What is Neonatal Jaundice?
Neonatal jaundice is a common condition found in newborns, often seen in the first two weeks after birth. Its main feature is a yellowing of the skin, white parts of the eyes, and mucous membranes due to a higher than normal level of a substance called bilirubin in the blood – a condition known as neonatal hyperbilirubinemia. It is termed “neonatal jaundice” because jaune means yellow in French.
Although this condition affects approximately 60% of full-term babies and 80% of premature babies in the first week after birth, it’s usually mild and goes away on its own – what medical professionals call “physiologic jaundice”. However, there is another, more serious type that should be identified and treated quickly to prevent any risks to the baby’s brain, known as “pathological jaundice”.
There are two different types of hyperbilirubinemia that can lead to jaundice. The most common type is Unconjugated Hyperbilirubinemia (UHB) and the other type, which indicates a more serious underlying health problem, is Conjugated Hyperbilirubinemia (CHB). These types need to be identified to deliver appropriate treatment because failing to treat pathological jaundice may lead to a condition called bilirubin encephalopathy, which can cause harmful effects on the baby’s central nervous system, especially in preterm infants or those with certain inherited conditions that affect how the body processes bilirubin.
To detect these types of hyperbilirubinemia, doctors may use a simple non-invasive device that measures bilirubin in the skin or draw a small amount of blood to measure total bilirubin levels for UHB. CHB is usually identified through additional lab tests, and in some cases, imaging studies. If not treated adequately, severe hyperbilirubinemia can cause a condition known as bilirubin-induced neurological dysfunction (BIND), which can be life-threatening.
The main treatments for UHB include phototherapy (light therapy) and exchange transfusions (replacing the baby’s blood with fresh blood), and in some cases, infusions of a medication called intravenous immunoglobulin (IVIG). The treatment for CHB may be more intricate and dependent on the cause of the jaundice. Despite major improvements in treatment methods, severe jaundice remains a significant health risk for newborn babies, causing disability and death if it’s not managed properly.
What Causes Neonatal Jaundice?
Neonatal jaundice (a yellowing of a baby’s skin and eyes in the first few weeks of life) arises from a condition known as neonatal hyperbilirubinemia, where there is too much bilirubin (a yellowish substance) in a newborn baby’s blood. This condition has two types: unconjugated (or indirect) and conjugated (or direct) hyperbilirubinemia.
Unconjugated hyperbilirubinemia is the most common type and can either be a normal part of a baby’s physical development or a sign of a disease. Around 75% of the time, the elevated bilirubin in a newborn’s blood is part of a normal biological course of events. Newborns typically have higher bilirubin levels compared to adults due to a larger amount of red blood cells and a shorter lifespan of these cells. There’s also a reduced activity of an enzyme (called uridine diphosphate glucuronosyltransferase or UGT) that’s required to process bilirubin, leading to its accumulation in the body. Hence, newborns have more bilirubin in their blood, which can lead to jaundice.
Usually, this jaundice appears 24 hours after birth, peaks at around 48 to 96 hours, and resolves in about 2 to 3 weeks. If the level of bilirubin becomes too high too quickly in the first 24 hours after birth, this signals a disease condition. Unconjugated hyperbilirubinemia can be largely categorized into three types depending on the cause: increased production of bilirubin, decreased clearance of bilirubin, and other reasons.
Increased production of bilirubin can occur due to destruction of red blood cells by the baby’s immune system if it reacts against incompatible blood groups between the mother and the baby or due to defects in the red blood cells. These conditions lead to an excess of bilirubin in the blood, prompting jaundice. Non-immune causes can include certain genetic disorders that affect the red blood cells, leading to their destruction and thus an increased production of bilirubin.
A decrease in bilirubin clearance happens when there are defects in the enzyme responsible for the process. This can occur due to certain inherited conditions like Gilbert syndrome (where the production of this enzyme is reduced) or Crigler-Najjar syndrome (where there is a complete absence or minimal presence of this enzyme, leading to severe jaundice).
Other factors that may cause increased bilirubin levels encompass conditions like congenital hypothyroidism, certain medications and a decreased intake of food due to breastfeeding. Mothers with diabetes also have infants who are at a higher risk of developing jaundice due to unconjugated hyperbilirubinemia.
Conjugated hyperbilirubinemia, also known as neonatal cholestasis, occurs when there’s an impairment in the liver’s ability to process direct bilirubin. This condition is serious and needs immediate attention and treatment. Common causes include infections, blockage of bile flow due to conditions such as biliary atresia and choledochal cysts, genetic disorders like Alagille syndrome and alpha-1 anti-trypsin deficiency, and other factors like parenteral nutrition-induced jaundice, gestational alloimmune liver disease, neonatal hemochromatosis and hypotension.
