What is Valsalva Retinopathy?
Valsalva retinopathy is a specific type of eye condition where bleeding occurs in front of the retina, typically due to increased pressure in the chest area. This condition was first described by Thomas Duane in 1972. It’s important to know that anyone, regardless of their health condition, can experience Valsalva retinopathy. In nearly all instances, the bleeding within the eye resolves on its own and eyesight returns to normal. However, the exact recovery may depend upon where the bleeding has occurred within the retina.
What Causes Valsalva Retinopathy?
Certain everyday activities can cause this condition, particularly those that involve the Valsalva maneuver. The Valsalva maneuver describes actions where you forcefully exhale without actually releasing air, like when you’re straining or holding your breath. These actions can include weight lifting, vomiting, coughing, sneezing, aerobic exercises, straining during constipation, playing wind instruments, engaging in physical activities, during sexual intercourse, after heart or lung resuscitation, and compression injuries.
There are also certain health conditions linked to this one:
* Proliferative diabetic retinopathy (PDR) – This is a complication of diabetes that affects the eyes. There’s an instance where a patient with PDR developed bleeding within the eye’s jelly-like filling (known as a vitreous hemorrhage) during an extended bout of vomiting after an eye test using a special dye.
* Congenital retinal macrovessel – This is an unusual, large blood vessel in the retina, the tissue at the back of the eye that senses light.
* Hypertensive retinal angiopathy – This refers to damage to the retina’s blood vessels due to high blood pressure.
* Congenital changes in retinal vessels including retinal arterial tortuosity and retinal telangiectasis – These are conditions you’re born with where the blood vessels in the retina twist unnaturally or become abnormally widened and dilated.
Risk Factors and Frequency for Valsalva Retinopathy
According to available research, there’s no specific age, gender, or race that’s more likely to be affected.
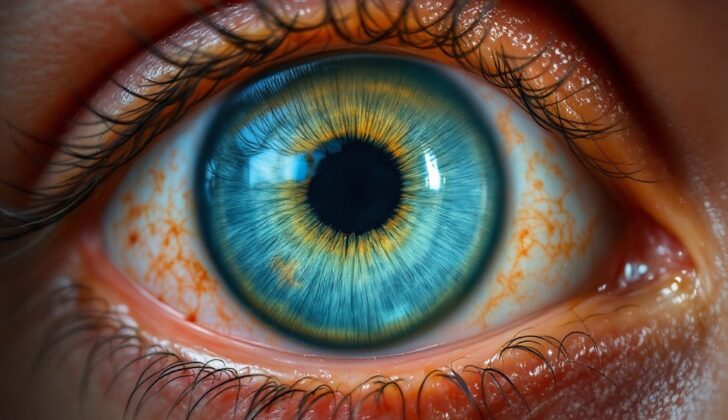
Signs and Symptoms of Valsalva Retinopathy
Valsalva retinopathy is a condition that can cause sudden, painless vision loss, usually in one eye (though sometimes in both). It often occurs after actions that involve a strong force of blowing or pushing, like coughing, vomiting, heavy sneezing, lifting weights, playing blowing instruments, or intense childbirth. Patients might describe their symptoms as seeing a black spot, spots moving in the eye (floaters), a red tinge to their vision, or blurred vision. The severity of these symptoms can vary based on the level and location of the internal bleeding in the eye.
Here’s what healthcare professionals often look for to diagnose Valsalva retinopathy:
- A very small, defined area of hemorrhage in the eye
- The hemorrhage might be round, oval, or ‘dumb-bell’ shaped
- Usually the hemorrhage covers more than one ‘disc area’
- The bleed is ‘pre-retinal’, occurring in front of or around the fovea, an important vision area in the eye.
- The internal surface of the eye (the ILM) can look like a smooth lump with a shiny surface, featuring striations on the hemorrhage.
- In the acute (early) stage, the blood is a bright red raised area, moving slightly when the eye moves. The blood can appear to be layered or ‘settled’.
There can be a ‘double ring sign’ if blood is trapped in two areas – the sub-ILM and subhyaloid spaces. The eye can also have multiple lesions, some located away from the macula (central vision region). In some instances, the pre-retinal hemorrhage may be quite small and might resemble a strawberry due to yellowish-white spots.
There can be other ocular signs like subconjunctival hemorrhages or petechial hemorrhages of the eyelids, among several others. Once the hemorrhage clears, the only sign might be a cavity formation at the level of the bleed, such as a sub-ILM cavity or serous detachment of the ILM. This can look like a neurosensory detachment.
Over time, the hemorrhage may lose its red color as the blood loses its oxygen, turning yellow, and then white.
Testing for Valsalva Retinopathy
During a medical check-up, your doctor might look for signs of a condition called Valsalva. This can include a slow heart rate (bradycardia), increased blood pressure in your arms and legs, and tiny red or purple spots on your skin (petechial hemorrhages).
Your doctor will also check if there are other health issues that could contribute to Valsalva, such as anemia (a condition that means you don’t have enough healthy red blood cells), sickle cell disease (a genetic disorder affecting the red blood cells), idiopathic thrombocytopenic purpura (a disorder causing excessive bruising or bleeding due to low platelets), diabetes, and high blood pressure. To do so, they could conduct several tests like counting the number of cells and platelets in your blood, checking your blood sugar level after fasting, measuring your blood pressure, and performing some specialized blood tests (prothrombin time and activated partial thromboplastin time). They might also run an electrophoresis test on your hemoglobin (the component in your blood that carries oxygen) to rule out sickle cell anemia.
