What is Juvenile Xanthogranuloma ?
Juvenile xanthogranuloma (JXG) is a condition that is relatively common in kids, making it the most common kind of a group of diseases known as non-Langerhans cell histiocytic disorders during childhood. It often shows up during a child’s first year of life – in fact, around 75% of cases appear at this time. Also, about 15-20% of babies already have this condition at birth. JXG is quite uncommon in adults, and it typically appears between the late twenties and thirties.
Some adults get this condition, but usually, they only have one lesion (a patch of damaged tissue). However, many cases might not be diagnosed because the lesions can be single and small. In up to 90% of all cases, these could go unnoticed. These lesions often looks like solitary or groups of firm yellow, orange or brown spots or small raised lumps.
The most common places where these lesions appear are the face, neck, and upper body. Inside the mouth, these lesions are pretty rare but when they do appear, they typically show up as yellow bumps on the sides of the tongue. They also occur on the gum, inner cheek skin, and in the center of the roof of the mouth — and these may break open and bleed. Skin lesions from JXG usually don’t cause any symptoms, and most of them get better on their own over a few years.
Although it’s quite rare, the most common places outside of the skin where JXG can occur are the eyes and then the lungs. Affects on the eye generally happens in one eye and in less than 0.5% of patients. About 40% of people with this form of JXG have multiple skin lesions at the time they’re diagnosed. Eye disease usually occurs before 2 years of age and most often affects the iris — the colored part of the eye. Serious complications, such as blood-filled swelling in the eye (hyphema) and increased pressure in the eye (glaucoma), can lead to blindness and require prompt referral to an eye doctor for examination and potential treatment. However, factors like other bones and internal organs or the central nervous system (such as causing a type of diabetes call diabetes insipidus) being affected is really rare. Also, it’s very rare that this disease could cause death. And unlike other similar diseases, juvenile xanthogranulomas are not related to metabolic or fat disorders.
What Causes Juvenile Xanthogranuloma ?
It is believed that juvenile xanthogranulomas or flesh-colored skin lumps in children occur due to unknown triggers, which could be anything from infections to physical factors. These triggers cause a certain type of inflammation and accumulation of cells in the tissues, known as a granulomatous histiocytic reaction. However, what exactly causes juvenile xanthogranulomas is not yet clear. As a result, doctors generally recommend a wait-and-watch approach.
Juvenile xanthogranulomas have been linked to a type of blood cancer called juvenile chronic myelogenous leukemia (JMML). This leukemia is also found in patients with an inherited disorder known as neurofibromatosis, which affects the growth and development of nerve cell tissues. While it’s rare, some patients may have both juvenile xanthogranulomas and neurofibromatosis. If this is the case, these children have a much higher chance – 20 to 32 times greater – of getting juvenile myelomonocytic leukemia than patients with only neurofibromatosis.
Some other conditions linked to juvenile xanthogranulomas include urticaria pigmentosa (a skin disease causing reddish-brown spots), insulin-dependent diabetes mellitus (a form of diabetes where the body needs insulin daily), aquagenic pruritis (skin itch caused by water contact), and even a type of viral infection known as cytomegalovirus (CMV).
Risk Factors and Frequency for Juvenile Xanthogranuloma
Juvenile xanthogranulomas mostly appear during early childhood, with 15-20% of patients having these lesions at birth. In about 75% of cases, these spots show up during the first year of a child’s life. In contrast, around 10% of cases occur in adulthood, known as adult xanthogranulomas. Among children, this condition more commonly affects boys, but among adults, it’s equally common in both men and women.
Signs and Symptoms of Juvenile Xanthogranuloma
Juvenile xanthogranuloma, a type of skin condition, typically shows up in two ways. The first form involves many small dome-shaped bumps that start off pink or reddish-brown and eventually turn yellow. These bumps are between 2 to 5 millimeters in size. The second form involves one or more large nodules that are between 1 to 2 centimeters. There are also some other less common types, like giant juvenile xanthogranuloma, atrophic plaque, cutaneous horn, and subcutaneous mass instances.
This condition can sometimes progress to a more serious form, called systemic juvenile xanthogranulomas, which happens in about 4% of kids. Unfortunately, this severe form can be fatal due to effects on the brain or liver, resulting in death in 5% to 10% of cases. Moreover, juvenile xanthogranulomas can also impact areas outside the skin, like the eyes, leading to issues such as bleeding within the eye, glaucoma, or even blindness. This especially happens in young children under 1 year of age. Specifically, the iris of the eye is most commonly affected. The common sign of this condition in the iris is spontaneous hyphema, which means bleeding in the eye, sometimes accompanied by high pressure inside the eye.
Besides eye problems, other complications related to the brain can include seizures, high pressure inside the skull, a type of diabetes insipidus, and delayed development. Juvenile xanthogranulomas can also affect other parts of the body such as deeper soft tissues, spleen, and lungs.
