What is Osteoradionecrosis?
Using radiation to treat cancers has been a lifesaving technique for the past 50 years. However, a small group of patients who have radiation treatment for head and neck cancers might get osteoradionecrosis (ORN) in the jaw. ORN simply means the death of bone tissue due to radiation exposure. Most patients who receive more than 6000 units (cGy) of radiation, run a 9% risk of developing ORN in the mandible, specifically the lower part of the jaw.
On a brighter note, the advent of a newer radiation technique known as intensity-modulated radiation therapy (IMRT) has shown a lesser occurrence of ORN in the mandible. Some of these patients tend to develop what we call ‘exposed intraoral mandibular bone’. This may sound complicated but it simply means that the bone in the lower jaw becomes visible inside the mouth. But don’t worry, many of these patients recover naturally without any complications. However, a few might develop bone infection (osteomyelitis), fractures of their lower jaw, and in severe cases, tissue in their mandible might die.
Increasingly, hyperbaric oxygen treatment is being used as a key treatment for osteoradionecrosis. This involves breathing pure oxygen in a pressurized room or tube which can encourage the healing process. Encouragingly, a team including oral maxillofacial surgeons, dentists, undersea and hyperbaric medicine specialists, infectious disease specialists, and radiation oncologists can coordinate well to provide the best treatment for patients who develop ORN as a consequence of radiation treatment. To achieve the best recovery results, hyperbaric treatments should be given along with appropriate surgical cleaning (debridement) of the affected area, as well as the use of antibiotic therapy targeted according to culture tests.
What Causes Osteoradionecrosis?
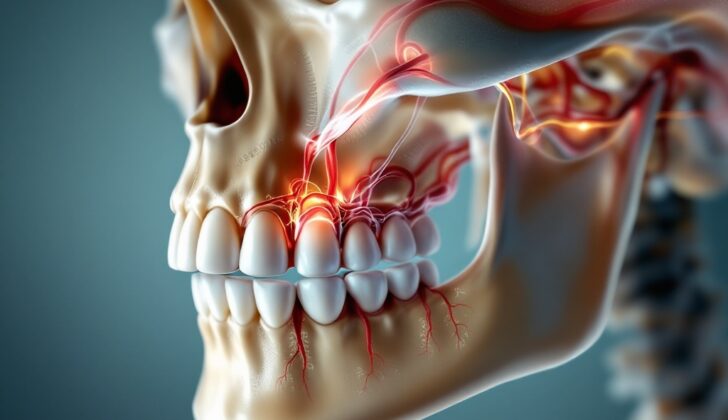
Osteoradionecrosis of the jaw (ORN) is a condition that can occur much later after radiation therapy has been done. Basically, it happens when tissues in the head and neck that have been exposed to radiation become less blood-rich and less oxygenated.
If the lower jaw (the mandible) is part of the area that received radiation, it may develop a type of damage called aseptic, avascular necrosis. This is a condition where bone tissues die off because they lack blood supply. This can potentially lead to infections, tooth loss or even a break or fracture in the jaw.
Osteoradionecrosis is not often seen in patients who received less than 6000 centiGrays (cGy) of radiation – to give context, a centiGray (cGy) is a unit used to measure radiation dosage. This condition might arise several years or even decades after the conclusion of the radiation treatment.
Risk Factors and Frequency for Osteoradionecrosis
Osteoradionecrosis is a condition that can occur after radiation treatment for head or neck cancer. About 9% of the patients who receive a very high dose of radiation (more than 7000 cGy) will develop this condition, while only 2% of those who receive 6000 to 7000 cGy will experience it. Almost no patients receiving less than 6000 cGy will get osteoradionecrosis. This condition can also occur if a tooth is removed from an area that previously received radiation, particularly in the lower jaw.
People who get osteoradionecrosis are usually over the age of 55. Additionally, up to one fifth of patients with severe osteoradionecrosis that doesn’t improve with treatment have bone damage resulting from recurring cancer or a secondary tumor caused by the initial radiation treatment.
Signs and Symptoms of Osteoradionecrosis
A thorough examination of the mouth is needed, using tools like a dental mirror and a tongue depressor. The examination focuses on:
- Checking the condition of the teeth, noting any missing teeth or those that may need to be removed.
- Inspecting the tongue and gums.
- Measuring and recording any exposed bone.
- Documenting any unusual channels or holes, known as sinuses or fistulae.
- Feeling the lymph nodes around the neck, behind the ears, and under the arms, and documenting the findings.
In addition to the physical examination, the following medical histories should also be documented:
- The schedule and dosage of any radiation therapy, which should be verified with the radiation oncologist.
- Any chemotherapy given, along with the start and end dates.
- Presence of conditions such as xerostomia (dry mouth), dysphagia (difficulty swallowing), dysphonia (voice disorder), and ageusia (loss of taste).