In addition, your doctor will also check on your eyes. They will test your corrected visual acuity, which basically means they will examine how well you can see. They also check the pressure inside your eyes, your pupils’ reaction to light, as well as conduct a thorough evaluation of your eyes. If there is bleeding under the conjunctiva (the clear tissue covering the white of your eye), it is called a subconjunctival hemorrhage.
Your doctor may also use a special type of scan called optical coherence tomography to identify where the bleeding is happening inside your eye and decide whether treatments such as laser therapy or surgery are needed. Fundus fluorescein angiography, a procedure that uses a special dye and camera to examine the blood vessels and other structures at the back of your eye, could also be performed to look for abnormal blood vessels and other diseases affecting the retina. Your doctor may take a fundus picture to keep track of how the disease progresses over time. If the bleeding goes beyond the vitreous, which is the jelly-like substance filling your eyes, a B-scan ultrasound could be required.
Treatment Options for Valsalva Retinopathy
If you are diagnosed with Valsalva retinopathy, a condition caused by a sudden increase in pressure that leads to bleeding in the eye, your treatment will depend on where the bleeding is located in your eye. Most of the time, doctors recommend monitoring the condition, as it often improves on its own. However, if there’s a large amount of blood in the area of your eye responsible for sharp, central vision, known as the macula, you might need to be treated right away.
The first step in treating Valsalva retinopathy is to manage any issues that might have contributed to the condition. For instance, if you have constipation, your doctor might recommend taking a laxative to make it easier for you to have bowel movements. Additionally, you might be advised to avoid taking blood-thinning medications and doing strenuous exercises, as these might make your condition worse. To help the blood in your eye settle down, your doctor might advise you to prop your head up. In some situations, blood in the eye can last as long as six months before it finally clears up.
In certain scenarios, a type of laser treatment might be recommended. This can be useful if there’s a large amount of blood that’s obscuring your macula for less than three weeks. In this process, a laser is used to create a small opening in one of the layers of your eye, allowing the blood to move to a different part of your eye. The laser is aimed at an area away from large blood vessels and away from the center of your field of vision. This treatment can help improve your sight. However, there can be complications from laser therapy including the development of a tear in the retina, additional bleeding, formation of scar-like tissue, retinal detachment, or further loss of vision.
In the event that you have a long-standing bleeding in the eye, or if there’s so much blood in the eye that your doctor can’t examine your retina, then a surgery called a vitrectomy might be needed. This procedure involves removing some or all of the jelly-like substance that fills your eye, also known as the vitreous humor.
What else can Valsalva Retinopathy be?
In some unusual cases, doctors might come across eye conditions that appear similar to Valsalva retinopathy, even though there have been no events of Valsalva maneuver. Some of these conditions include:
- Diabetes-triggered proliferative vascular retinopathies, retinal vein occlusion, etc. These require ruling out of any new blood vessels at the optic disc.
- Hypertensive retinopathy
- Sickle cell anemia
- Physical abuse injuries, which in severe cases can lead to something called battered baby syndrome
- Terson syndrome
- Rupture of a large blood vessel, also known as a macroaneurysm
- Anemic retinopathy
- An acute episode of the jelly-like substance pulling apart from the retina in the eye, called posterior vitreous detachment. This too might give rise to hemorrhages, thus necessitating ruling out peripheral retina tears
Apart from Valsalva retinopathy, there are a limited number of eye issues where you can see bleeding across multiple layers of the retina i.e., pre-retinal, intraretinal, and subretinal. These include Valsalva retinopathy, anemic/leukemic retinopathy, and physical trauma like battered baby syndrome.
Sometimes, pre-retinal hemorrhage, the same as those in Valsalva retinopathy, can occur in people with no history of Valsalva or exertion. In these situations, there may be some blood vessel diseases in the retina (like hypertension or diabetes), issues with blood clot cell accumulation, or the person might be on blood-thinning medication. Some patients with repetitive instances of pre-retinal bleeding might have a family history of the same, hinting at a possible hereditary disease.
What to expect with Valsalva Retinopathy
The outlook is often positive, with the bleeding usually clearing up on its own within a few weeks to months. However, how well your vision recovers depends on where the bleeding is in the back of your eye (the fundus) and which layer of the eye is affected by the bleed. If the bleeding occurs at the macula, the central area of your retina, it can have negative effects. This could be due to the presence of iron contained within the blood’s hemoglobin, pressure effects, or fibrosis (the thickening and scarring of connective tissue) once the bleeding has cleared up.
Possible Complications When Diagnosed with Valsalva Retinopathy
Permanent visual loss could occur if there is a subretinal hemorrhage at the macula, which is a part of the retina in the eye responsible for sharp, clear, central vision. Additionally, if a hemorrhage is present for a long time, changes in the ERG, which is a test to detect problems with the retina, could be observed. This happens when ferritin, derived from blood that has lost its oxygen-carrying component (hemoglobin), gets deposited within cells of the Retinal pigment epithelium, which is a layer of cells at the back of the eye.
Common Eye-related Issues:
- Permanent visual loss due to subretinal hemorrhage at the macula
- Changes in ERG caused by long-standing hemorrhage
- Deposition of ferritin within Retinal pigment epithelial cells
Preventing Valsalva Retinopathy
Patients should be reassured that the outlook is generally good if they have Valsalva retinopathy, a condition where a sudden increase in pressure in the chest or abdomen causes tiny blood vessels to break in the eyes. However, it’s not possible to determine who might be at risk. To help prevent this, patients should avoid holding their breath for too long while doing things that require effort, such as weight lifting, sneezing, or coughing. Instead, it’s recommended to take multiple breaths during these activities, as this can help manage the pressure and reduce the risk of experiencing this eye condition.