What is Central Toxic Keratopathy?
Excimer laser ablation is a common method used in the U.S. to correct minor to average vision problems. It’s usually safe and the yearly rate of complications is less than 0.8% since 2010. A rare complication, called Central toxic keratopathy (CTK), was first identified in 1998. It’s been called by many different names such as stage IV diffuse lamellar keratitis, central lamellar keratitis, and keratinocyte-induced corneal micro edema, among others.
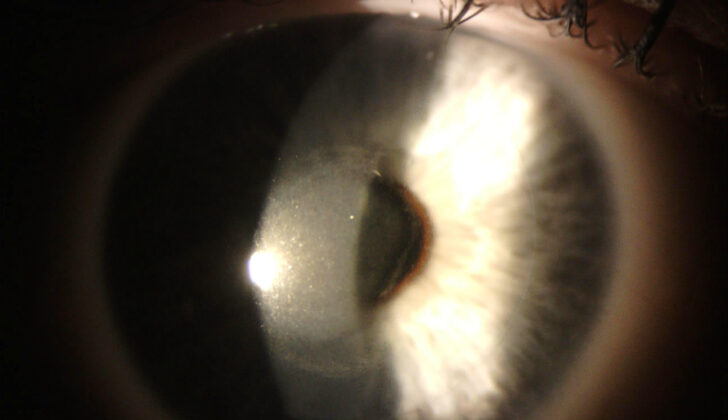
CTK typically appears as a cloudy spot in the center or offset center of the cornea after having excimer laser ablation surgery (like LASIK or photorefractive keratopathy). This can occur within nine days of the surgery. It’s thought not to be due to inflammation, but the exact cause is still not known. Initially, it was thought to be a severe form of another condition called diffuse lamellar keratitis (DLK). However, recent evidence suggests that CTK is a separate condition entirely from DLK.
In addition to its occurrence after certain eye surgeries, there is also a suggestion that CTK might exist in situations other than after refractive surgery. For example, there have been cases of CTK associated with contact lens use, even without recent physical scraping of the eye’s surface. It has also been reported to occur randomly and possibly in response to certain types of laser eye surgery or the use of eye drop anesthesia.
What Causes Central Toxic Keratopathy?
The exact cause of CTK, a certain type of eye condition, is still unknown. It’s been suggested that it could be a reaction to something used during eye surgery, like glove material, secretions from an eye gland, povidone-iodine, or marking pen ink. Another idea is that it might be related to the use of an ultraviolet laser, which could potentially trigger some kind of toxic reaction with these substances. This is because the cloudiness in the eye, characterizing CTK, often appears in the area where the laser is most used.
However, there have been cases in which the cloudy portion appears at the edges of the eye or in people who haven’t had laser surgery. So it’s suggested there might be another cause perhaps related to certain proteins called inflammatory cytokines and metalloproteinases or immune responses that involve antigens and antibodies.
No definitive risk factors for developing CTK have been established yet, due to the uncertain cause. However, because CTK was first noticed as a complication following LASIK surgery, and most reports of CTK occur after laser eye correction, it seems that people getting these procedures might have the highest risk. Plus, in many cases, people with CTK also had a condition called DLK beforehand, so there might be some shared risk factors between the two. But these risks might not be relevant for people who have CTK without a history of recent eye surgery.
Risk Factors and Frequency for Central Toxic Keratopathy
To the best of our knowledge, no studies have been done specifically to figure out how common Central Toxic Keratopathy (CTK) is. However, some research has been done on eyes that have undergone LASIK surgery. In one study, out of 522 LASIK treated eyes, four developed CTK (0.77%). In another study, out of 17,100 LASIK treated eyes, nine developed CTK (0.05%).
Signs and Symptoms of Central Toxic Keratopathy
People who develop Central Toxic Keratopathy (CTK) might first experience symptoms associated with Diffuse Lamellar Keratitis (DLK), another condition that can happen after certain eye laser surgeries. These symptoms can include pain, sensitivity to light, blurred vision, seeing “halos” around lights, feeling like there’s something in the eye, and seeing ‘floaters’. It’s important to mention that having DLK isn’t necessary for a CTK diagnosis. Those diagnosed with DLK after laser eye surgery might also be at risk of getting CTK. Therefore, they should receive appropriate treatment and be watched for signs of CTK.
An eye exam using a special instrument called a slit-lamp, would usually reveal a cloudy area or opacity in the clear front part of the eye (cornea) in people with CTK. This cloudiness, which is different from the common haze seen after certain kinds of laser eye surgery, can lead to a drop in vision. It usually appears within nine days post-surgery and can last from 2 up to 18 months before disappearing on its own. Even after it clears, some people might have ongoing issues, like areas of thinning in the cornea and reduced vision.
A detailed eye exam including Optical Coherence Tomography (OCT) might show alterations in the cornea’s structure, and other techniques could reveal abnormalities like changes in the cornea’s curvature and thinning, both of which might lead to issues with nearsightedness and farsightedness. On top of this, certain specialized imaging methods could point to changes in the cornea’s cells and layers.
Testing for Central Toxic Keratopathy
Diagnosing Central Toxic Keratopathy (CTK), a condition affecting the eye, doesn’t depend on specific imaging or tests, but rather on what doctors observe through a clinical assessment. There are three main signs that may help doctors identify CTK: a non-inflamed blurry spot in the center of the eye, a thinner cornea, and shifts towards farsightedness in vision.
