What is Glottic Stenosis?
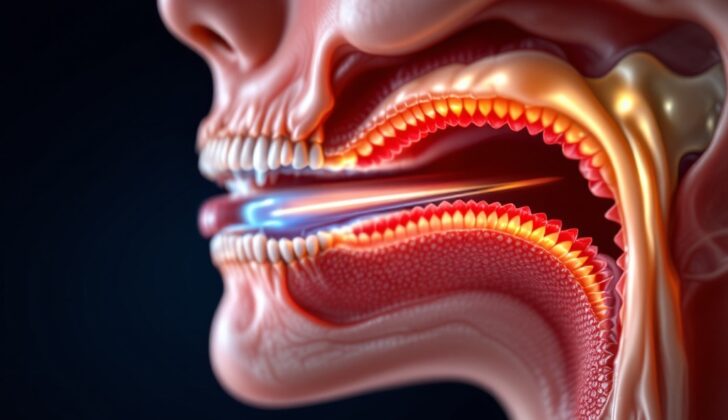
Glottic stenosis is a condition where the upper part of your airway, located at the glottis, becomes narrower than usual. The glottis is a part of your larynx (or voice box) that contains the vocal cords and the opening for air passage. The glottis starts from where the true and false vocal cords meet, extends downwards to a point about one centimeter below the lower part of the vocal cords. It has two sections: the front two-thirds, which is the vocal glottis (used for speech), and the back one-third, known as the respiratory glottis (used for breathing).
Glottic stenosis is one type of laryngeal stenosis, which refers to any narrowing in your larynx. This narrowing can occur in the glottis, above the glottis (supraglottic), or below the glottis (subglottic). It can be something you are born with, or it might develop later in life (acquired).
Treating this condition can be complicated, as doctors need to make sure they can maintain the patient’s ability to breathe, speak, and swallow without difficulty.
What Causes Glottic Stenosis?
Glottic stenosis is a condition where there’s a narrowing in the part of your throat called the glottis. This can happen from birth, also called “congenital,” although it’s quite rare. When it does occur, it’s usually because the fetus’ throat didn’t fully open up during the third month of being in the womb. The throat’s formation in the fetus often involves reopening it, with complete failure leading to a completely closed up throat, or laryngeal atresia. This condition can vary in severity, presenting as a thin membrane obstructing the throat, a thick web of tissue either in the front or back, or even completely fused vocal cords.
It’s a lot more common to develop this condition, also called “acquired,” and there are various reasons why this might happen. The main one is injury caused by having a breathing tube (endotracheal tube), possibly due to the pressure from the tube restricting blood flow which leads to inflammation and scarring. The chances of developing this condition from a breathing tube increases depending on how long the tube is in for, its size, the number of times the tube is inserted, and any excessive movement from the tube, especially if the patient is agitated.
There are other ways to injure the throat that could cause this condition, like accidentally swallowing something harmful, chemical burn from ingesting caustic substances, radiation, and injuries from outside the body. The tube that we place through your nose and go down your throat for feeding or to drain your stomach (nasogastric tube), if left in for long, could also cause ulcers leading to this condition. Aggressive surgeries in the throat could also lead to this condition.
Certain infections like syphilis, fungal infections, and diphtheria can cause this condition. Diseases characterized by inflammation and the formation of lump-like lesions, such as tuberculosis, sarcoidosis, and granulomatosis with polyangiitis (disease causing inflammation and damage to blood vessels) are other potential causes. Some rare causes could be fungal infections in patients with weakened immune systems, leprosy, a blistering condition called mucous membrane pemphigoid, and scarlet fever.
There’s some thought that stomach acid flowing back into the throat (gastroesophageal reflux) might have a role in making this condition worse, but it’s not quite clear yet how much of a factor it really is.
Risk Factors and Frequency for Glottic Stenosis
Glottic stenosis, a narrowing of the part of the throat containing the vocal cords, can occur due to several reasons. The most common type is post endotracheal intubation stenosis, which happens after a tube is inserted into the trachea to assist in breathing. Two research studies have found that 6 to 19% of patients who underwent intubation, especially those intubated for five days or longer, develop this condition. Congenital glottic stenosis, which is present at birth, is extremely rare, with one extensive study identifying 51 cases in children over a 32-year period.
- The most common type of glottic stenosis is post endotracheal intubation stenosis.
- Between 6 and 19% of intubated patients may develop this stenosis.
- The risk is particularly high in those intubated for five days or longer.
- Congenital glottic stenosis is very rare.
- Over a period of 32 years, only 51 cases were identified in children in one large study.
Signs and Symptoms of Glottic Stenosis
Glottic stenosis, a narrowing of the windpipe caused by swelling or abnormalities, can have various symptoms based on its cause and severity. The most common symptom is stridor, an abnormal breathing sound that varies depending on whether the obstruction is in the upper or lower respiratory tract.
