What is Pediatric Abusive Head Trauma (Head Injury in Abused Children)?
Pediatric abusive head trauma (AHT), also known as shaken baby syndrome (SBS), is a harmful condition that often impacts infants and young children. This brain injury can be caused by shaking, an impact to the head, or a combination of both. Among various forms of child abuse, AHT is the most dangerous and deadly.
This type of head trauma specifically affects children under five years old, resulting from violent shaking or a heavy blow to the head. The consequences can vary greatly – from full recovery to significant brain damage, and even death.
Head and brain injuries are the main cause of trauma-related deaths in children under two years. Early diagnosis can be difficult though, as those responsible often try to hide their actions. Moreover, health professionals might miss some signs and symptoms as they might be internal, with no external indications, making it difficult to determine if the child has been subjected to abuse.
A key approach in preventing AHT is educating caregivers on how to avoid unintentionally causing it and teaching health providers to recognize the sign and symptoms. Mental health care is the best preventive measure to decrease child abuse. Surviving children often endure long-term financial and medical strains.
The individuals who cause harm to these children rarely own up to their abusive actions. They frequently avoid responsibility, fear punishments, and fabricate accidents like falls down the stairs or from a crib, high-chair, or bed.
Clinicians and healthcare providers need to be vigilant when it comes to head injuries in children. If the injuries aren’t apparent, health professionals may miss signs of abusive head injury. Patterns of injuries could indicate AHT or child abuse, so healthcare providers should familiarize themselves with typical injuries from accidents vs. those from abuse.
AHT often involves an injury to the skull or brain of a child under five years old, resulting from violent shaking or a blow to the head. “Abusive head trauma” also encompasses cases where a child is dropped or thrown. It’s essential to be aware that the term describes the injury, not the method of causing it.
If a physician diagnoses a child with “shaken baby syndrome,” it may lead to challenges in court due to precluding evidence of other types of injuries. Abusive head trauma is the biggest cause of death and disability from child abuse in infants and young children. In fact, it was the major cause of brain injuries in a quarter of children older than 2.
When it comes to “shaken baby syndrome,” the term refers to a brain injury consistent with violently shaking an infant or small child. The injuries often include various internal bleeds in the brain and eyes, and severe brain injury. There may also be cases where evidence of a blow to the head is present, hence terms like, “shaken impact syndrome” might be used.
The diagnosis of AHT follows a thorough medical examination and testing and should not rely solely on a set of three common findings.
In conclusion, other terms associated with shaken baby syndrome include nonaccidental head injury (NAHI), inflicted traumatic brain injury (iTBI), nonaccidental head trauma (NAHT), shaken impact syndrome (SIS), and whiplash shaken infant syndrome (WSIS).
What Causes Pediatric Abusive Head Trauma (Head Injury in Abused Children)?
There are several risk factors for abusive head trauma, which can involve the child, family, and caregiver. For example, infants who cry a lot, especially those with colic, are at risk because caregivers who are frustrated may shake them violently. This is most common when babies are between 6 to 8 weeks old and cry the most, which also happens to be when abusive head trauma is most frequent.
Individuals who have a higher risk for causing abusive head trauma include those with mental health issues, those with a history of domestic violence, people who get frustrated easily, inexperienced caregivers, and those who didn’t get prenatal care. Others at high risk include those with low levels of formal education, people from lower socioeconomic backgrounds, single-parent families, and young parents who lack support.
Those who most often cause acute head trauma include the father or stepfather, the mother’s boyfriend, female babysitters, and the mother. Shaking is usually linked to how frustrated or stressed the person is.
Although child abuse affects all ethnic groups, socioeconomic groups, and races, it is more common in boys and teenagers. Babies who are abused are more likely to be seriously hurt or die. Numerous factors can increase a child’s chance of being abused. These can involve individual factors, like a child having a disability, the mother not being married, the mother smoking, and the parent being depressed. Family-level factors include domestic violence in the home and having more than two siblings. Community-level factors include social isolation, lack of recreational facilities, and societal issues like poverty. Other factors can also increase the chance of child abuse such as living with an unrelated adult and having been previously reported to child protective services. However, there are also factors that decrease the risk of child maltreatment, like having supportive family, concerned parents, parental education about child development and parenting, along with social support and parental resilience.