If a patient has recently had a type of laser eye surgery known as excimer laser ablation, or has shown signs of Diffuse Lamellar Keratitis (DLK) in the days before, this may make the diagnosis of CTK more straightforward. However, when patients have not had this type of laser surgery, doctors must be highly alert to the possibility of CTK to ensure they diagnose it correctly.
Treatment Options for Central Toxic Keratopathy
Treatment approaches for Central Toxic Keratopathy (CTK), a unique syndrome that affects the cornea of the eye, have shifted dramatically due to recent insights. Previously, treatments relied heavily on steroid-based medications. However, new research suggests that steroids might actually hinder the process of the eye’s repair by blocking specific cells from rebuilding the eye’s structure. As such, experts now advise using steroids only until the cornea becomes opaque and white blood cell count drops. After this point, continued use of steroids might not only be useless but could expose the patient to unnecessary drug side effects.
In many cases, close follow up and regular monitoring without any invasive treatment are often recommended, as the cloudy appearance in the cornea associated with CTK typically tends to clear on their own.
Though there’s no standard treatment for CTK, a few other medical options may be beneficial. For instance, doxycycline, which is known to prevent cell breakdown in the cornea, may be effective. Vitamin C could also promote the healing process in the cornea. That said, using mitomycin-C, a medicine commonly used in laser procedures to reduce post-surgery clouding, may not be advisable, as it may further reduce cells required for the eye’s repair.
While surgical interventions are generally not recommended due to the risk of tissue loss and thinning, some report that certain procedures might speed up recovery. For example, a form of surgical treatment called “flap lift and irrigation” was found to halt disease progression in one patient. Some even suggest that removing a part of the eye’s flap could correct vision problems related to CTK.
Regardless of whether a treatment path involves medication-only or includes surgery, it’s crucial for patients to have regular follow-ups for eye tests. These include topography, tomography, confocal microscopy, and OCT imaging to closely monitor any changes in the cornea and vision. Such careful monitoring could also contribute to a better understanding of CTK and its long-term effects.
What else can Central Toxic Keratopathy be?
When trying to diagnose Central Toxic Keratopathy (CTK), a variety of conditions might seem similar at first glance. These health issues can also cause changes in vision or make the center of the eye (the cornea) cloudy or opaque.
In the past, CTK was believed to simply be a severe form of Diffuse Lamellar Keratitis (DLK). However, we now understand that CTK and DLK are two different problems. The clarification between the two becomes crucial when both conditions coexist. Unlike DLK, which keeps the cloudiness within a specific part of the cornea, CTK’s cloudiness can spread to the front of the corneal flap and the remaining ‘stromal bed’ at the back.
Infectious Keratitis may also lead to a dense cloudiness in the middle of the eye. But unlike CTK, it doesn’t result in swelling as there’s no inflammation and it lacks the typical pale yellow color of inflammatory wounds. Besides, Infectious Keratitis may show other signs that are nontypical to CTK, like spreading, reddened eyeball, eye discharge, appearance of inflammatory cells, and a response from the anterior chamber of the eye.
Treatments such as Corneal Cross-Linking (CXL) and Photorefractive Keratectomy (PRK) might also show post-surgery haziness, causing confusion with CTK. The difference is, this sort of haziness tends to appear more than a month after surgery, whereas CTK would usually show up within nine days.
Finally, other diagnoses to consider when diagnosing CTK are: fluid or debris in the interface, an immediate steroid reaction, heightened eye pressure causing haziness, superficial punctate keratitis (tiny bumps on the surface of the cornea), and trauma.
What to expect with Central Toxic Keratopathy
The outlook for patients with CTK can often be decent to good. Over time, the central cloudiness tends to lessen somewhat and the thickness of the middle layer of the eye (stroma) often increases. That said, some patients may continue to have lingering vision defects, which can be disappointing, particularly for those who initially elected to have laser surgery with the hope of perfect vision without glasses or contact lenses.
On a more positive note, patients can choose to have additional surgery once the cloudiness subsides to minimize any remaining vision distortion and correct any continuing vision issues, without the CTK coming back.
Possible Complications When Diagnosed with Central Toxic Keratopathy
If Corneal Transplant Keratoconus (CTK) is not diagnosed or is poorly managed, the patient’s condition could worsen. As mentioned before, continuing steroid treatment could also delay improvement or make the disease worse. Even after the main symptoms lessen, some complications may linger, such as residual striae (scarring) and hyperopia (farsightedness). But don’t worry – these issues can be treated with eye surgery that corrects focus.
Common Complications:
- Worsening of patient’s condition due to undiagnosed or poorly managed CTK
- Delay in improvement or exacerbation of the disease due to continued steroid treatment
- Residual striae (scarring) even after the main symptoms lessen
- Hyperopia (farsightedness) which lingers even after the disease has mostly cleared
Preventing Central Toxic Keratopathy
The exact cause of CTK, a certain eye condition, remains unknown and there are reports of cases where no specific triggering event could be identified. Therefore, no concrete advice can be given on how to prevent or reduce the chances of developing CTK. However, a large number of the cases have been linked with laser eye surgery and elective visual correction surgery. Though these complications are rare, it’s crucial for patients to understand before the operation that these surgeries carry certain risks and could possibly lead to unfavorable outcomes.