What is Ocular Surface Squamous Neoplasia?
Ocular Surface Squamous Neoplasia (OSSN) is a condition that can easily be mistaken for common eye surface disorders such as pinguecula (yellowish patches on the eye), pterygium (growth of pink, fleshy tissue on the eye), conjunctival granulomas (small, inflamed lumps on the eye), and cysts. It’s crucial not to ignore OSSN as it can cause serious eye and general health problems. The condition was first identified in 1860 by Von Graefe and has since been thoroughly researched, significantly improving treatment methods.
OSSN can affect only the conjunctiva (a clear tissue covering the front of the eye and inside of the eyelids), only the cornea (the clear, front surface of the eye), or start in the conjunctiva and spread over the cornea. The range of diseases related to OSSN includes from mild conditions called Conjunctival Intraepithelial Neoplasia (CIN), to more serious ones like squamous cell carcinoma, a type of skin cancer.
These diseases are categorized in two ways: non-invasive and invasive types. The term CIN was first used by Pizzarello and Jakobiec, falling in line with how gynecological tumors are named. They divided CIN into mild, moderate, and severe dysplasia, based on how much of the conjunctiva is affected. Mild dysplasia affects less than one-third, moderate affects up to two-thirds, and severe affects the full thickness of the conjunctiva.
Lee and Hirst were the first to suggest a classification for all OSSN cases, including:
– Benign OSSN: conditions that are not harmful, such as pseudotheliomatous hyperplasia, benign hereditary intraepithelial dyskeratosis and, papilloma
– Preinvasive OSSN: conditions such as conjunctival/corneal intraepithelial neoplasms grades I–III that have not yet invaded the surrounding tissues
– Invasive OSSN: conditions that have spread to surrounding tissues, such as squamous carcinoma, mucoepidermoid carcinoma
What Causes Ocular Surface Squamous Neoplasia?
The development of OSSN, or Ocular Surface Squamous Neoplasia, is influenced by multiple factors. Research has linked it to the human papillomavirus (HPV), exposure to ultraviolet B light (UVB), human immunodeficiency (HIV) viruses 1 and 2, and Hepatitis B and C. Other factors that increase the risk of OSSN include chronic smoking, use of petroleum products, having light-colored hair and eyes, vitamin A deficiency (which can lead to a condition called xerophthalmia), exposure to certain chemicals like arsenic and beryllium, injury to the eye’s surface, and being from certain high-risk geographic locations such as Britain, Austria, and Switzerland.
Another factor can be a failure in the body’s DNA repair system, as seen in a condition called xeroderma pigmentosa. This failure, linked with OSSN, can be triggered by UVB rays, which can cause mutations in a gene called p53. Some studies have found high levels of a substance called nuclear p53 in people with OSSN. Additionally, certain features, such as fair skin, light-colored iris, and a history of severe sunburns, were indicated as potential risk factors for OSSN.
Certain strains of HPV, specifically HPV 6 and 11, have been found to cause conjunctival papilloma and other abnormalities and cancers of the eye’s surface. Other strains, HPV 16 and 18, have been closely linked with CIN, which stands for Cervical Intraepithelial Neoplasia, another type of pre-cancer.
Risk Factors and Frequency for Ocular Surface Squamous Neoplasia
OSSN, also known as ocular surface squamous neoplasia, has different rates of occurrence based on location. Some studies have found that OSSN occurs in different proportions around the world such as 0.13 per lakh of population in Uganda, less than 0.2 cases per million per year in the United Kingdom, and 1.9 cases per 100,000 population in Brisbane, Australia. It appears to mostly affect white people, about 90 to 100%. In some countries including Africa, OSSN occur equally among males and females.
Another study showed that people with darker skin, living near to the equator in tropical climates, are five times more likely to get OSSN. It was also discovered that the incident of squamous cell carcinoma, a specific type of OSSN, reduces by 49% with every 10-degree difference in latitude. OSSN incidents are most frequently reported in older males (approximately 80%).
- The average age of an OSSN diagnosis is 56 years old, varying from 4 to 96 years old.
