What is Pernicious Anemia?
Pernicious anemia is a somewhat uncommon disease where the body’s immune system affects the absorption of vitamin B12 from food. This leads to a deficiency of the vitamin and consequently, a type of anemia known as megaloblastic anemia. It can happen to anyone, anywhere in the world, but seems to impact people above 60 years old more often. Diagnosing this disease can be complicated because it shows up in many different ways, and the tests available to identify it have limitations.
Still, once it’s diagnosed, treatment typically involves supplementing vitamin B12, which often improves the anemia. Even with improvement though, patients will need to continue taking vitamin B12 supplements and have regular check-ups for the rest of their lives.
What Causes Pernicious Anemia?
Pernicious anemia is a disease that occurs due to an autoimmune problem. This kind of anemia is known as megaloblastic anemia and it is caused by a deficiency in vitamin B12 because of a deficiency in a substance known as intrinsic factor (IF). In simple terms, IF is a special protein made by particular cells in the stomach that helps your body absorb vitamin B12. When your body produces antibodies that fight against IF, it hinders vitamin B12 from attaching itself to this protein, and as a result, your body can’t absorb the vitamin.
In up to a quarter of patients who have autoimmune gastritis, a condition that affects certain parts of the stomach, pernicious anemia is discovered. This stomach condition destroys the cells that produce both IF and stomach acid, reducing the amount of available protein for absorbing vitamin B12 from food and causing a decrease in the release of a nutrient called cobalamin. Sometimes ‘pernicious anemia’ and ‘autoimmune gastritis’ are used interchangeably, but you should know that pernicious anemia is actually seen as a later development in the progression of autoimmune gastritis.
Interestingly, people with pernicious anemia are more likely also to have other autoimmune disorders like type 1 diabetes, autoimmune thyroid disease, and a skin condition called vitiligo. Furthermore, research studies have found certain genes that are linked to a higher risk of developing pernicious anemia.
However, whether a bacterium called Helicobacter pylori, known for causing stomach ulcers, plays a part in causing pernicious anemia is still uncertain.
Risk Factors and Frequency for Pernicious Anemia
Pernicious anemia is a condition that is not very common, particularly in people with European ancestry, where it’s found in less than 1% of the population. However, it can be a common cause of a type of anemia known as megaloblastic anemia worldwide. Although it can affect people of all ages, it usually impacts those who are over 60-70 years of age more, with about 2% of them having it. It affects both men and women in different proportions depending on the region. Interestingly, people of Asian descent have a lower chance of developing this condition compared to other groups.
Signs and Symptoms of Pernicious Anemia
Pernicious anemia is a slow-developing condition that can take 2 to 5 years to present noticeable symptoms. It’s tricky to diagnose due to the variety of potential symptoms which can also be associated with other conditions. The disease may cause a wide array of symptoms like fatigue, headache, depression, and much more.
Signs of the disease often include:
- Constitutional symptoms: fatigue, lethargy, loss of appetite, and weight loss
- Neurological changes: headaches, confusion, difficulty focusing, memory loss, cognitive decline, numbness, and balance issues
- Psychiatric effects: emotional instability, depression, personality changes, psychosis
- Otolaryngologic symptoms: loss or change in the sense of taste, inflammation of the tongue
- Cardiopulmonary indications: palpitations, difficulty breathing
- Gastrointestinal problems: indigestion, diarrhea, reduced appetite
Patients with advanced pernicious anemia may also have noticeable physical characteristics such as pale or yellowing skin, dry skin, tender tongue, and rapid heart rate. Neurological complications, such as peripheral neuropathy and subacute combined degeneration (SCD), can be a significant part of the condition, affecting sensation, reflexes, mobility, and vision. Sometimes these neurological signs occur even without the presence of anemia.
If the patient or a close family member has an autoimmune condition like diabetes type 1, vitiligo, or hypothyroidism, this may increase the likelihood of having pernicious anemia. In such cases, a neuropsychiatric evaluation may be needed.
Testing for Pernicious Anemia
Diagnosing pernicious anemia, a condition caused by a deficiency in vitamin B12, can be challenging due to the lack of a widely approved test for B12 absorption. Multiple approaches and criteria exist for diagnosis.
Doctors typically carry out an initial set of tests, looking at blood counts, cobalamin (a form of B12) level, folate level, iron levels, and reticulocyte count (which measures the amount of young red blood cells in your body). An examination of a sample of your blood under a microscope is also usually done.
