microcytic anemia (a type of anemia characterized by smaller and paler than normal red blood cells) is diagnosed, treatment can begin. This usually involves taking a 325 mg tablet of a medication called ferrous sulfate three times a day. This treatment helps the body absorb up to 10mg of iron from the gut, which is why it’s typically the first choice for treating this type of anemia. However, some patients can experience side effects such as nausea and constipation.
These side effects might make it challenging for some people to continue the treatment, but it’s possible to improve this by increasing the dosage gradually while carefully monitoring for side effects. Doctors typically aim to find the highest dose that a patient can tolerate and use this for replacing the iron they’ve lost. It takes about three weeks to start noticing an improvement after beginning the treatment, and full effects should be seen by two months.
When oral medication isn’t the best option, iron can be given intravenously (via a needle directly into a vein). This can be the case if:
* The side effects of the oral medication are too severe
* The anemia doesn’t improve with oral treatment
* There’s a problem with the digestive system that makes it difficult to absorb iron properly
* The patient continues to lose blood faster than it can be replaced with oral treatment
An iron preparation mixed with a substance called sorbitol can be slowly infused into the body over five minutes at a dose of 50mg per kg body weight for men and 35mg per kg body weight for women. This dose is usually the amount of iron that the body is lacking, plus an extra gram to replenish the body’s iron reserves.
What else can Microcytic Hypochromic Anemia be?
When a patient has hypochromic microcytic anemia, a condition that means their red blood cells are smaller and lighter in color than normal, doctors will consider several possible causes. These may include:
- Thalassemias, a set of inherited blood disorders
- Anemia of chronic disease, which can happen as a result of long-term medical conditions
- Lead poisoning
- X-linked sideroblastic anemia, a genetic disease that prevents the body from properly incorporating iron into red blood cells
Conducting the right tests to confirm which of these conditions is causing the symptoms is crucial to providing appropriate treatments.