What is Granular Cell Tumor?
Granular cell tumors are a kind of growth identified as early as 1926 by a Russian scientist named Abrikossoff. At first, people thought these tumors originated from muscle cells, which is why they were initially known as granular cell myoblastomas. But with the help of modern tools that allow us to study cells in detail, we now think these tumors come from Schwann cells, a type of cell that covers nerve fibers. However, there’s a type of granular cell tumor that doesn’t show typical features of nerve tissue, indicating that they might come from different sorts of cells.
These uncommon tumors are usually found in the skin, mouth, digestive system, and just beneath the skin. But, they can appear anywhere in the body like the breast, bladder, nervous system, and the urinary and respiratory systems. Though they can affect anyone regardless of age and gender, they are commonly seen in women between their 40s and 60s. Granular cell tumors are usually single, painless lumps less than an inch and a half in size. Sometimes, they are discovered by accident.
In most cases, granular cell tumors grow slowly and are not harmful. However, about 1% to 2% of these tumors can turn malignant, meaning they can spread and are harmful. If a tumor is malignant, it can lead to a grim health outlook and the only definitive cure is to remove it surgically.
What Causes Granular Cell Tumor?
The origins and development of granular cell tumors are still not fully understood, and their genetic makeup is still mostly a mystery. We do know that these tumors might have reoccurring genetic changes, especially in people who have specific syndromes. But we’ve only recently started to understand the genetic changes that cause these tumors in individuals who do not have genetic syndromes, thanks to new technologies like whole-genome sequencing.
Certain syndromes like Noonan syndrome, neurofibromatosis I, and LEOPARD syndrome have been linked with the appearance of multiple granular cell tumors. Researchers found PTPN11 gene mutations in tumors connected with LEOPARD and Noonan syndromes. It’s also been suggested that multiple granular cell tumors might be caused by abnormal cell signals from the RAS/MAPK pathway–this mutation is common to all three syndromes. in another study, granular cell tumors have also been linked to PTEN gene mutations in people with PTEN hamartoma tumor syndrome.
But it’s important to know that these links between syndromes and gene mutations haven’t been confirmed in large-scale studies yet. They are often based on individual case studies or small groups of cases. In fact, one study that attempted to confirm the importance of PTEN and PTPN11 mutations couldn’t find either of them, but instead found KDR, GNAQ, and ATM mutations in some granular cell tumors.
Researchers have also found a type of granular cell tumors that are not related to nerve cells (non-neural). These tumors don’t react to the S100 protein but do carry an ALK gene mutation.
More recently, whole-genome sequencing was used to find ATP6AP1 and ATP6AP2 mutations in granular cell tumors. These mutations were discovered in 72% of studied cases in a 2018 study. These mutations cause an accumulation of certain proteins inside the cell and result in the characteristic appearance of these tumors. What’s interesting is that these two mutations are very rare in other types of cancer. Further research in 2019 confirmed that these mutations are indeed present in many granular cell tumors.
In the case of malignant granular cell tumors, genome sequencing has found mutations in the BRD7 gene and in the GFRA2 pathway. Other studies reported that some malignant granular cell tumors also have mutations in the ATM, ASXL1, NOTCH2, and PARP4 pathways, as well as some genetic losses in certain chromosomes.
Risk Factors and Frequency for Granular Cell Tumor
Granular cell tumors are not common and appear mostly in people between the ages of 40 and 60. Women are more likely to have these tumors than men. While more cases of benign (non-cancerous) tumors are reported in African-American patients, a majority of the cases of malignant (cancerous) tumors are seen in Caucasian patients.
As per a study, over a period of 32 years, the overall occurrence of granular cell tumors in surgical samples was a mere 0.03%. Most people have only one tumor, but some might have more than one. These tumors can be located anywhere in the body, but they are often found in the head and neck region.
- About 30% of these tumors affect the skin and the tissue beneath the skin (subcutaneous tissue).
- In 15% of cases, these tumors affect the breasts.
- They affect the respiratory tract in 10% of cases.
- The digestive tract is affected in 5% to 11% of cases.
- Only a small number (1% to 2%) of these tumors turn out to be malignant.
Signs and Symptoms of Granular Cell Tumor
Granular cell tumors are usually skin-colored or brown-red, harmless, and develop slowly. They often form as small lumps under the skin, typically in the head and neck. These lumps are usually less than 3-4 cm in size. However, they can appear anywhere in the body, most prominently in the skin, mouth, stomach, breasts, and respiratory tract. The concentration of these tumors in the tongue and skin may be due to the high number of peripheral nerves in these regions. In rare instances, they can form in several places like the urinary tract, thyroid gland, neurohypophysis (part of the brain), and pancreaticobiliary system (responsible for making and releasing bile and digestive enzymes).