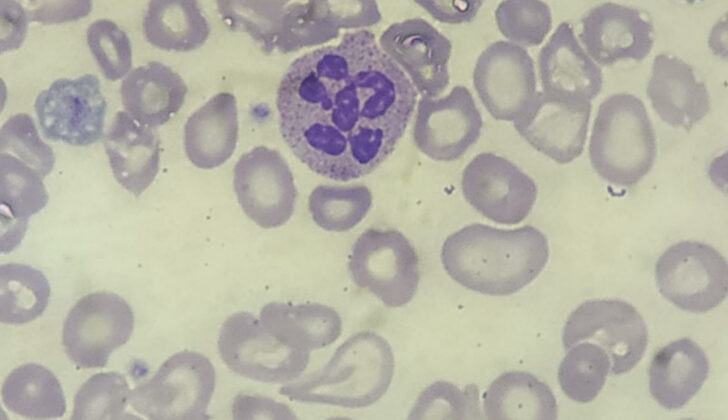
If your complete blood count (CBC) indicates anemia, signs of larger than average red blood cells (a condition called macrocytosis), and a reduction in all types of blood cells (pancytopenia), it could be a sign of pernicious anemia. However, about one-third of people with a B12 deficiency won’t have macrocytosis. Your reticulocyte count may show fewer reticulocytes than normal.
Looking at a sample of your blood under a microscope may reveal some distinctive features. It can show larger than normal red blood cells (macro-ovalocytes), neutrophils (a type of white blood cell) with more segments than normal (hypersegmented neutrophils) and variable red blood cell size and shape (anisopoikilocytosis). However, these features are not exclusive to pernicious anemia and can occur in other types of anemia too.
A B12 deficiency is defined by a serum cobalamin level of less than 200 ng/L in the right context. However, the single measure of cobalamin level alone may not be reliable for detecting B12 deficiency. If your cobalamin level is 200 ng/L or more, additional tests like serum MMA, fasting homocysteine, and holotranscobalamin (HTC) might be needed to help with the diagnosis.
In addition, it is important to rule out anemia caused by folate deficiency, as treating B12-deficient individuals with folate alone may exacerbate associated nerve damage.
Anti-Intrinsic Factor (IF) antibodies tests are carried out to confirm pernicious anemia as these antibodies interfere with B12 absorption in the gut. Positive results for these antibodies, along with a serum cobalamin level of less than 200 ng/L, confirm the diagnosis for pernicious anemia.
It’s worth noting that while the test for anti-IF antibodies is highly specific, it is less sensitive, which means it could falsely show the absence of the disease. It is also important to remember that not all IF antibodies are the same; Type 1 prevents B12 from binding to IF, and Type 2 prevents the B12/IF complex from being absorbed. About 70% of patients with pernicious anemia have Type 1 IF antibodies.
Although rarely needed, a bone marrow biopsy can show irregularities in cell development. If you have pernicious anemia, you could also be suffering from autoimmune gastritis, a condition where the immune system mistakenly attacks parts of your own body, in this case, the stomach.
In conclusion, diagnosing pernicious anemia involves several tests and examinations, and it may require an endoscopy with biopsy in some cases to confirm the diagnosis and check for other conditions.
Treatment Options for Pernicious Anemia
People diagnosed with pernicious anemia need treatment for life. This treatment usually begins with a B12 injection that is given daily or every other day for 1 to 2 weeks. The B12 used can be hydroxocobalamin (in Europe) or cyanocobalamin (in the United States). After the first few weeks, you then get weekly injections for 1 to 2 months. After this period, the frequency of the injections usually drops to once a month if cyanocobalamin is used or every 2 to 3 months if using hydroxocobalamin.
After these initial intense treatment stages, patients have a choice. They can either continue to get the B12 injections for their whole life or take high-dose oral B12 tablets daily. A 2016 review stated that taking oral vitamin B12 is as effective as getting B12 injections. These tablets usually contain cyanocobalamin in doses of 1000–2000 micrograms. There are also other types of B12, like sublingual (which you dissolve under your tongue) and intranasal (spray or drops into the nose), but these are not typically recommended.
What else can Pernicious Anemia be?