Risk Factors and Frequency for Neonatal Jaundice
Unconjugated hyperbilirubinemia, which often leads to clinical jaundice, is quite common in newborn babies. In fact, about 80% of both full-term and premature babies are found to have jaundice, but not all of them require treatment as only around 10% need phototherapy. Physiological jaundice, which usually appears after the first day of life, is the most common cause and is responsible for half of the cases. It is also seen that around 15% of babies who are breastfed may experience this type of jaundice for more than 3 weeks.
Noteworthy, severe jaundice, which is generally defined by total serum bilirubin (TSB) levels greater than 25 mg/dL, is quite rare and is seen in only about 1 in 2500 live births. Some of the usual causes for this condition are ABO incompatibility and G6PD deficiency. Interestingly, newborns of Southeast and East Asian descent tend to have higher TSB levels than Black or White infants. It’s also more prevalent in infants living at high altitudes and in the Mediterranean region, especially Greece.
Acute bilirubin encephalopathy, a condition affecting the brain, is diagnosed in roughly 1 in 10,000 live births, while chronic bilirubin encephalopathy is even less common, occurring in about 1 in 50,000 to 100,000 live births. It’s also worth noting that kernicterus, a permanent neurological condition that’s often linked with bilirubin, is reported at higher rates in developing countries.
Lastly, a condition called conjugated hyperbilirubinemia, which is actually less common than unconjugated hyperbilirubinemia, affects approximately 1 in 2500 full-term babies. The most common cause for this type of jaundice during the neonatal period is biliary atresia, which makes up an estimated 25% to 40% of all cases. Other causes can be infections and total parenteral nutrition (TPN) induced cholestasis (inability to release bile). Almost 60% to 70% of patients with this condition will need a liver transplant during their childhood years, making it the most common reason for pediatric liver transplants.
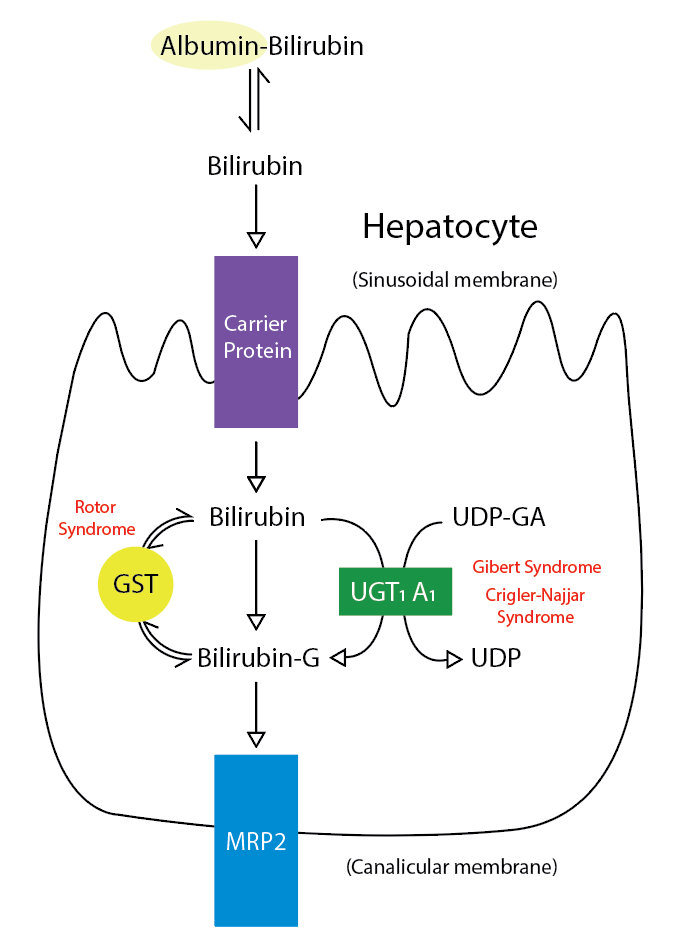
bilirubin glucuronate; the donor is uridine diphosphate glucuronic acid
(UDP-GA). This is catalyzed by the enzyme uridine
diphosphate-glucuronyltransferase (UGT1A1). Gilbert and Crigler-Najjar syndrome
is associated with decreases in UGT1A1 activity. Glutathione-S-transferase (GST)
is a carrier protein that assists bilirubin uptake into the cytosol and may be
implicated in Rotor syndrome.