Sometimes, these tumors can present as multiple nodules. If this occurs, it is essential to examine the patient for symptoms of conditions like Noonan syndrome, neurofibromatosis type I, and LEOPARD syndrome.
In the breasts, granular cell tumors can occur anywhere, including all four quadrants, the axilla (armpit), and nipple. Seventy percent of these cases are detectable as lumps that can be felt under the skin. Some may be detected incidentally or during screening without a conspicuous lump. Although they are usually pain-free, some people have reported pain, itching, skin retraction or dimpling, and lymph node inflammation.
In the gastrointestinal tract, such tumors are often found during routine checks and are usually symptomless. However, these tumors are most commonly detected in the lower esophagus, then the duodenum (first part of small intestine), anus, and stomach. Cases in the colon, biliary tract (the duct system that transports bile), and rectum are also reported. Some people may exhibit nonspecific symptoms such as burping, difficulty swallowing, abdominal bloating, or blood in stool. During endoscopy, these tumors may appear as a hard, light grey lump sitting below the normal skin-like covering (mucosa) of the digestive tract or on the mucosa itself, resembling ordinary digestive polyps.
In the oral cavity, the tumors mostly occur at the front of the tongue. They form a solid, yellow or pink, painless, single nodule. While these can also be seen on the lip, palate, and inner mouth, they are found in these locations in less than 20% of oral cavity granular cell tumors.
In the neurohypophysis (back part of the pituitary gland in the brain), these tumors are often symptomless and usually found during post-mortem examinations. Rarely they cause symptoms like visual impairment due to mass effect, headache, or symptoms related to high prolactin levels.
- Malignant (cancerous) forms of these tumors often present as lumps beneath the skin, most commonly in the lower limbs.
- They are usually larger than benign (non-cancerous) ones and may already have metastasized (spread) to the lungs, lymph nodes, and bones at the time of diagnosis.
- Clinical warning signs associated with malignant tumors include rapid growth, ulceration (formation of ulcers), invasion of the surrounding structures visible on radiological images, and a size larger than 5 cm.
Testing for Granular Cell Tumor
In some cases, imaging tests, like MRI scans, may not be needed before removing small, harmless-looking lumps in the skin or mouth. However, for tumors in places like the gastrointestinal tract, breast, soft tissue of the arms or legs, or other uncommon areas, imaging is often used. This is because these tumors can’t be easily identified from other harmless or cancerous growths just by looking at them.
In the case of granular cell tumors, which can occur in the muscles, MRI scan is the best imaging method to understand if they are benign (non-cancerous) or malignant (cancerous). Benign granular cell tumors in muscles may appear the same intensity or brighter than the muscle on certain imaging techniques. They are often round or oval in shape, less than 4 cm wide, and close to the skin’s surface. Malignant forms, or cancerous ones, often show different signals on certain imaging sequence, might be bigger than 4 cm, and might invade nearby structures.
Evaluating lumps in the breast can be challenging, as their imaging findings can resemble breast cancer. They may appear as small, round, clearly outlined lesions that are less than 3 cm on mammograms. In ultrasound findings, they are often seen as irregular, firm masses which might not have clear edges or boundaries. On MRI scan, benign and cancerous lesions in the breast present similar imaging findings to those in muscles.
For granular cell tumors in the esophagus, ultrasound and MRI finding varies. They are more often seen as hypoechoic, homogeneous, and smooth-edged, although other descriptions have been reported.
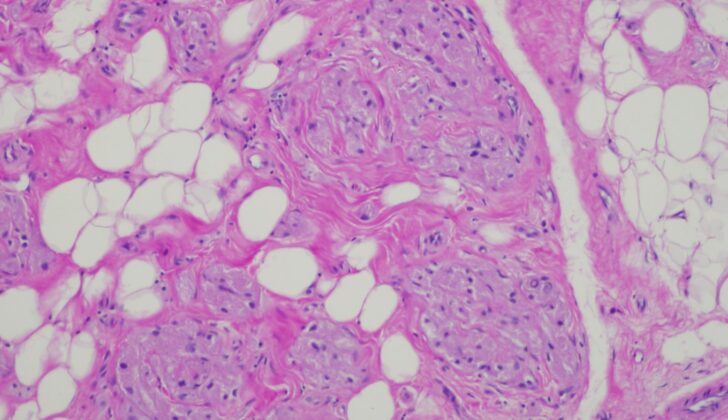
Given that granular cell tumors and other benign or malignant tumors may have similar clinical signs and radiologic findings, doctors usually require a biopsy for microscopic examination to confirm the diagnosis. This is a procedure where a small sample of tissue is removed for examination in a lab. Both benign and malignant tumors have particular microscopic findings, so removing the entire lump rather than just a small piece is preferred to avoid any chance of missing parts of the tumor that could exhibit malignant characteristics.
