What is Blunt Eye Trauma (Eye Injury)?
Blunt eye trauma can cause various injuries within the eye itself. These can be ‘open’ or ‘closed’ injuries. Closed injuries have two types, namely, contusion and lamellar lacerations. Open injuries can result in a tear (laceration) or a full break (globe rupture) in the eye. An open wound may happen because something pierces the eye, goes through it, or an object gets lodged in the eye (IOFB). Eye injuries can result from a direct hit, an indirect hit, or the eye being squashed from front-to-back or side-to-side.
The cause of the injury could be a hard hit on the eye or unintentional blunt trauma. Eye injuries are classified as closed, ruptured, or injuries outside the eye. Any part of the eye can be affected; specific identification is usually based on a medical examination rather than laboratory tests, though these may be required for serious cases or those likely to need surgery.
Imaging tests like X-rays, CT scans, or MRIs are typically done after surgery. If there’s suspicion of a foreign object being lodged in the eye, imaging may be done before surgery to check the depth and location of the IOFB. The treatment depends on the type and severity of the injury and if surgery is needed. The final impact on vision is based on the nature of trauma, time taken for treatment, extent of eye damage, timing of surgery if required, and post-surgery care.
What Causes Blunt Eye Trauma (Eye Injury)?
Blunt trauma to the eye can result in both open and closed injuries. Closed injuries can be generally categorized as bruises or partial tears, while open injuries are broken down into tears and ruptures. There can be a tear if the eye is injured by something penetrating it, like an object stuck in the eye. A rupture might occur if blunt force causes pressure inside the eye to increase, breaking the outer layer of the eye. How the eye is injured can range from direct hits to the eye to accidental blunt trauma.
Young children frequently experience closed injuries while playing at home or with peers. The most common injuries for them involve sports trauma, being hit by a wooden stick, or getting burned by firecrackers. Closed injuries in adults are more commonly associated with scenarios like assault, work-related trauma, traffic accidents, falling, or intentional harm. These injuries can also occur due to high-risk job situations, particularly in fields like manufacturing, plumbing, mining, and agriculture. Furthermore, these can happen due to sports or domestic violence.
It’s significant to note that an eye rupture can occur when the front part of the eye known as the cornea or the white part of the eye known as the sclera, or both, have a defect. This usually happens when something directly penetrates the eye, but enough blunt force can also cause the pressure inside the eye to rupture it. Common causes of eye injury in children are sharp toys, household pets, scissors, and eyeglasses, with scissors being the most prevalent. For adults, workplace injury, chemical exposure, stick injury, or injury from items like iron rods, nails, and cement are leading causes. For elderly people, it is quite common that they get injured from falling from the bed, bathroom, or vehicles, or falling on ground.
Retrobulbar hematoma, which is a collection of blood at the back of the eye, is often related to trauma to the eye or associated fractures of the eye socket. It may also inadvertently happen during sinus or eye surgery. In rare cases, it can occur in people who are taking blood thinning medications and experience a sudden increase in pressure, like from throwing up, straining, or coughing.
Risk Factors and Frequency for Blunt Eye Trauma (Eye Injury)
Eye injuries, also known as globe injuries, occur at a rate of 3.5 per 100,000 people, with men accounting for about 80% of these cases. Children are often injured by sharp objects like pens, scissors, or knives that directly penetrate the eye. Eye injuries can also result from blunt force trauma, like car accidents, physical fights, or work-related incidents that involve activities like hammering. For older people, falls are the most common cause of eye injuries. Even though eye injuries leading to retrobulbar hematoma (bleeding behind the eye) are rare, occurring in less than 1% of cases, they’re frequently associated with progression to blindness.
Men, especially those aged 30 to 40, are most likely to suffer from open globe injuries. It’s also common to find an intraocular foreign body, or an object inside the eye, present in 40% of these cases. This is often seen in situations involving activities that could easily lead to eye penetration such as hammering, grinding, or drilling.
- A study in North India showed that 82.3% of non-work related eye injuries were most common.
- Sports-related injuries were observed in 23.9% of cases and road accidents accounted for 23.6% of cases.
- About 89.3% of cases were due to mechanical injuries.
- Injuries involving wood and metallic objects lead to open globe injury in 24.9% and 20.9% of cases, respectively.
