What is Axenfeld-Rieger Syndrome?
In 1920, a notable German eye doctor named Theodor Axenfeld, noticed an important feature in the eye called the Schwalbe line, which was extra visible and pushed forward. He pointed out the strands of iris sticking to it. These findings were later titled ‘Axenfeld anomaly’. Later, an Austrian eye specialist, Herwigh Rieger, discovered a unique set of eye abnormalities called the ‘Rieger anomaly’. These included changes to the Schwalbe line, underdeveloped iris, multiple pupils, and displaced pupils.
There were also general body changes found alongside the Rieger anomaly such as issues with teeth, facial bones, belly button, an abnormal opening in the male urethra, and problems with the pituitary gland. These were classified as Rieger syndrome. Nowadays, the terms Axenfeld anomaly, Rieger anomaly, and Rieger syndrome are not used. Instead, these eye irregularities and their related body changes are together diagnosed as Axenfeld-Riger syndrome (ARS).
ARS is a disease composed of abnormal features in the front part of the eye, together with systemic abnormalities like dental, heart, face and belly wall defects. The genetic changes involved with ARS are present in several genes identified by their position in our chromosomes such as PITX2 (chromosome 4q25), FOXC1 (chromosome 6p25), PAX6 (chromosome 11p13), FOXO1A (chromosome 13q14), and CYP1B1 (chromosome 2p22.2).
What Causes Axenfeld-Rieger Syndrome?
ARS, also known as Axenfeld-Rieger syndrome, has been linked to alterations or mutations in several chromosomes, including chromosomes 2, 4, 6, 9, 13, 18, and 21.
ARS Type 1, on the other hand, is a type of disorder that is passed down through families. It’s caused by a change or mutation in a gene known as PITX2, which is located on chromosome 4. This gene is instrumental in the development of teeth and the color part of the eye, or iris.
ARS Type 2 is also inherited but has been associated with mutations on chromosome 13. This means that the disorder’s specific characteristics are known, but the exact genetic change causing the problem hasn’t been identified yet.
ARS Type 3 has been linked to changes in a gene called FOXC1, which is located on chromosome 6. If mutations occur in FOXC1, it can cause ARS type 3. This gene is also associated with a syndrome that has some of the same signs and symptoms as ARS type 3.
From all cases showing signs of ARS, about a quarter to a third are found to have mutations in both the FOXC1 and PITX2 genes, which are situated on chromosomes 6 and 4 respectively. Various types of these changes have been studied, resulting in a better understanding of the genes’ role in ARS.
About 10% to 30% of ARS patients have been found to have mutations in the PITX2 gene, as found through animal studies. A specific subset of ARS, referred to as De Hauwere Syndrome, is characterized by water accumulation in the brain, issues with eye muscles, wide-spaced eyes, loose joints, delayed motor skills, and hearing loss.
ARS shows what is known as genetic heterogeneity – this means different genes can cause the same characteristics or signs of the condition. It is typically inherited in what’s known as an autosomal dominant manner, but it can occasionally appear randomly in a family. The symptoms of ARS can vary widely in expressivity, despite the fact it often shows full penetrance, or likelihood of appearing when the gene mutation is present.
Risk Factors and Frequency for Axenfeld-Rieger Syndrome
ARS, or Axenfeld-Rieger syndrome, is quite rare. It’s estimated to occur in about 1 in 50,000 to 1 in 200,000 live births. It can affect anyone, regardless of race or gender. In most cases, the unique characteristics of ARS appear in both eyes.
Signs and Symptoms of Axenfeld-Rieger Syndrome
Axenfeld-Rieger syndrome, often referred to as ARS, is a condition that can result in a variety of irregularities, such as abnormalities related to the eyes, teeth, face, and abdomen. In the past, this syndrome was categorized into several different disorders, such as Axenfeld anomaly and Rieger anomaly. Generally, it is identified during infancy or childhood. Glaucoma associated with ARS often doesn’t show up until later in childhood or adulthood, but there are instances when it can appear very early in life, even within the first three years.
Congenital glaucoma may present with signs like a large, blue-tinged cornea, tearful eyes, and light sensitivity. Patients often complain about abnormal eye appearance, crossed eyes, or poor vision. Light sensitivity is especially common due to irregularities with the iris and pupil. Many cases of ARS are found during routine eye checkups, so it’s crucial for all patients to receive a comprehensive eye examination.