- The average age of occurrence of carcinoma, a type of OSSN, is 5 to 9 years younger than intraepithelial neoplasia.
- OSSN is reported often in white males living close to the equator who are in their 60s and 70s. However, in Asia, it is more frequently seen in younger people with HIV and xeroderma pigmentosa.
- OSSN represents about 4 to 29% of all ocular-orbital tumors.
- OSSN is the third most common tumor after melanoma and lymphoma.
Signs and Symptoms of Ocular Surface Squamous Neoplasia
OSSN, short for Ocular Surface Squamous Neoplasia, is a type of eye condition where patients usually find themselves dealing with a mass or lump in the eye that can cause irritation, redness, a sensation similar to having a foreign object in the eye, itching, and sometimes, less clear vision. This condition affects the clear layer of the eye and can slowly grow over the limbus and cornea. There are rare cases where a person can have this condition in both eyes or have multiple masses.
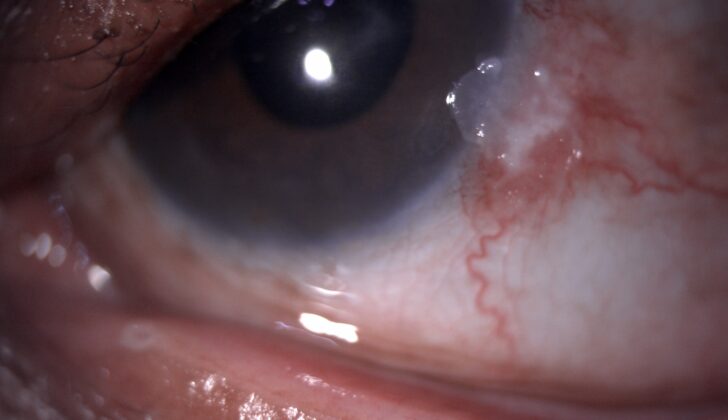
OSSN presents itself as a grey white lesion that’s raised and has irregular borders. There’s usually a noticeable blood vessel associated with it, often referred to as the sentinel or feeder vessel.
OSSN comes in different forms, including:
- Papillomatous: This benign or non-cancerous form of OSSN is pink to cherry red, similar to a strawberry in looks, and the redness is due to a vascular core in the middle of the lesion. It can appear differently in children and adults.
- Leukoplakic: This type of OSSN has a thick, whitish surface due to surface hyper-keratinization and is considered a stage before becoming invasive.
- Gelatinous: This type has a circumscribed, artery-like configuration and is slow-growing. It can be divided into nodular and diffuse types.
In terms of corneal OSSN (involving the clear front surface of the eye), the appearance is typically mottled, translucent, opalescent and has defined borders. These are slow-growing, indolent, known for recurrence, and are usually due to the spread of abnormal cells from the nearby limbus. There are also cases of squamous cell carcinoma and Mucoepidermoid carcinoma, which can be more aggressive variants and mimic the appearance of OSSN.
Testing for Ocular Surface Squamous Neoplasia
Exfoliative cytology and impression cytology are two methods used to collect cells to diagnose eye surface cancers. The first technique, exfoliative cytology, is performed with a specific brush to collect cells that are not adhering well to each other and are shedding off the surface of the mucous membrane. This is a common phenomenon with cancer cells.
The second technique, impression cytology, involves using a cellulose acetate paper. This method is not only simple and affordable but also offers the advantage of maintaining the original arrangement of the cells. This method is often used for surface biopsies when eye surface cancer is suspected. Studies have shown that there’s about an 80% match between the results obtained from impression cytology and those from traditional biopsies and suspected diagnoses based on the samples taken.
Impression cytology can also be performed using a biopore membrane. The benefit here is that you can store the sample for several days without disturbing the arrangement of the cells. These tests can help identify invasive or non-invasive forms of cancer, and even track the regression of the tumor and how it responds to chemotherapy treatments.
Certain dyes can also be used to assist in the diagnosis of eye surface cancer. This includes rose bengal, toluidine blue, and methylene blue. The rose bengal dye helps identify unhealthy and dead cells, which it stains bright pink. Toluidine blue is particularly effective at staining rapidly dividing cells, which are a common feature of the cancer mass. Methylene blue dye can easily penetrate cell walls and binds quickly to nucleic acid, making it useful for identifying cancerous cells with a fast metabolism.