Risk Factors and Frequency for Pediatric Abusive Head Trauma (Head Injury in Abused Children)
Shaken baby syndrome is challenging to diagnose, making its frequency hard to determine. This is due to no centralized reporting system, lack of clear signs of abuse, ambiguous symptoms, and the fact that severe head injuries often occur as part of ongoing neglect and abuse, sometimes leading to severe health problems or death.
In the first year of life, it’s estimated that shaken baby syndrome affects approximately 35 out of every 100,000 infants. The effects of this kind of abuse are severe – around 65% of babies will have significant neurological disabilities, and between 5% and 35% may not survive their injuries. Most survivors are left with cognitive and neurological impairments.
Shaken baby syndrome is part of a much larger issue. Every year, millions of families are investigated by Child Protective Services for suspected child abuse or neglect. An average of over 3 million children per year are reported for potential maltreatment, and around 20% of these cases are confirmed.
- Experts estimate that between 1,000 to 1,500 infants per year are victims of pediatric abusive head trauma.
- According to the Centers for Disease Control and Prevention (CDC), about 10% of the 2,000 children who die from abuse each year are victims of shaken baby syndrome.
- Victims are usually between 3 and 8 months old, but it can occur in newborns and children up to 4 years of age.
- Up to 25% of all children diagnosed with shaken baby syndrome sadly lose their lives as a result of their injuries.
States with the highest rates of child abuse include New York, California, Texas, Michigan, Florida, Illinois, Massachusetts, Indiana, Ohio, and Kentucky.
Signs and Symptoms of Pediatric Abusive Head Trauma (Head Injury in Abused Children)
Abusive head trauma in children and infants is often difficult to diagnose as it goes unnoticed or misdiagnosed due to misleading background information and lack of consistent signs of injury. Often, symptoms vary from mild ones, mistaken for flu or cold, to life-threatening situations. Regrettably, a delay in diagnosis often results in more severe complications and potential repeated injuries, with a correct diagnosis typically made on an average of three health care visits.
The earliest signs of abusive head trauma can include:
- Decreased social interaction
- Difficulty in feeding
- Vomiting
- Feeling tired or low energy
- Extremely low body temperature
- Excessive sleep
- Failure to grow or gain weight appropriately.
More severe cases might present life-threatening symptoms such as difficulty in breathing, slow pulse rate, bulging of the soft spot on the newborn’s head, less awareness, and even seizures. In some cases, the child’s caregivers might delay acquiring medical assistance out of fear of potential legal consequences.
Despite this, it is important for doctors to consider the possibility of abusive trauma, even when there is no visible outside injury. A thorough physical examination can sometimes reveal subtle signs of abuse.
Physical signs of abusive head trauma can include:
- Bruising in infants less than four months old
- Bruising on the ears, neck, or torso in children less than four years old
- Bulging soft spot on a newborn’s head
- Shrinkage of the brain size
- Injuries to the frenulum
- Build-up of fluid in the brain
- Restriction marks around the neck
- Bleeding in the retina
- Fractures in long bones and ribs
- Bleeding around the brain
One should undergo a universal neurologic screening for detecting any hidden injury inside the skull, since many kids with abusive head trauma does not show symptoms. The biggest neurological sign is a change in state of consciousness, delays in development, seizures, and nausea with vomiting.
More specifically, retinal bleeds are usually more severe in abusive head trauma cases compared to accidental ones. However, it should not be the sole basis for diagnosis as it might also result from other causes such as anemia, birth trauma, or leukemia. In contrast, absence of retinal bleeding doesn’t necessarily rule out abuse.
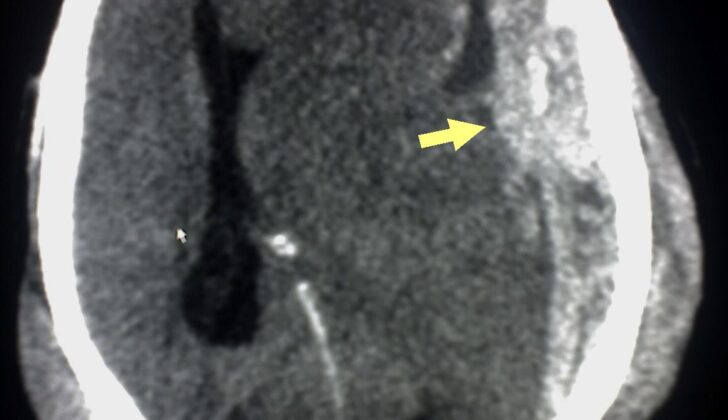
A common finding in abusive head trauma is a subdural hematoma, or a bleed in the brain space, caused by sudden or violent movement of the brain within the skull. Separately, rib fractures are common signs of abuse in infants and often result from the chest being squeezed.