- Globe injuries caused by sharp objects were three times more common than blunt trauma incidents, accounting for 56% of eye injuries.
Based on various analyses, the yearly incidence rate of perforating eye injuries (holes in the eye) is 3.5 out of every 100,000 cases in the United States. Another study from Australia found that 2.4 to 7.9 out of every 1,000 non-indigenous and indigenous adults, respectively, became blind in one eye due to blunt trauma. According to global data, around 750,000 patients worldwide are hospitalized each year due to eye injuries. Eye trauma makes up approximately 7% of all body injuries and 10 -15% of all eye-related problems. It is estimated that globally, 1.6 million people are blind due to eye trauma, with 2.3 million people being blind in both eyes and 1.9 million being blind in one eye. Interestingly, about 90% of all eye injuries could be prevented.
Signs and Symptoms of Blunt Eye Trauma (Eye Injury)
When someone has had a traumatic injury to the eye, doctors will usually be suspicious of an injury to the eyeball, or globe. Signs of this could include ongoing pain in the eye, vision problems, or if the person has been using any blood thinning medications. In severe cases of globe rupture, the eye might be misshaped, vision could be reduced or gone altogether, and there might be blood in the front part of the eye. There’s also something called the Seidel sign, which shows leakage from the site of injury when a special stain is used on the eye. However, doctors avoid this test if they can already tell that the globe has ruptured.
Similarly, if a person has suffered a retrobulbar hematoma, or a bleeding behind the eye, this will usually result in severe pain in the eye and bulging of the eye, or proptosis. Vision loss can also be a symptom for this kind of injury. It’s important to note that both of these injuries are serious threats to vision and need immediate attention from an eye doctor.
Other symptoms for both conditions could include swelling around the eye, bruising, or blood under the clear surface of the eye, depending on how the injury happened. Globe rupture might not always alter the shape of the eye noticeably, but it will usually result in eye pain and loss of vision. Similarly, a retrobulbar hematoma might present with eye pain and loss of vision, but the bulging of the eye is a key sign for this condition.
There are many other symptoms and signs that could occur after an eye injury. Here are some that might appear in different parts of the eye:
- Conjunctive issues: bleeding or congestion, a foreign body, or a tear.
- Cornea issues: damage like abrasion or erosion, swelling, a tear, wound or scar, or a corneal ulcer
- Sclera issues: a partial to full-thickness tear with or without the jelly-like substance in the eye pushing through, or a foreign body lodged in the sclera.
- Anterior chamber issue: presence of blood.
- Iris issues: separation of iris root from the ciliary body (structure behind iris), tears in the iris stromal tissue.
- Pupil issues: dilated or constricted pupil, rupture of the pupillary margin.
- Lens issues: cataract (clouding of lens), damage to zonular fibers, or ring impression due to trauma and displacement of lens.
- Globe rupture: can occur with severe blunt trauma.
- Optic nerve issues: avulsion (separation from its attachment) or neuropathy (damage to nerve).
- Vitreous issues: bleeding or detachment, or opacities (clouds) present.
- Choroid issues: rupture, hemorrhage, detachment, or inflammation.
- Retina issues: white cloudiness at the back of the eye, tear or detachment, wound healing related complications, or bleeding.
- Macular issues: swelling, pigmentary degeneration, hole, or cyst.
All these symptoms are critical to evaluate and diagnose the type of injury and its extent correctly. It’s important to remember that any kind of eye trauma could carry a risk of serious complications and should be treated immediately to prevent loss of vision.

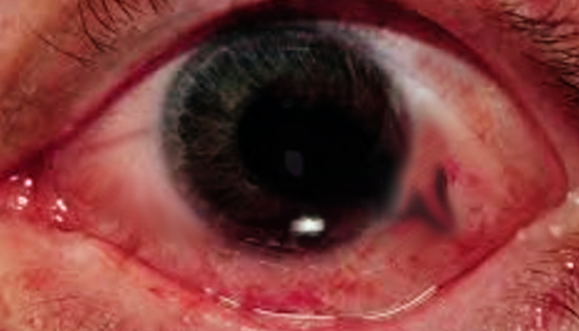
depicting blood staining of the anterior lens capsule
Testing for Blunt Eye Trauma (Eye Injury)
When examining the eyes, the sharpness of vision, also known as visual acuity, should be checked separately for each eye. It’s important to avoid forcing any movements of the eye that may potentially be injured. Any issues with the pupil’s reaction to light also need to be looked into.