These dyes can be particularly useful during surgery to identify the cancerous lesion and the margins for removal. However, it’s important to note that these dyes have high sensitivity but low specificity, which means they can also stain other pathologies with abnormal epithelium.
Finally, technologies like anterior segment optical coherence tomography (ASOCT) and confocal microscopy offer additional methods for diagnosing eye surface cancer. ASOCT provides high-resolution imaging, making it easier to visualize the tumor and distinguish it from normal tissues. This technology can also provide information about any thickening of the epithelial tissue, activity within the epithelial tissue, and the depth of the tumor.
Confocal microscopy is another technique for evaluating eye surface cancer. Despite its limited availability, this method is a straightforward and safe technique for early diagnosis, follow-up, and evaluating the likelihood of recurrence of eye surface cancer. This technology can also gauge the effectiveness of topical chemotherapy treatments.
In some cases, especially with squamous cell carcinoma, high-frequency ultrasound could be used to determine the extent of the cancer’s invasion into the eye.
Treatment Options for Ocular Surface Squamous Neoplasia
The goal of treatment for ocular surface squamous neoplasia (OSSN), a type of eye cancer, is to get rid of the tumor, prevent it from coming back, preserve eyesight, and avoid any complications. Previously, the standard treatment for OSSN was surgical removal. However, recent advancements in medical treatments have provided doctors and eye specialists with more options.
Medical Treatment
There are two subdivisions in medical management – chemotherapy and therapy involving the immune system, also known as immunotherapy.
Chemotherapy has many benefits. It allows the whole eye surface to be treated at once, so there’s no need to worry about getting clear tissue margins like in a surgical biopsy. It also specifically targets the tumor cells, reducing the risk of damage to the limbal stem cells, and it offers a simpler, cost-effective solution and is a beneficial option for recurrent cases. Its limitation is that it might not penetrate deeply enough in cases of invasive squamous cell carcinoma.
Two main chemotherapeutic agents used include Mitomycin C (MMC) and 5 Fluorouracil (FU). They work by interfering with DNA synthesis, disrupting cell growth, and causing cell death.
Immunotherapy
Interferon Alpha2b (INF-alpha2b) is an immunotherapeutic agent used for OSSN treatment. It is a naturally occurring protein that affects cell growth and has anti-viral and anti-tumor activity. It has been suggested for OSSN treatment due to its potential effectiveness against human papillomavirus (HPV), which is thought to be linked to OSSN. Pegylated Interferon Alpha 2b, a version of Interferon Alpha 2b that stays in the body longer, has also shown promise in treating OSSN with minimal side effects.
Radiotherapy
Radiotherapy, using radiation to kill cancer cells, was previously used for OSSN treatment but is not used as much now due to its side effects and complications.
Surgical Treatment
Surgical removal remains the gold standard for OSSN treatment as it can confirm the diagnosis and kick-start medical therapy. However, it comes with a risk of recurrence. The recommended surgical technique for effective OSSN removal involves a ‘no-touch’ technique, involves removing the tumor without directly touching it, minimising the risk of spreading the tumor cells. After removing the tumor, the residual defect can be closed using a variety of methods depending on the size of the defect.
Cryotherapy
Cryotherapy, a technique that uses freezing temperatures to destroy residual tumor cells, may also be used during surgery.
Enucleation and Exenteration
In rare instances where the cancer has spread within the eye or to the eye socket, procedures to remove the eye (enucleation) or eye and surrounding tissues (exenteration) may be necessary.
Current Therapeutic Strategy
The current recommended treatment depends on the size of the tumor. For smaller tumors, the advice is complete excision biopsy, followed by regular check-ups. Larger tumors may require an initial treatment to reduce the tumor size, followed by surgical removal. In some cases, chemotherapy is recommended, followed by a rigorous schedule of follow-ups to ensure the absence of recurrence.
What else can Ocular Surface Squamous Neoplasia be?