Signs and Symptoms of Neonatal Jaundice
When a newborn baby develops jaundice, healthcare professionals need to perform a detailed assessment. They’ll look into details about the pregnancy, family health history, the baby’s delivery, when the baby’s symptoms began, how well the baby is feeding, and the mother’s lab test results. The color of the baby’s stool and urine can suggest what type of jaundice the baby might have.
There are minor risk factors related to jaundice in newborn babies, which includes the baby’s bilirubin level being in the higher-than-normal range, the babies’ mothers having diabetes, an abnormally high number of red blood cells, the baby being male, and the mother being older-than-average when the baby is born.
The American Academy of Pediatrics (AAP) recommends all newborn babies be visually checked for jaundice every 12 hours from their birth until they go home. It’s also essential to identify any risks for severe high bilirubin levels. Major risk factors for newborn babies born after 35 weeks include:
- A bilirubin level in the high-risk zone before hospital discharge
- Jaundice in the first 24 hours after birth
- When the baby’s and mother’s blood groups do not match
- When the baby is born earlier than 36 weeks
- Previous experience with phototherapy in an immediate family member
- Bruising after delivery
- Breastfeeding only (not supplemented with formula)
- Asian descent
To check for jaundice, newborn babies should ideally be examined in daylight. However, this method is not always reliable, especially if the baby has been under phototherapy for jaundice, or if the baby has darker skin. In cases like these, a lab test should be run to confirm. Physical signs connected with pathological jaundice may include paleness, small red or purple spots on the skin, bruising, a swollen liver or spleen, weight loss, and dehydration. It’s crucial to observe any signs of bilirubin encephalopathy, such as poor feeding, lethargy, altered sleep, abnormal muscle tone, and seizures. However, keep in mind that up to 15% of babies with this condition display no symptoms initially. If symptoms hint towards neonatal cholestasis, it’s likely that multiple bodily systems are involved, which may indicate the need for further diagnostic tests.
Testing for Neonatal Jaundice
The American Academy of Pediatrics (AAP) recommends checking the bilirubin levels of newborns between 24 and 48 hours after birth to detect a liver function problem called unconjugated hyperbilirubinemia, which causes the skin and whites of the eyes to turn yellow. If the baby leaves the hospital before this time, a bilirubin level test should be conducted before the baby goes home.
Bilirubin levels are typically checked using a device that measures the amount of bilirubin in the skin or through a blood test. Using the device on the skin can sometimes be less accurate in babies with dark skin or in babies who have had light therapy for jaundice. If the result from the device is too high, then a blood test should be done.
To identify if a blood disorder is the cause of the unconjugated hyperbilirubinemia, doctors might check the baby’s and mother’s blood type, complete a full blood cell count, look at the blood under a microscope, and test for a specific glucose enzyme deficiency. To check for bilirubin-related toxicity, a protein called albumin might also be checked, which acts as an indicator for free bilirubin – the type of bilirubin that can cause damage.
Computer images of the brain are usually not needed when diagnosing unconjugated hyperbilirubinemia. However, certain MRI findings in babies with severe bilirubin-induced brain damage (bilirubin encephalopathy) can show changes in the brain’s signals.
In the case of another type of liver function problem called conjugated hyperbilirubinemia, different enzymes in the blood might be checked as they can indicate liver cell injury or blockage in bile channels. Other tests including checking the baby’s blood-clotting ability and albumin level might be done to check how well the liver is functioning. The baby might also be screened for genetic conditions or infections that were present at birth.
Imaging scans like an ultrasound of the liver might be needed to check for blockage of bile, a digestive juice made by the liver. The test can show signs like hardened bile or a condition known as biliary atresia. Another imaging test using a tracer can also show if there is an obstruction causing the bile to build up. On the other hand, liver biopsy is the most accurate method used for diagnosing liver function problems. This test involves taking a small sample of liver tissue for examination under a microscope.
Treatment Options for Neonatal Jaundice
The treatment of newborns with a high level of unconjugated bilirubin, a yellow substance found in bile, involves two main treatments: Phototherapy and exchange transfusion. More treatments may be given depending on the patient’s response. Bilirubin is something the liver should break down, but high levels can cause jaundice (yellow skin and eyes). The method for treating this depends on the risk factors for brain damage, the baby’s age, and the level of bilirubin at a given hour.