Testing for Juvenile Xanthogranuloma
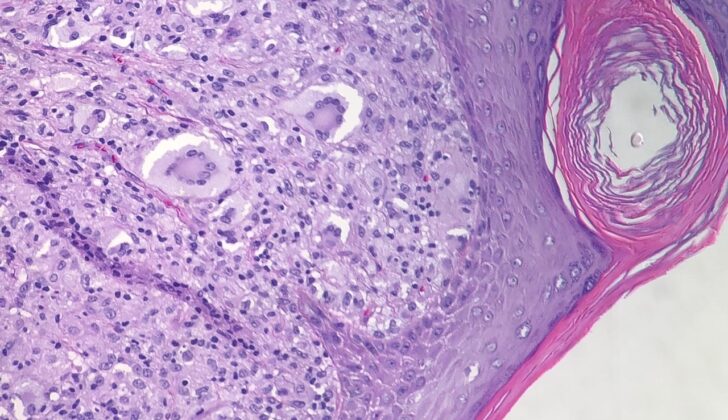
Dermoscopy is a technique that doesn’t involve breaking the skin or entering the body, often used to help diagnose a condition known as juvenile xanthogranuloma. This technique often shows a unique pattern that resembles a setting sun (a red and yellow center with a distinct red halo around it). The final confirmation of the diagnosis normally comes from completely removing the affected area through surgery.
Treatment Options for Juvenile Xanthogranuloma
If you have a skin condition that can be easily reached, doctors may choose to remove it entirely as a form of treatment. But don’t worry, most skin issues children face tend to heal on their own with time and often don’t need any specific treatment.
If the issue is inside your body (non-cutaneous), the situation could be a bit trickier. The treatment can involve a combination of operations, drug treatments (chemotherapy), radiation treatment (radiotherapy), or medications that weaken the immune system (immunosuppression). These treatments are typically considered for patients with disease symptoms that cannot be completely removed by surgery or are not appropriate for surgery.
If you also have Neurofibromatosis type 1 (NF-1), a genetic disorder that causes tumors to form on nerve tissue, your doctor will want to see you often. During these visits, they will likely run blood tests to monitor for juvenile chronic myelogenous leukemia (JMML), a rare type of blood cancer typically found in young children.
It’s also advised that high-risk patients get regular eye exams. If the disease affects your eyes, different types of steroid medications could be given to minimize inflammation. Sometimes complications can arise, such as increased eye pressure (glaucoma) or blood in the clear front part of the eye (hyphema). If that happens, surgery or system-wide steroid medications may be necessary.
What else can Juvenile Xanthogranuloma be?
If your doctor suspects a juvenile xanthogranuloma, they might look at other benign (not harmful) or malignant (harmful) conditions to rule out, depending on the symptoms and the affected location.
One important consideration is Langerhans cell histiocytosis, which is a condition that can appear similar to juvenile xanthogranuloma. However, certain features can make it distinguishable. For example, Langerhans cell histiocytosis usually has cells with grooved nuclei that have a coffee bean-like appearance. Certain types of protein markers (CD1a and S-100) would be found in Langerhans cell histiocytosis, but not in juvenile xanthogranuloma.
Another condition to bear in mind is reticulohistiocytoma, another disorder that can resemble juvenile xanthogranuloma. This condition usually presents with large immune cells and fibrous tissue in the skin. Although these cells might test positive for a protein marker known as CD68, they are typically negative for another protein called vimentin, which is different from juvenile xanthogranuloma.
Although juvenile xanthogranulomas may present in uncommon areas, such as the vulva, it is also important to rule out other conditions, like a type of tumor called embryonal rhabdomyosarcoma, which has a similar appearance under the microscope.
Other conditions to consider when making a differential diagnosis might include:
- Other xanthomatous lesions (abnormal tissue growth)
- Mastocytomas (skin tumors)
- Dermatofibromas (benign skin growths)
- Spitz nevus (a kind of mole).
What to expect with Juvenile Xanthogranuloma
Juvenile xanthogranuloma, a type of skin growth in children, usually has a great outcome. Most of these growths naturally disappear on their own over a span of 3 to 6 years. However, if the growth is cosmetically bothersome or threatens vital body functions, treatment can be provided.
Possible Complications When Diagnosed with Juvenile Xanthogranuloma
Juvenile xanthogranuloma (JXG) often comes with little to no complications because it usually heals on its own. In some cases, lesions may be taken out due to aesthetic reasons. Eye lesions are a bit different and typically need treatment. This step is crucial to prevent serious problems like blindness, glaucoma, or hyphema (blood in the eye).
Possible consequences of not treating JXG:
- Blindness
- Glaucoma
- Hyphema