For babies born with this condition, signs may include having breathing difficulties right from birth. This can be coupled with a weak or unusually soft cry, and in some cases, no voice at all (aphonia). Severe cases may require immediate medical interventions such as intubation or a tracheostomy. Some children with mild glottic stenosis might not show any symptoms until they have a respiratory infection. Swelling of the airway and thick mucus can cause difficulty in breathing. It’s also important to monitor kids who frequently have croup (a viral infection causing a barking cough), as they may have glottic stenosis.
For individuals who develop glottic stenosis later in life, the symptoms will depend on where and how severe the narrowing is. People with a restriction towards the back of the windpipe mainly present with breathing difficulties. Those with anterior (front side) glottic webs mainly have voice alterations. Common symptoms include:
- Difficulty breathing
- Episodes of no breathing (apnea)
- Rapid breathing (tachypnea)
- Hoarseness
- Change in voice or no voice (aphonia)
- Difficulty swallowing (dysphagia) and inhalation of food or liquid into the lungs (aspiration)
In addition, it’s important to understand when and how severely the symptoms started, what improves or worsens them, and the overall health and voice quality of the patient. Information about past occurrences of intubation or trauma, as well as any infections, inflammation, or other health conditions could also be helpful in diagnosis and treatment.
Testing for Glottic Stenosis
If your doctor suspects that you may have glottic stenosis, which is a narrowing of the voice box opening, they will typically use a flexible fibreoptic endoscopy as a first step in diagnosing it. This procedure involves using a thin tube with a tiny camera on the end to look into your throat and voice box. This test can be done while you’re awake, regardless of your age.
If the first test suggests you might have glottic stenosis, your doctor will likely recommend microlaryngoscopy. This is a more in-depth examination of your voice box performed under general anesthesia. This allows doctors to evaluate the movement of structures inside your throat. A biopsy, or a small sample of tissue from the narrowed area, may also be taken to analyze in a laboratory to help understand what’s causing the condition and could also be part of the treatment.
Besides these procedures, your doctor might use imaging studies and other tests to see the extent of the narrowing and assess your swallowing function. Although not often used, a lateral soft tissue neck plain x-ray can sometimes be helpful, especially if a foreign body is suspected to be causing the problem. Videofluoroscopy, another imaging tool, can help check how swallowing might be affected.
A CT scan, a type of x-ray that takes detailed images from different angles, is also valuable. It can show your doctor the severity of the stenosis and help them assess if any other lung problems coexist. 3D segmentation, a process that breaks down a CT scan into smaller, more detailed images, can also be useful for surgical planning.
Other investigations your doctor may recommend include a voice analysis to understand how the condition is affecting your speech, and pulmonary function tests to examine your lung function. The doctor might also suggest electromyography (EMG), a test that measures muscle response to nerve stimulation, which can help differentiate glottic stenosis from a condition called bilateral vocal cord paralysis. Finally, if your doctor suspects that an inflammatory disease may be causing your condition, they might order some blood tests to measure the level of inflammation in your body.
Treatment Options for Glottic Stenosis
Glottic stenosis, a condition where part of your larynx (voice box) narrows or closes, requires specialized treatment tailored to each individual. The main goal of managing this condition is to secure your airway so you can breathe easily. However, it’s also important to try and preserve the function of your larynx and, by association, your voice.
When glottic stenosis is present from birth, doctors often carefully monitor the situation or may use a non-invasive procedure (an endoscopic approach) to separate the area causing the problem. For severe cases, doctors may need to place a stent (tube) in the larynx or perform a tracheostomy (permanent hole in the neck to breathe through). If this condition is detected before birth (known as congenital high airway obstruction syndrome), doctors have to carefully manage the baby’s air supply until a permanent solution, like intubation (tube in the throat) or tracheostomy, can be put in place.
Glottic stenosis can also develop from infections or inflammation. Here, the focus is on treating the initial problem medically; doing so can often improve the stenosis and eliminate the need for surgery.
Acquired glottic stenosis, which is developed after birth, can be treated with one of two main surgical methods. Thin web-like structures causing the problem can often be managed with small dilatations or incisions made with a laser or a blade. For thicker web-like structures, which risk returning after treatment, doctors may need to use more complex methods including removing the scar tissue, recovering the area with mucus, and placing a stent. For posterior glottic stenosis, where the back part of the larynx narrows, some techniques have shown promising results.