- Large, blue-tinged cornea
- Tearful eyes
- Light sensitivity
- Abnormal eye appearance
- Crossed eyes
- Poor vision
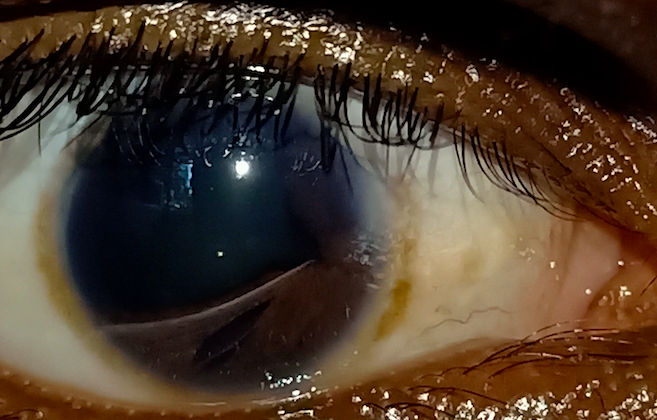
‘Axenfeld anomaly’, a term related to ARS, includes a pronounced and forward-shifted Schwalbe line, which can be seen in a slit-lamp examination. Other conditions, like Alagille syndrome, can also demonstrate a posterior embryotoxon. Moreover, it’s possible for healthy individuals to display a posterior embryotoxon – this is found incidentally in around 8% to 15% of normal individuals, typically without related ocular or systemic abnormalities, such as glaucoma.
ARS can also be associated with irregularities of the iris, such as weak stromal, full-thickness iris defects that can create the look of multiple pupils, a misplaced pupil, and ectropion uveae. Generally, the cornea appears clear, unlike in the iridocorneal endothelial (ICE) syndrome. Before, these findings, along with posterior embryotoxon, were categorized as Rieger anomaly. They can seem clinically very similar to ICE syndrome, which typically occurs in older individuals and affects only one eye. The iris can sometimes appear normal, but there can also be other ocular findings.
Rieger anomaly can also come with various non-eye related conditions, previously referred to as Rieger syndrome. Among the common findings are abnormalities in tooth development, such as missing one or more teeth, having smaller than normal teeth, and facial features like mild craniofacial irregularities, wide-set eyes, sunken upper jaw, and a broad flat nasal bridge. Other systemic associations can include hypospadias, redundant skin around the belly button, umbilical hernia, an excess of brain fluid, hearing loss, anal stenosis, kidney anomalies, cardiac abnormalities, arachnoid cyst, pituitary abnormality, endocrinological irregularities like short stature and slow growth, and a dislocated hip from birth.
Testing for Axenfeld-Rieger Syndrome
Gonioscopy is a critical step in examining people who might have Axenfeld-Rieger syndrome (ARS), as it allows doctors to look closely at the angle where the iris meets the cornea in your eye. In people with ARS, doctors often observe specific features during gonioscopy, such as a prominent Schwalbe line (boundary between the clear cornea and white sclera), strands of iris tissue attached to this line, the front insertion of the iris, and the existence of iris tissue processes (bumps). With ARS, these visible iris strands can vary, being thin or wide.
Besides gonioscopy, other tests for ARS may be advised. These could involve taking pictures of the front of the eye, the optic nerve (that connects to your brain), or even a mapping the thickness of your cornea. High-definition eye scans of the optic nerve and a part of your retina, as well as visual field tests, can also be done.
People suspected to have 6p25 microdeletion syndrome should receive a thorough check-up, that includes a visit to an eye doctor- especially if they have a certain eye condition known as posterior embryotoxon. Additional checks could comprise evaluations of brain development, heart scans, brain imaging, vision and hearing tests, and specific brain response tests.
Children with ARS often have an increased risk of glaucoma, a condition that can lead to vision loss. Therefore, getting these children checked and treated promptly is of utmost importance. For babies with glaucoma, full checks under anesthesia may frequently be needed- these might assess the corneal size, eye pressure, the state of the optic nerve, and the eye’s axial length. While basic health care providers may spot symptoms and diagnose in the first instance, these children will need further assessments by eye specialists. There might be a need for surgeries or focused care to prevent permanent visual impairments or blindness.
Treatment Options for Axenfeld-Rieger Syndrome
The way we treat Axenfeld-Rieger syndrome is unique to each person because symptoms can vary greatly. About half of patients with this condition will develop a certain type of eye disease called glaucoma, which may eventually need surgery. These surgeries, known as trabeculectomy and trabeculotomy, can effectively control the eye pressure according to studies in children.
Medications for glaucoma often don’t work well for patients with Axenfeld-Rieger syndrome. In a study of 46 individuals, nearly 70% needed surgery to manage their glaucoma. The medications that could be used include beta-blockers, inhibitors, and prostaglandin analogs. However, medicines containing alpha agonists, like brimonidine, can lead to sleep apnea and depress the central nervous system in kids. They should be avoided in children under 2 years.
Two types of surgery, goniotomy and trabeculotomy, may not always work in the long run if there are abnormal developments in the eye. In such situations, other surgical options are more effective. These include trabeculectomy with anti-fibrotics, combined trabeculotomy and trabeculectomy, and the placement of glaucoma drainage devices. However, a lot of these patients need more than one surgery. Also, it can be quite hard to control the eye pressure over time, even with medications and surgeries.
Sometimes, there may be a need for special procedures, including cyclocryotherapy and diode laser cyclophotocoagulation. Like any surgery, these procedures have risks such as low eye pressure, a type of bleeding in the eye called suprachoroidal hemorrhage, and eye infection known as endophthalmitis. It’s important to carefully weigh the risks and benefits before planning any procedure like these.
What else can Axenfeld-Rieger Syndrome be?