In cases of blunt force trauma to the eye, it’s vital to measure the pressure inside the eye. The reason for this is the risk of developing secondary glaucoma, a condition often triggered by trauma that can lead to sudden vision loss. This type of glaucoma can occur because the damage disrupts the eye’s drainage system, causing an unhealthy rise in eye pressure.
Gonioscopy, another eye examination, can be used to look for things like foreign bodies in the eye or blood in certain parts of the eye. This exam is performed under local anesthesia and should be done when the eye isn’t inflamed. The exam can be postponed if the patient is experiencing any pain.
One way to find any damage or defects in the outer layer of the eye is through fluorescein staining. This test involves using a special dye that can highlight any cuts, scrapes, or other issues on the eye’s surface.
Seidel’s test and Forced Seidel’s test are methods used to detect leaks in the eye’s fluid by applying dye and observing any leaks under a special light.
Imaging methods such as X-ray, B scan ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI) can be used to examine the eye and surrounding areas. X-rays can locate foreign objects, whereas B scan ultrasonography is crucial for detecting eye issues like retinal detachment or blood in the eye. Meanwhile, a CT scan can check for additional facial injuries and confirm the diagnosis, while an MRI is useful in detecting hidden injuries behind the eye. However, MRI scans are not used if metallic foreign bodies are suspected.
In cases where visual acuity is questionable, electrodiagnostic tests like electroretinogram (ERG), electrooculography (EOG), and visual evoked potential (VEP) can be used to evaluate the integrity of the optic nerve and retina.
Optical Coherence Tomography is used to examine the macula – the part of the retina responsible for detailed central vision – and to rule out certain eye conditions.
Lastly, along with eye examination, any other head or facial bone injuries that might have occurred with eye trauma should be thoroughly checked as they often accompany serious eye injuries. Minor eye movement can be affected due to eye trauma and should be tested. Any necessary lab tests should be carried out depending on the clinical condition and any use of anticoagulant medicine.
Treatment Options for Blunt Eye Trauma (Eye Injury)
If someone’s eye globe ruptures, the immediate treatment at the emergency department involves actions to prevent the damage from becoming worse or any further loss of fluids from inside the eye. This includes providing anti-vomiting medicine to help prevent an increase in eye pressure and loss of eye fluids caused by vomiting. They will also provide pain killers as required and place a rigid shield over the eye to protect it. Any further touching or moving of the eye should be avoided and the patient should be positioned partly upright.
For a retrobulbar hematoma (bleeding behind the eye), pain relief and anti-vomiting medicine should be given too. The main treatment for this injury is immediate decompression, a procedure that can be done by an emergency doctor or an eye specialist, as fast as possible. This is because a delay of more than 4 hours from the time symptoms start can lead to poorer vision outcomes. Preventive antibiotics can be given to prevent further infection of the eye.
In the case of an eye globe injury or retrobulbar hematoma, it’s important to consult urgently with an eye specialist. Surgery is the definitive treatment for these injuries and should be carried out by an eye specialist.
For blunt eye trauma treatment, the specific action depends on the part of the eye that is affected. Across all cases, observation and specific treatments or surgeries may be required. In the case of injuries to the conjunctiva (the clear tissue covering the white part of the eye), conjunctival congestion, or foreign bodies in the conjunctiva, treatment with topical medication can be used in mild cases. Deeper cases may require surgery.
In the cornea (the clear front surface of the eye), if there’s epithelial damage or corneal edema (swelling), topical medication can be used. In more severe cases, a special type of contact lens or a procedure known as a graft may be necessary. If there’s a corneal tear, which is more serious, surgery is needed.
For lens-related injuries, observation or corrective lenses might be enough in minor cases. If the lens is dislocated, surgery is needed.
If the globe (the eyeball itself) is injured or ruptured, topical antibiotics and protection for the eye are used. Surgery to repair the injury may also be needed.
Damage to the optic nerve, blood-filled vitreous (the clear, jelly-like substance in the middle of the eye), and retina (a layer of tissue in the back of the eye that senses light and sends images to the brain) are more serious issues. Depending on the case, observation, systemic corticosteroids, surgery, or even a lens implant may be needed.