There are various conditions that appear similar to each other. These can be:
- Actinic keratosis (Sun-induced skin damage)
- Benign intraepithelial dyskeratosis (noncancerous skin disorder)
- Conjunctival/tarsal cyst (A cyst in the eye)
- Conjunctival haemangioma (A cluster of blood vessels in the eye)
- Keratoacanthoma (skin condition that causes small, benign tumors)
- Malignant melanoma and nevi (skin cancer and moles)
- Pannus (abnormal growth of tissue)
- Pinguecula (A yellowish patch or bump on the white of the eye)
- Pterygium (growth of the conjunctiva or mucous membrane)
- Pseudoepitheliomatous hyperplasia (a rapid growth of cells in the skin surface)
- Pyogenic granuloma (noncancerous skin growth)
- Xerophthalmia (dry eyes due to Vitamin A deficiency)
What to expect with Ocular Surface Squamous Neoplasia
Generally, the outlook is positive for patients with OSSN (Ocular Surface Squamous Neoplasia – a type of eye tumor) where the cancer has been thoroughly removed, as the chances of it returning are quite low. However, the odds of the cancer returning can increase due to several factors, including incomplete removal of the tumor, older age, deep penetration of the cancer into tissues, OSSN that impacts the cornea (the front part of the eye), and larger tumors (those bigger than 2 mm).
In these more complicated cases, the outlook is more uncertain. Recent advances in both medical treatments and surgeries have proven effective. Only 5% of cases are reported to come back locally, and less than 2% spread to the lymph nodes. More aggressive types of cancer, like invasive and mucoepidermoid carcinoma (another type of cancer), tend to have a poorer outlook.
Possible Complications When Diagnosed with Ocular Surface Squamous Neoplasia
Medical complications you could experience include:
- Drug toxicity, which is when your body reacts negatively to a medication
- Keratitis, an inflammation of the cornea
- Scleral melt, a condition that causes a thinning of the white part of your eye
- Sclerokeratitis, an inflammation involving both the white part of your eye and the cornea
Surgical complications are also possible, such as:
- Recurrence, where the issue comes back after treatment
- Scleral necrosis, a condition where the white part of your eye undergoes tissue death
- Scleral melt, which again refers to thinning of the white part of your eye
- Dellen, which are small, shallow dents in the cornea
- Corneal thinning, a condition where the clear, front layer of your eye becomes thin
- Corneal perforation, a serious condition where there’s a hole in the cornea
Recovery from Ocular Surface Squamous Neoplasia
After having an excisional biopsy, which is a surgical removal of a piece of tissue, patients are typically treated with topical steroids and lubricants in slowly decreasing doses. The drug Mitomycin C, generally in a strength of 0.02 to 0.04%, is started on a cycle of one week on and one week off, but only once the histopathological diagnosis has confirmed Ocular Surface Squamous Neoplasia (OSSN), an eye condition that involves changes to the cells on the surface of the eye.
Following the patient’s treatment, consistent check-ups are necessary to look for any signs of return of the condition, or health issues as a result of chemotherapy drugs. The ophthalmologist, who is an eye doctor, along with optometrists (eye specialists) and nurses, plays a vital role in the patient’s recovery and improving the appearance of their eye.
It’s also important that patients understand the potential side effects of the prescribed treatments which include topical steroids (medications applied to the skin), chemotherapy (drugs used to kill or slow growth of cells), and immunotherapy (treatment that uses your body’s immune system to fight diseases) and report any complications to their eye doctor.
Preventing Ocular Surface Squamous Neoplasia
All patients should be informed about the necessity of surgery and specific medical treatments. They need to understand that the removed mass might be a surface tumor which requires appropriate and prompt treatment. It’s crucial for patients to regularly return for check-ups after the surgery.
Furthermore, OSSN, which is the condition they have, is often linked to HIV, HPV and Hepatitis B. Therefore, blood tests are necessary and this should be made clear to the patient. Patients also need to be made aware of the importance of avoiding direct, excessive sunlight and to understand the potential side effects of their medical treatment.
Lastly, the patient needs to know that this condition, OSSN, usually has a positive outlook, and most patients have good outcomes.