Phototherapy (using light to treat a disease) is the first go-to treatment for managing high bilirubin levels. This therapy can reduce bilirubin to safe levels and lower the risk of billirubin toxicity and the need for exchange transfusion. The starting point for this therapy is determined by the risk factors for brain damage, the infant’s age, and bilirubin levels at specific hours.
These risk factors can include infant born before 38 weeks of pregnancy, low levels of a protein in blood called albumin, positive Direct Antiglobulin Test (DAT) or a diagnosis of Glucose-6-phosphate dehydrogenase (G6PD) deficiency, sepsis (body’s response to an infection), and severe deterioration of the patient’s condition in the past 24 hours.
However, for infants born prematurely, there aren’t standardized guidelines for phototherapy and exchange transfusion. Most hospitals devise their own rules based on the birth weight and the number of weeks the baby is.
Phototherapy is most effective when using light in the blue-green range. The therapy involves converting bilirubin into a substance easy to excrete out of the body. The baby’s maximum body surface should be exposed to the light source while the eyes are covered to prevent retinal injury. It’s essential to maintain hydration to ensure good urine output where most bilirubin is excreted. Breastfeeding support should also be provided to prevent dehydration.
Once phototherapy is completed, the total bilirubin level may rise again but is usually lower than the level before treatment. Although considered safe, phototherapy can have some side effects, including rashes, dehydration, low calcium levels, retinal damage, allergic reactions, and a rare condition called Bronze baby syndrome which usually disappears after stopping phototherapy.
Exchange transfusion was the first successful treatment for jaundice and is now the secondary treatment to phototherapy for severe high bilirubin levels. This method involves replacing the baby’s blood with donor blood. Because most bilirubin is located outside of blood vessels, the level of bilirubin after the exchange is approximately 60% of what it was before. After the procedure, they continue phototherapy until the bilirubin level is safe to discontinue it.
Intravenous immunoglobulin (IVIG), a mix of antibodies, helps prevent RBC breakdown. The American Academy of Pediatrics recommends IVIG when the bilirubin level is near the threshold of exchange, despite intense phototherapy.
For conjugated hyperbilirubinemia (where bilirubin is combined with other chemicals), the treatment depends on what caused the jaundice. Cholestasis (blockage in the bile duct system) conditions and severe liver damage may need a liver transplant. In cases of nutrition-induced cholestasis, doctors suggest cyclic parenteral nutrition, start feeding the infants as early as possible, and monitor the contents of parenteral nutrition to minimize liver injury.
What else can Neonatal Jaundice be?
Figuring out why a baby is showing signs of jaundice is complicated work as there are many possible causes. (For a deeper look into this, refer to the Jaundice Causes section). If a newborn baby starts to show signs of jaundice, which is shown by a yellowish skin and eye color, it’s important to figure out quickly if the jaundice is due to a temporary and harmless condition or if it’s a sign of a disease that needs to be treated.
Some older babies and children can have yellowish skin because they are getting too much carotene in their diet. However, this isn’t the same thing as jaundice because their eyes and the inside of their mouth don’t turn yellow, which is a sign of jaundice. Also, this condition is not harmful and babies aren’t born with it.
Just looking at the color of a baby’s skin isn’t a good way to determine if the baby is suffering from a harmful level of jaundice. That’s why it’s important for all newborn babies to be examined for signs of jaundice before leaving the hospital.
What to expect with Neonatal Jaundice
In most cases, unconjugated hyperbilirubinemia – which is an excess of a substance called bilirubin in the blood – can be treated effectively. However, if treatment is delayed or inadequate, it may result in a condition called bilirubin encephalopathy, which is damage to the brain caused by high levels of bilirubin. This condition particularly affects developing countries or places with limited access to medical resources.
In some instances, a serious complication called kernicterus has been making a comeback in countries where it was nearly eradicated. This is mainly due to babies being discharged from the hospital too early and not receiving the necessary follow-up care.
Patients with a certain type of hyperbilirubinemia known as Crigler-Najjar type I face a challenging prognosis and usually require a liver transplant for a complete cure. Without a transplant, they are likely to develop bilirubin encephalopathy.
The outlook for conjugated hyperbilirubinemia – another type of hyperbilirubinemia where the bilirubin is processed differently in the body – depends on what’s causing it. If the cause is a disease called biliary atresia, early diagnosis and surgical intervention within the first two months of life significantly improves the prognosis. Similarly, patients with a disorder called bile acid synthesis disorder (BASD) usually have good outcomes and respond well to medication.