The macula (a part of the retina responsible for sharp, central vision) could develop edema (swelling), degeneration, a hole, cyst, or scar due to trauma. Depending on the type and severity of damage, treatments could range from observation to eye drops, injections, or surgery.
What else can Blunt Eye Trauma (Eye Injury) be?
When someone experiences a strong blunt force to the eye, it can lead to various medical problems. These could include:
- Bursting of the eyeball (known as globe rupture)
- Blood collecting behind the eye (retrobulbar hematoma)
- Eye condition causing increased pressure in the eye leading to vision loss (traumatic glaucoma)
- Blood in the eye’s anterior chamber (hyphema)
- Fracture of the bony floor of the eye socket, sometimes causing trapped muscles (orbital blowout fracture with entrapment)
- Objects that have entered the eye (foreign body)
- Damages to the white outer layer of the eyeball (scleral disruption)
- Bleeding into the jelly-like material that fills up the back part of the eyeball (vitreous hemorrhage)
Doctors need to take all these possibilities into account when treating someone who has suffered a blunt force to the eye.
What to expect with Blunt Eye Trauma (Eye Injury)
The outcome of a blunt eye injury greatly depends on the consequences of the injury. A study has shown that about a quarter of patients with general eye trauma end up with sight loss in one eye. For children, research suggests that vision tends to be better after blunt eye injuries compared to injuries involving penetration, although blunt injuries might lead to higher rates of glaucoma.
However, if the eye has been ruptured due to blunt trauma, the patient’s vision might worsen significantly since it likely indicates a high-speed impact. Certain factors, such as a non-reactive pupil, lack of a red reflection, an initial vision worse than 20/200, and an eyelid cut, might worsen the vision prognosis.
In another study, it was found that a quarter of patients with certain types of retinal injuries from blunt eye trauma had vision worse than 20/30 in the affected eye. Vision also tends to be worse following blunt eye trauma if there is blood in the eye, retina detachment or internal bleeding. Traumatic optic nerve injury also usually leads to a poor vision outcome.
The severity and type of the initial injury are often good indicators of potential poor outcomes. The Ocular Trauma Score is a recognized way of predicting a person’s likely vision outcome following an eye injury.
Possible Complications When Diagnosed with Blunt Eye Trauma (Eye Injury)
Depending on the kind and severity of an eye injury, the complications can be quite different. They can many especially based on where the injury is and how deep it goes. Here are some potential complications:
- Conjunctival Tear
- Corneal Tear
- Corneal infiltrates
- Corneal scarring
- Hyphema
- Hypopyon
- Anterior chamber exudates
- Fibrinous membrane
- Iridodialysis
- Iris prolapse
- Traumatic Mydriasis
- Iridoplegia
- Angle-closure glaucoma
- Post-traumatic glaucoma
- Subluxated lens
- Dislocated lens
- Subluxated IOL
- Dislocated IOL
- Posterior capsular rupture
- Zonular dialysis
- Cataracts
- Retinal Tear
- Retinal detachment
- Choroidal detachment
- Choroidal rupture
- Traumatic optic neuropathy
- Optic nerve avulsion
- Endophthalmitis
- Panophthalmitis
Depending on the extent of the injury, vision loss could be affected to different degrees. In cases of severe trauma where eye surgery can’t help, it may be necessary to remove the entire eye. This is known as enucleation.
Recovery from Blunt Eye Trauma (Eye Injury)
Depending on the reason for the surgery, all patients should be given medication after the procedure. This could include antibiotics, antifungal medication, steroids, or oral anti-inflammatory drugs. It’s important to monitor the patient closely after the surgery to prevent any serious complications.
Preventing Blunt Eye Trauma (Eye Injury)
It’s crucial to inform patients about the importance of wearing eye protection during activities where eye injuries are common. These can include playing sports or riding motorized vehicles and other such situations. Wearing protective goggles or glasses is known to significantly reduce severe eye injuries, even in combat situations.
Particularly, if a person has lost the vision in one eye due to injury, they should always wear protective glasses to protect the sight in their remaining eye, as the loss of vision in this eye could lead to complete blindness. And remember, eye injuries can happen at home, not just when participating in high-risk activities like sports. So, everyone should consider wearing the right eye protection at all times to keep their eyes safe.