Several different treatments are used to enhance the effectiveness of glottic stenosis surgery. One method includes injecting botulinum toxin to temporarily weaken muscles that cause narrowing in the larynx, helping promote better healing and reducing the risk of re-narrowing. Another treatment, mitomycin C, helps reduce the risk of re-narrowing and scarring by inhibiting the cells that produce scar tissue. Steroids can also be injected into the back of the larynx to help reduce inflammation and the formation of excess tissue. However, the use of systemic steroids, which affect the entire body, can be complex as they can reduce scar tissue formation but also decrease wound healing.
Open surgical techniques may be necessary when the other procedures don’t work or if the larynx webbing is too thick. This typically involves creating a fissure (narrow opening) in the larynx and surgically removing the web. A stent is often used to keep the larynx open while the body heals. Various types of grafts can be used to cover the healing area such as skin grafts, mucosal grafts, and rib cartilage grafts.
What else can Glottic Stenosis be?
Glottic stenosis, a condition that affects the voice box, can be hard to distinguish from a similar condition called bilateral vocal cord palsy. Both of these conditions have similar symptoms and can be triggered by the same events. To determine which of these two conditions a patient is suffering from, doctors might use techniques like electromyography (a test that evaluates muscle and nerve function), a flexible nasendoscopy (a procedure that allows doctors to look at your nasal passages), or an examination under anesthesia.
But there are other conditions that also need to be ruled out when diagnosing glottic stenosis. These include:
- Supraglottic squamous cell carcinoma (a type of throat cancer)
- Tracheobronchial amyloidosis (a disease that causes protein deposits in certain organs)
- Relapsing polychondritis (a rare disorder that causes inflammation in various tissues)
- Idiopathic laryngeal, tracheal stenosis (unexplained narrowing of the windpipe)
- Respiratory papillomatosis (a rare condition where tumors grow in the air passages leading from the lungs to the nose and mouth)
What to expect with Glottic Stenosis
Airway blockage in the voice box, known as glottis, can be tricky to manage and treat effectively. Dealing with this condition requires a certain level of expertise, as blockages often reappear even after treatment, thus demanding repeated procedures.
The voice box being affected can lead to less successful results after reconstructive surgery compared to blockages in other parts of the airway. Similarly, a patient’s existing illnesses or medical conditions can also increase the risk of not attaining favorable results.
There is a difference in opinion regarding the best surgical approach to treat this condition. Some experts believe that all non-surgical and endoscope-assisted treatments should be tried first, with surgical approaches on standby if those fail. On the other hand, there are experts who believe that starting with open surgeries has better outcomes.
Take into account that results for voice quality can be highly variable after such treatments. However, the voice generally improves after the airway blockage is treated.
Possible Complications When Diagnosed with Glottic Stenosis
Normal complications after surgery, like bleeding, wound infection, puffiness caused by air under the skin, or nerve and blood vessel damage, are usually treated in a non-aggressive manner. However, some issues need immediate attention, such as blockage of the airway, accidentally inhaling a stent (a device used to keep open narrowed or blocked bodily passages), a large bruise (hematoma), or a collapsed lung (pneumothorax). A blocked airway is usually treated by inserting a tube into the trachea or by performing an emergency tracheostomy (a surgical opening in the neck for breathing), while inhaled stents require urgent removal using a bronchoscope (a tool used to view the airways). Large bruises and collapsed lungs are treated by draining the excess fluid or air. Also, mucus and secretions can block the airway and require instant suctioning.
In addition, there are other complications like the narrowing of passages coming back, chronic inhalation of food or fluids into the lungs, infection, expulsion of a keel (a device used to prevent closure of the larynx), inflammation of cartilage, changes in voice, excessive growth of roundish, healing tissue, and dependence on a tracheostomy.
- Bleeding
- Wound infection
- Puffiness from air under the skin
- Damage to nerve and blood vessels
- Airway blockage
- Accidental inhalation of a stent
- Large bruise (hematoma)
- Collapsed lung (pneumothorax)
- Blockage of airway by mucus and secretions
- Narrowing of passages reoccurring
- Chronic inhalation of food or fluids into the lungs
- Infection
- Expulsion of larynx-protecting device (keel)
- Inflammation of cartilage
- Changes in the voice
- Excessive growth of roundish, healing tissue (granulation tissue)
- Dependence on a tracheostomy
Preventing Glottic Stenosis
If a patient starts experiencing sudden symptoms like difficulty breathing or if these symptoms get worse, they should immediately go to the emergency room. This is especially important after surgery. It’s crucial for both the patient and the people caring for them to understand and manage their condition, which is airway narrowing or ‘stenosis.’
For parents of children born with glottic stenosis, a type of stenosis affecting the voice box, it’s necessary to learn pediatric basic life support and how to take care of a tracheostomy, a medical procedure where a hole is made in the neck to help breathing.
Patients need to know that glottic stenosis often comes back, and they might need multiple treatments. However, they should be reassured that with time and regular check-ups, they can manage their condition well and lead a good quality life.