Other factors that can lead to anemia characterized by large red blood cells (megaloblastic anemia) are:
- Conditions that negatively affect bone marrow (myelodysplastic syndromes)
- Breaking down of red blood cells before their normal lifespan is over (hemolytic anemia)
- Blood clotting disorder that can lead to small blood clots throughout the body (thrombotic thrombocytopenic purpura)
There can be other reasons for B12 deficiency:
- Problem with the body’s ability to absorb B12 from food (food-cobalamin malabsorption)
- A vegan diet that lacks B12
- Certain medications like metformin, proton pump inhibitor therapy, and estrogen contraceptive pills
- Operations on the stomach or the part of intestine (ileal resection) that absorbs B12
- Diseases affecting the part of the intestine that absorbs B12 (ileal disease)
Additional causes for an increased number of large red blood cells (macrocytosis):
- Lack of folic acid (folate deficiency)
- Use of a medication to treat cancer, psoriasis, and rheumatoid arthritis (methotrexate)
- Alcohol addiction (alcohol use disorder)
Other possible reasons for nerve damage in the hands and feet (peripheral neuropathy):
- High blood sugar conditions like diabetes mellitus
- Condition that puts pressure on the nerve in the wrist (carpal tunnel syndrome)
- Infections or certain medications
- Deficiencies of other necessary vitamins
- Excessive alcohol use (alcohol use disorder)
What to expect with Pernicious Anemia
Before scientists figured out how to treat it, pernicious anemia usually resulted in death. These days, with the right treatment, people with pernicious anemia usually do very well, except if they also have another condition call SCD. While getting extra Vitamin B12 can slow down the disease and help with nervous system problems in most SCD patients, full recovery isn’t common.
Typically, after starting treatment for pernicious anemia, the body starts to produce new young red blood cells in about 5 days. Then within 4 to 6 weeks, the overall number of red blood cells should get back to normal. However, it usually takes longer for neurological symptoms like issues with movement or sensation to get better. The more severe and long-lasting these symptoms were before treatment, the less likely they are to fully recover. On the other hand, psychiatric symptoms such as emotional instability and psychosis may improve quickly.
Possible Complications When Diagnosed with Pernicious Anemia
If you have pernicious anemia, you may have a higher risk of developing stomach cancer. In a global study of over 22,000 patients, approximately 0.27% developed stomach cancer each year. The same study also reported that the recurrence rate of stomach cancer in these patients was around 6.8%.
An extensive study in the United States found that pernicious anemia patients also had an increased risk of 10 different types of cancer. The most notable increase in risk was found for a type of stomach cancer known as gastric carcinoid tumors. Catching pernicious anemia 6 or more years after diagnosis resulted in a staggering 11-fold increase in these specific tumors’ risk. Regardless, it’s important to note that gastric carcinoid tumors are rare, making up only about half a percent (0.5%) of the total 17,076 cases in the study.
Several recommendations have been proposed to manage pernicious anemia:
- The British Society of Gastroenterology (2019) proposes that those who are 50 years or older with lab evidence of pernicious anemia should be considered for an initial endoscopy with biopsies. Samples should be taken from the greater and lesser stomach curves, where stomach cancer often develops in those with pernicious anemia. They acknowledge that the evidence for this recommendation is low quality.
- The European Society of Gastrointestinal Endoscopy, European Helicobacter and Microbiota Study Group, European Society of Pathology, and Sociedade Portuguesa de Endoscopia Digestiva (2019) suggest that patients with pernicious anemia may benefit from endoscopic exams every 3 to 5 years. But, they also mention that the evidence supporting this recommendation is relatively weak.
- The American Gastroenterological Association (2021) encourage healthcare providers to recognize pernicious anemia as a late-stage symptom of autoimmune gastritis. This usually comes with vitamin B-12 deficiency and macrocytic anemia. If a patient is newly diagnosed, they should have an endoscopy with biopsies to confirm and to rule out any potential tumors.
Preventing Pernicious Anemia
Patients need to be informed not just about their treatment, but also how their condition increases their risk for cancer, particularly stomach cancer. It’s important to make them understand the relationship between pernicious anemia and other disorders that the body’s immune system attacks. The doctor should discuss the best way to take vitamin B12 supplements with the patient, as this needs to be taken for life.
If a patient opts for oral therapy, it’s crucial to highlight the difference between this and other optional self-supplements. For those who decide on injections, they may need training on how to inject themselves. Patients sometimes stop taking their treatment when they start feeling better, which is why continuous education is necessary.
By regularly updating patients about their condition and the treatment, doctors increase the chances of patients sticking to what’s needed for lifelong management of pernicious anemia. It’s also key to teach patients about the signs of other autoimmune disorders and stomach cancer. Spotting these conditions early means quicker treatment and better chances of recovery.