Testing for Osteoradionecrosis
If your doctor suspects that you might have a condition called osteoradionecrosis (ORN) of the jaw, they will likely want to look at images of your jaw. These could include X-rays, panorax images (a type of X-ray that shows a wide view of the jaw), or scans from a computed tomography (CT) machine (which makes detailed pictures of the inside of the body) or a magnetic resonance imaging (MRI) machine (which uses strong magnets and radio waves to create detailed images of the inside of your body).
There are no specific lab tests that can tell if you have ORN. The best way to know for sure is with a biopsy, where a small piece of the affected tissue is removed and examined under a microscope. However, your doctor may ask you to do a couple of blood tests as well. For example, they might test for sedimentation rate (a test that measures how quickly red blood cells fall to the bottom of a test tube – if they fall quickly, that could suggest inflammation in the body) and C-reactive protein (a substance produced by the liver in response to inflammation). Both of these are usually higher if you have osteomyelitis, an infection in the bone.
Treatment Options for Osteoradionecrosis
Osteoradionecrosis is a condition that happens when tissues and bones are damaged due to radiation exposure. This can result in an area of bone that loses blood supply and ‘dies’. Treating osteoradionecrosis requires a team of specialists from fields such as surgery, infectious diseases, radiology, and hyperbaric medicine. They work together to develop an effective approach to treatment – if they worked separately, the treatment may not be successful.
The first step in treating osteoradionecrosis is to determine how advanced the condition is, which can be done using what’s known as a ‘staging system’. The staging system helps doctors to decide on the best treatment options, which can involve a combination of surgery and hyperbaric treatments depending on the stage. Hyperbaric treatment involves breathing pure oxygen in a pressurized environment, which can increase the amount of oxygen that reaches the body’s cells and tissues, promoting healing. With all cases of osteoradionecrosis, it’s important to remove all affected or ‘dead’ bone.
For more advanced cases, additional treatments such as pentoxifylline and tocopherol (referred to as ‘PENTO treatment’) may be beneficial. These are medicines that can improve blood flow and reduce inflammation.
The staging system for osteoradionecrosis was developed by Robert Marx. It describes the severity of the condition in the mandible (lower jaw bone) and guides treatment options:
– Stage I: This stage is characterized by exposed bone that has been there for a while or has developed quickly. The standard treatment is 30 hyperbaric treatments before surgery followed by a bone debridement surgery (which is a process to remove dead or damaged tissue) with another 10 hyperbaric treatments afterwards.
– Stage II: Patients in this stage do not respond well to 30 pre-surgery hyperbaric treatments, or they require a more intensive debridement surgery. The goal of surgery for stage II osteoradionecrosis is to preserve as much of the mandible as possible. If it’s anticipated that a portion of the mandible needs to be removed, the patient is usually moved to Stage III.
– Stage III: Patients in this stage, including those progressed from stages I and II, would need to have part of the mandible surgically removed and have severe prognosis, like pathologic fracture, percutaneous fistulae (an abnormal connection between an artery and a vein), and lytic lesions (areas of bone damage) extending to the lower part of the mandible. The standard treatment for stage III patients includes removing all the dead bone through debridement. They are also given 30 hyperbaric treatments before surgery and 10 treatments afterwards.
What else can Osteoradionecrosis be?
When evaluating a condition called osteoradionecrosis, healthcare providers have to consider several possible diagnoses:
- The original cancer may have recurred or a new tumor could have developed because of the radiation therapy.
- Osteomyelitis, an infection of the bone, could also be present and would need to be treated with antibiotics.
- A bone disease called Bisphosphonate related osteonecrosis of the jaw may be the issue. This condition is a known side effect of a certain medication, so a thorough review of the patient’s medical history can help rule this out.
What to expect with Osteoradionecrosis
Patients who were first treated with antibiotics, hyperbaric oxygen therapy (a treatment where you breathe pure oxygen inside a pressurized room), and surgical removal of damaged tissue typically saw positive results. Those suffering from severe osteoradionecrosis of the jaw, which is a severe bone disease often caused by radiation therapy, and do not respond well to standard treatment methods might be treated with pentoxifylline and tocopherol therapy. Reports show that this treatment method results in a full recovery or significant improvement in 60% of cases.
Possible Complications When Diagnosed with Osteoradionecrosis
Osteoradionecrosis – a severe complication from radiation therapy – can lead to serious issues such as:
- Sores and dead tissue in the mouth’s lining with exposed bone. This condition can generally cause infection and bone decay.
- Exposed bone could irritate nearby soft tissues in the mouth.
- The bones might become fragile and could fracture easily.
- Fistulae, or abnormal connections between tissues, can develop. These are usually a sign of a spreading local infection. If not treated properly, this can lead to systemic infections that can affect the whole body and possibly cause sepsis, a life-threatening condition.
Preventing Osteoradionecrosis
Osteoradionecrosis, a condition where the bone gets damaged due to radiation treatment, is less common now than before, but it’s still a potential side effect of treating conditions in the head and neck area with radiation. It’s important for doctors to explain this to patients before they decide on using radiation therapy. Reducing the amount of radiation used can help lower the risk of this happening. If this side effect does occur, quick medical attention allows doctors to start treatment quickly, which can cut down on further complications.