Iridocorneal Endothelial Syndrome
Iridocorneal Endothelial Syndrome is a condition that usually affects middle-aged women. It often impacts just one eye and causes changes in the corneal endothelium, the clear tissue covering the front of the eye. There are three types of the syndrome:
- Chandler Syndrome – The endothelium takes on an unusual appearance similar to the front of the eye. It can cause the cornea to have a beaten bronze look and swell.
- Essential iris atrophy – This leads to progressive damage to the iris, which can result in holes in the iris, multiple pupils, and distortion of the pupil.
- Cogan-Reese (iris nevus) – The iris develops small bumps on its front surface.
Iridoschisis
Iridoschisis involves the splitting of iris layers. Generally, it impacts the lower iris but does not damage the pigmented iris tissue on the back of the iris. It’s often associated with a shallow front part of the eye and a type of eye pressure condition known as angle closure glaucoma.
Peters Anomaly
Peters Anomaly is a birth defect that causes a cloudy cornea, which may or may not be stuck to the iris or associated with a cataract.
Aniridia (iris hypoplasia)
In Aniridia, the iris appears to be absent during an eye exam, but a small part of the iris may be visible upon further inspection. It’s associated with other conditions, including corneal scarring, high eye pressure, underdeveloped fovea (the center part of the retina), and an underdeveloped optic nerve.
Oculodentodigital Dysplasia
This is a genetic condition resulting from mutations in a specific gene. It causes a range of symptoms, including smaller-than-normal eyes and cornea, high eye pressure, cataracts, a narrow nose, tooth enamel problems, and joined or webbed fingers.
Congenital Ectropion Uveae
This condition causes a smooth, bump-less front surface of the iris, visible pigmented back of the iris, high iris insertion, and associated eye pressure disorders.
Ectopia Lentis Et Pupillae
This is a genetic eye condition that affects both eyes and causes displacement of the pupil and the lens. It may also cause nearsightedness, detachment of the retina, and cataracts.
What to expect with Axenfeld-Rieger Syndrome
The outlook for patients with Axenfeld-Rieger syndrome (ARS) depends on their individual circumstances, as the condition can vary significantly in how it presents and affects other aspects of health. Some patients may only have abnormalities in the front part of their eyes, while others may also have heart defects of varying degrees. The complexity of these issues can affect their overall wellbeing.
For those affected only by eye issues, the outlook is generally good if they don’t develop glaucoma. However, treating glaucoma can be difficult, and it may not respond to medication alone. Patients with ARS who require surgery for glaucoma usually need more than one surgical procedure, with on average around 2.2 surgeries performed on each eye.
If glaucoma diagnosis and management are delayed, it can lead to blindness, eye shrinkage, or a condition known as a painful blind eye.
Possible Complications When Diagnosed with Axenfeld-Rieger Syndrome
Axenfeld-Rieger syndrome, or ARS, can lead to a number of complications. Among these are different types of ocular or eye-related problems, including a condition known as posterior embryotoxon. Around half of all people who have ARS will develop a disease called glaucoma, a condition which often surfaces after middle childhood but can also appear earlier in some cases.
One common symptom across all ARS cases is a high placement of the colored part of the eye, or iris. This is particularly noticeable in people with ARS who also have glaucoma. On the other hand, other abnormalities like strands of iris tissue around the eye’s periphery, iris changes, and posterior embryotoxon may not necessarily correlate with whether or not a person has glaucoma, or how severe it might be.
Experts believe that glaucoma in ARS patients may be due to problems with the angle of the eye or issues with the development of certain parts of the eye, like the trabecular meshwork and Schlemm canal. It’s thought that disruptions in the development of certain cells could lead to the survival of immature cells over the iris and angle of the eye. This could block the flow of fluid from the eye, which in turn causes glaucoma.
Born with a glaucoma (Congenital Glaucoma or CG) in patients is often connected to mutations in the FOXC1 and PITX2 genes. This can lead to serious issues, like blindness or diminished vision in children. Another common effect of childhood glaucoma is a condition known as amblyopia.
Patients with FOXC1 gene mutations might also experience hearing loss, eye problems, and heart-related complications. One particular study involving a family with several cases of ARS and heart disease found FOXC1 mutations, suggesting that this gene could be involved in the development of the cardiac system.
Common complications associated with ARS:
- Various eye-related problems, including posterior embryotoxon
- High placement of the iris
- Glaucoma
- Congenital Glaucoma (CG), often due to mutations in the FOXC1 and PITX2 genes
- Blindness or diminished vision in children
- Amblyopia
- Hearing loss, eye problems, and heart-related complications in patients with FOXC1 gene mutations
Preventing Axenfeld-Rieger Syndrome
It can be helpful for patients and their families to be aware of the different types and risks of complications associated with ARS, a medical condition that can lead to an increased risk of developing glaucoma. Aside from eye-related abnormalities, ARS can also result in abnormalities in the teeth and cause underdeveloped upper jawbones. Patients experiencing these symptoms may find it beneficial to consult with specialists who deal with facial defects, such as maxillofacial surgeons. Furthermore, patients have the option to undergo genetic counseling and potentially genetic testing, as some types of ARS can be passed down through families.