Skull fractures can result from direct force applied to the head and suggest abusive head trauma when they are complex or multiple. Other indicative fractures involve long bones, posterior rib, or metaphyseal “corner” fractures which are common in abusive head trauma than accidents. Metaphyseal fractures have a unique “bucket-handle” appearance due to the disruptive force on the bone ends caused by shaking, twisting or pulling on the limbs. Clinicians should also consider abusive head trauma in case of unexplained neck injuries, seizures or fractures even when there’s no retinal or subdural hemorrhage or brain injury.
Testing for Pediatric Abusive Head Trauma (Head Injury in Abused Children)
When there is suspicion of abusive head trauma, a thorough and detailed investigation is needed. This involves multiple steps such as a full medical history, physical check-up, lab tests, imaging scans, and getting advice from specialists.
It’s especially important to find out the timeline of symptoms – when they appeared and how they advanced. Doctors should use non-leading questions to avoid influencing the answers and potentially find a different reason for the injuries. A story that doesn’t mention an accident or a short fall is often seen in abusive head trauma cases. Children who have suffered accidental injuries usually have caregivers who talk about a trauma event. Red flags to be alert for include a changing or inconsistent story from caregivers.
Examining the child carefully from head to toe is an important part of the assessment, with special emphasis on the neurologic examination.
Several tests should be carried out for further evaluation:
– Complete blood count including a check on platelet levels
– Chemical makeup of the blood
– Testing liver and pancreatic functioning
– Urinalysis
– CT/MRI/MRA scans, and a full skeletal survey
Imaging like CT and MRI scans can often confirm if abusive head trauma has occurred. Initially, a skeletal survey and a head CT scan should be done.
CT Scan
The head CT scan plays a crucial role in diagnosing internal head injuries that have resulted from abusive head trauma. Though very helpful, a CT scan might not always detect swelling, fractures, or tissue damage. Therefore, in most cases, it is followed up with an MRI.
MRI
An MRI can provide more detail by distinguishing between a long-standing subdural (beneath the dura mater of the brain) and subarachnoid (between the brain and skull) collections. It can also determine the extent of brain injury. Diffusion MRI scans can provide even more information for a correct diagnosis.
Skeletal Survey
For children under two with unexplained traumatic injuries, a skeletal survey is necessary. It consists of X-rays of the spine, head, ribs, and long bones. These are usually successful in detecting abuse. A single image or ‘babygram’ should be avoided as it gives only limited detail. If a fracture is suspected but doesn’t initially show up, follow-up rib films can be considered after 2-3 weeks.
Bone Scans
If skeletal surveys do not display any fractures but there’s high suspicion of some, bone scans can be used as an alternative. These scans are costlier, harder to execute, and expose the child to more radiation.
Laboratory Tests
Lab tests should include a complete blood cell count with platelet count, a chemistry panel, prothrombin time, partial thromboplastin time, amylase, lipase, aspartate aminotransferase, alanine aminotransferase, and a urine test. These tests can either provide further evidence of abusive head trauma by revealing additional injuries indicative of child abuse, or they can identify an underlying medical condition that might be misunderstood as child abuse or abusive head trauma.
Treatment Options for Pediatric Abusive Head Trauma (Head Injury in Abused Children)
When dealing with abusive head trauma, most often, doctors focus on supportive care for the patient. This involves closely watching vital signs like heart rate and blood pressure. If a patient has trouble breathing, they may need a machine to help them breathe (known as intubation and mechanical ventilation). There may be increased pressure inside the skull, and this needs to be observed and managed. If the patient has a type of blood clot called a subdural hematoma, doctors might consider surgery to remove it. The goal of all treatments is to maintain a balance between keeping the pressure inside the skull low while ensuring good blood pressure to make sure enough blood reaches the brain.