In the past, the prognosis for gestational alloimmune liver disease (GALD) – a disease of the liver in the fetus or newborn caused by immune response from the mother – was often poor, with up to 80% mortality without a liver transplant. However, medical advancements in treatment methods like intravenous immunoglobulin (IVIG) use and double volume exchange transfusion have significantly improved outcomes in recent years.
For most other causes of cholestasis, which is a condition where bile cannot flow from the liver to the small intestine, the prognosis is often less favorable. A multidisciplinary approach involving various healthcare providers might be necessary for these patients.
Possible Complications When Diagnosed with Neonatal Jaundice
Newborns who have an extreme level of bilirubin in their blood, a condition named severe hyperbilirubinemia, are in danger of developing bilirubin-induced brain issues, or BIND. This happens because bilirubin attaches itself to specific areas in the brain, like the globus pallidus, hippocampus, cerebellum, and subthalamic nuclear bodies, and this causes toxicity in neurons.
The first stage of this condition is Acute Bilirubin Encephalopathy (ABE) and the signs include extreme tiredness, weakness, and lack of the usual strength for sucking. It’s important to note that at this stage, it is possible to reverse this condition.
However, left untreated, ABE can become chronic, leading to irreversible brain damage which is also known as kernicterus. Patients that reach this stage start to show signs like uncontrolled and unintended movements, seizures, abnormal body positioning, unusual eye movement, imperfections in dental enamel, and even hearing loss.
Not only does an excessive amount of bilirubin in newborns lead to brain issues, but newborns who have neonatal cholestasis, another liver condition, are also at risk of developing serious liver problems such as liver failure, cirrhosis, and in worst-case scenarios, liver cancer.
Another concern with long-term cholestasis is the stunted growth and deficiencies in fat-soluble vitamins that it can lead to.
Common Health Risks:
- Bilirubin-induced brain issues (BIND)
- Acute Bilirubin Encephalopathy (ABE)
- Chronic and irreversible brain damage (kernicterus)
- Neonatal cholestasis may lead to serious liver problems
- Long-standing cholestasis can cause stunted growth and fat-soluble vitamin deficiencies
Preventing Neonatal Jaundice
In 2022, the American Academy of Pediatrics (AAP) shared new instructions on how to handle newborns with high bilirubin levels (hyperbilirubinemia). The first step in preventing high bilirubin levels happens during pregnancy. Doctors should check pregnant women’s blood type (Rh typing) and treat as needed. If there’s a positive or unknown result in the mother’s antibody test, the newborn will need to have blood tests to find out their blood type and DAT status.
All newborns should be checked for things that could raise their risk of hyperbilirubinemia. They also frequently need to be monitored to prevent severe jaundice, a yellow discoloration of the skin due to high bilirubin levels.
Some of the risk factors for serious hyperbilirubinemia include:
* Being born earlier than 38 weeks
* Having jaundice within the first 24 hours of life
* High bilirubin levels (TSB or TcB) close to the point where light therapy (phototherapy) is needed
* Signs of the destruction of red blood cells (hemolysis) or quickly rising bilirubin levels
* Need for light therapy before leaving the hospital
* A brother, sister, or parent who needed light therapy or a blood transfusion (exchange transfusion)
* Family history of conditions affecting red blood cells, like G6PD deficiency
* Only breastfeeding with not enough intake
* A bruise or swelling on the scalp (scalp hematoma) or significant bruising
* Down syndrome
* A large baby born to a diabetic mother
There are certain risk factors that can make neurological damage from hyperbilirubinemia more likely and lower the level at which the baby would need phototherapy:
* Being born earlier than 38 weeks
* Having less than 3.0 g/dL of albumin (a protein that helps keep bilirubin in the blood) in the blood
* Conditions that cause hemolysis
* Sepsis – an overwhelming body response to infection
* Severe clinical instability from any cause
Since feeding plays a role in the development of hyperbilirubinemia, all breastfeeding moms should receive help to make sure their babies get enough milk. The AAP suggests breastfeeding within the first hour of life, followed by breastfeeding when the baby shows signs of hunger, at least 8 times daily.
Medical staff should check all hospitalized newborns for jaundice visually every 12 hours. They also suggest checking bilirubin levels in all babies before they leave the hospital. Most babies with high levels of bilirubin recover well. Parents should be given information about this condition and the necessary treatment when needed.
Babies with jaundice caused by conditions with poor recovery often need multiple medical consultations. For these families, adequate counseling and support should be provided.