Doctors often go through a few stages of treatment:
First, they make sure the patient’s airway is clear, they’re able to breathe, and their circulation is good. If the child is awake, aware, and has normal blood pressure, treatments might only involve supportive care. If the blood pressure is too low, doctors will administer fluids. If the child’s condition is more critical, for example, if they’re unconscious or having a lot of trouble breathing, doctors may need to take more advanced steps to improve breathing and prevent choking. The neck might need to be immobilized during these procedures to prevent further injury.
Secondary injury to the brain can also occur after the initial trauma. This may include a range of issues such as blood clotting problems, low oxygen levels, low or high blood pressure, increased pressure inside the skull, high levels of carbon dioxide (hypercarbia), altered blood sugar levels, changes in electrolyte balance, growth of hematomas (blood clots), seizures, and fever. These conditions can worsen the existing brain injury. Doctors aim to minimize these complications to prevent further damage to the brain.
Monitoring oxygen levels in the blood and making sure there is enough oxygen reaching the brain is essential. Doctors might use pulse oximetry, a device that measures the amount of oxygen in the blood. To prevent hyperventilation that could lead to vasoconstriction (narrowing of the blood vessels) and decreased blood flow to the brain, doctors might use a method called capnography to measure the levels of carbon dioxide being exhaled. Important to note, managing the pressure inside the brain is crucial to prevent further injury.
In the next stage of treatment, if the injury has resulted in high pressure inside the skull, medications like barbiturates might be given. These medications help lower the pressure by reducing the brain’s metabolic demand and blood flow.
For severe cases where the above treatments aren’t effective, a type of surgery called decompressive craniectomy might be performed. This surgery involves removing a part of the skull to allow the brain to swell without causing additional injury.
What else can Pediatric Abusive Head Trauma (Head Injury in Abused Children) be?
When considering child head injuries, it is important to rule out alternative causes to abusive head trauma. These include accidental injury, birth-related injuries, blood clotting, inherited conditions, tumors, hormonal disorders, meningitis, diseases affecting the body’s tissues and disorders causing increased fluid in the brain. Other conditions, that share common symptoms, should also be excluded like the fragile bone disease, certain metabolic disorders, vitamin K deficiency, and rebleeding from a previous head injury.
- Accidental head trauma
- Sudden brain bleeding
- Abnormal connections between arteries and veins
- Blood disorders
- Bleeding in the lower part of the brain
- Disorders involving connective tissue
- Bleeding between the brain and the skull
- Pus-filled infection between the brain and the skull
- Intracranial bleeding
- Metabolic disorders such as glutaric aciduria type 1 causing bleeding at the back of the eye
- Stroke
- An infected mass between the brain and the skull
Head injuries in kids can result from falls, yet most falls don’t cause serious trauma. However, any child with severe injuries from a fall must undergo further medical evaluation to exclude abusive head trauma. Traditionally, injuries from falls off a bed are minor with the exception of falls from bunk beds. Serious injuries can happen but are rare and depend on factors like the type of flooring and the distance of the fall.
Stair falls can pose a significant injury risk, particularly if a child is in a moving device like a walker or stroller and about 1 to 8% result in brain bleeds. If a child slips from a caregiver’s arms while walking up or down the stairs, the resulting injuries are usually less severe, often limited to specific areas and rarely multiple.
Falls from 1 to 4 feet rarely cause serious head trauma or multiple injuries, yet some studies report deaths among children from falls this height, often suggesting further evidence of abuse. In studies of falls from 5 to 6 feet, similar findings have been reported. Falls from great heights (10 feet or more) rarely result in death unless the fall is from an extremely high place, but the risk of fractures and injuries increases with the height of the fall. In a large study, out of 75,000 cases, 18 children suffered fatal injuries as a result of a fall, with some falling from a swing and others from a flat surface like a ledge or ladder.
What to expect with Pediatric Abusive Head Trauma (Head Injury in Abused Children)
Abusive head trauma is associated with significant health problems and even death. These health problems can range from mild learning difficulties to severe mental or physical disabilities and death. The effects of this trauma can include blindness, attention deficit, delayed development, intellectual deficits, loss of sensation or hearing, motor dysfunction, lack of growth, feeding difficulties, seizures, and difficulties with behavior and education.
Abusive head trauma can also lead to paralysis of one side of the body (hemiplegia), paralysis of all four limbs (quadriplegia), water accumulation in the brain (hydrocephaly), and a smaller brain size (microcephaly). The likelihood of a patient with abusive head trauma recovering is linked to the severity of the injury seen on CT and MRI scans.
Survivors of severe abusive head trauma often experience a significant reduction in their quality of life. Even those with mild injuries may experience substantial lifelong impairment.
Research has compared the brain development outcomes after abusive head trauma and accidental head injuries. The findings show that infants younger than 36 months old who suffer abusive head trauma are likely to experience more severe injuries resulting in heart and breathing issues, deeper brain injuries, widespread brain oxygen deprivation, and worse outcomes compared to those with an accidental head injury. Unfortunately, children diagnosed with abusive head trauma are more likely to die compared to children with accidental head trauma.
Shocking statistics show that more than half of children between 0 to 4 years old who are injured by abusive head trauma will die before they reach 21 years of age. Harrowingly, children who are severely injured from abusive head trauma will experience a 55% reduction in their health and quality of life.
Abusive head trauma often leads to a number of long-term health issues. Over half of the children will experience full or partial blindness. Around 5% will need eye surgery, and over 20% will need a feeding tube due to the severity of their injuries.
Possible Complications When Diagnosed with Pediatric Abusive Head Trauma (Head Injury in Abused Children)
Possible complications of the condition can be diverse and might affect various parts of the body. These could include:
- Acquired microcephalus
- Cortical blindness
- Difficulty developing at a normal rate
- Loss of hearing
- Hydrocephalus
- Learning disabilities
- Bleeding in the retina
- Thinning of the macular
- Atrophy of the pigment layer in the retina
- Seizures
- Spasticity
- Loss of sight
- Weakness
Patients who experience bleeding in both retinas are likely to have suffered a severe neurological injury. Large hemorrhages behind the retina, wide-spread changes in the back of the eye, or bleeding in the clear, gel-like substance that fills the back of the eye are signs of this neurological injury.
Recovery from Pediatric Abusive Head Trauma (Head Injury in Abused Children)
If the patient’s job or physical abilities are impacted, it might be a good idea to think about consulting with occupational and physical therapists. Also, if language or speech problems are apparent, seeking advice from a speech therapist could also be worth considering.
Preventing Pediatric Abusive Head Trauma (Head Injury in Abused Children)
Society has a great responsibility, both ethically and financially, to reduce cases of abusive head trauma in children as it causes irreversible damage. The cost borne by society due to abusive head trauma is huge. In fact, it costs over $70 million in medical expenses every year in the United States.
Children who are victims of such trauma often need long-term support like education, physical therapy, speech therapy, and occupational therapy. Some may even need care in a nursing home for their entire lives. The people who cause this trauma often feel deep regret and their lives are also severely affected due to costly jail sentences.
Preventing abusive head trauma in children mostly involves reducing child abuse and neglect, and increasing education. This educational effort includes public announcements, pamphlets, brochures, and also extends to family resource centers and home visit programs, especially in homes at a higher risk such as those of young parents living in poverty.
These programs also offer mental and social services. Before hospitals discharge new parents, they need to be made aware of the risks associated with shaking a baby. Pediatricians and emergency department staff need to be trained to recognize parents who may be at risk of abusing their infant. Parents also need to be given some strategies to handle the frustrations of coping with a crying baby and understand the risks associated with shaking an infant with a developing brain.
To address the challenge of preventing abusive head trauma in children, there are two national health programs. One is the Period of PURPLE Crying program. This program provides education about normal infant behaviors like crying that can lead to frustration in caregivers. Here, ‘PURPLE’ refers to Peak (when crying is most intense around 2 months, then lessens), Unpredictable, Resistant (to soothing), Pain-like (appearance on face), Long (periods of crying), and Evening (most common time for crying).
The National Center on Shaken Baby Syndrome aims to increase confidence and skills in new and prospective parents. Professionals in the healthcare sector, through proper education about the dangers of shaking a baby, can contribute significantly to reducing the incidence of abusive head trauma. During every meeting with families, the focus should be on prevention. Educational resources are available through several organizations, including the American Academy of Pediatrics, the National Center on Shaken Baby Syndrome, and Prevent Child Abuse America.
Prevention is crucial and all healthcare providers need to work together to educate the public. Persistent crying is the main trigger for abusive head trauma. By identifying and educating those caregivers who are at a higher risk, the number of children experiencing abusive head trauma can be reduced.