Treatment Options for Granular Cell Tumor
For granular cell tumors, which can be either benign (not cancerous) or malignant (cancerous), the recommended treatment is to remove the entire tumor with surgery. This procedure is typically followed by regular check-ups. If the tumor is small, it can usually be removed in its entirety for diagnosis. However, for larger tumors, a biopsy (sample of the tissue) is usually taken first before the remainder of the tumor is removed with surgery. Particularly for tumors found in important areas for appearance or function, a specific type of surgery called Mohs surgery is sometimes used to ensure complete removal while sparing as much healthy tissue as possible. A procedure called sentinel lymph node biopsy, which tests for the spread of cancer, is only advised if a tumor appears to be malignant. Similarly, removal of the lymph nodes is generally only suggested if they can be felt during a physical exam or if it is confirmed that the cancer has spread to the lymph nodes.
Chemotherapy and radiation therapy have a limited role in the treatment for these tumors. There are a few isolated reports of successful treatment using these methods for malignant tumors and cancer that has spread at the time of diagnosis. A drug called pazopanib, which is typically used for a type of cancer called sarcoma, has been reported to treat recurring malignant granular cell tumors in a few cases. However, there is currently no standard chemotherapy plan for this type of tumor due to the lack of relevant clinical trials. The use of radiation therapy after surgery (adjuvant radiation therapy) is a controversial topic, with inconsistent recommendations. Radiation therapy is sometimes suggested for recurring malignant tumors or for cancer that has spread and cannot be removed with surgery.
In terms of tumors in the digestive tract, it is important to follow up after the initial examination (endoscopy), using an endoscopic ultrasound to determine the size, location, and depth of the tumor. This information will help determine the best treatment approach. In contrast to other locations, small (less than 1 cm), symptom-free tumors in the esophagus can be monitored with repeat endoscopic ultrasounds. Tumors larger than this, those causing symptoms, those growing quickly, or those suspected of being cancerous are removed with surgery. A type of surgery called endoscopic mucosal resection is used for benign tumors under 2 cm, while a different type of surgery (submucosal endoscopic resection) is used for benign tumors between 2 to 3 cm that are located in the submucosa (a layer of the digestive tract). For tumors located deeper in the stomach wall, conventional open surgery or video-assisted thoracoscopic surgery is usually required.
In the colon, the best strategies for removing benign tumors less than 2 cm are endoscopic mucosal resection or endoscopic submucosal dissection. Some recommend a technique called endoscopic submucosal excavation for benign tumors up to 5 cm, with more traditional surgery for those larger than this and for malignant growths. However, there is some disagreement, with others advising polypectomy (removal of polyps) for tumors under 4 cm, and colectomy (removal of parts of the colon) for any growth larger than 2 cm.
What else can Granular Cell Tumor be?
When diagnosing granular cell tumors, doctors need to consider a wide range of other potential conditions due to the varied location of these tumors. Some of these other conditions might include:
- Alveolar soft parts sarcoma
- Adnexal tumors
- Apocrine carcinoma
- Basal cell carcinoma
- Cholangiocarcinoma
- Colonic adenoma
- Cystic lesions
- Dermatofibroma
- Dermoid cyst
- Desmoid tumor
- Duct ectasia
- Fat necrosis
- Fibroadenoma
- Fibrosarcoma
- Gastrointestinal stromal tumor
- Granulomatous mastitis
- Hidradenoma
- Hypertrophic scar
- Invasive mammary carcinoma
- Irritation fibroma
- Keloid
- Leiomyoma
- Leiomyosarcoma
- Lipoma
- Malignant fibrous histiocytoma
- Neurofibroma
- Nodular fasciitis
- Oncocytic renal cell carcinoma
- Prurigo nodularis
- Regressing verruca
- Rhabdomyosarcoma
- Sclerosing adenosis
- Schwannoma
- Steatoma
- Traumatic neuroma
There are also some other conditions that show similar findings under the microscope (histologic differential). They have similar physical appearances or granular variants. These include:
- Alveolar soft parts sarcoma
- Ameloblastoma
- Angiosarcoma
- Atypical fibroxanthoma
- Basal cell carcinoma
- Congenital granular cell epulis
- Dermatofibroma
- Dermatofibrosarcoma protuberans
- Epithelioid histiocytoma
- Fibroxanthoma
- Granular cell dermatofibroma
- Hibernoma
- Leiomyoma
- Leiomyosarcoma
- Lobomycosis
- Malignant fibrous histiocytoma
- Malignant peripheral nerve sheath tumor
- Melanocytic nevus
- Melanoma
- Neurofibroma
- Non-neural granular cell tumor
- Primitive polypoid granular cell tumor
- Reactive granular cell change
- Reticulohistiocytoma
- Rhabdomyoma
- Rhabdomyosarcoma
- Schwannoma
- Squamous cell carcinoma
- Trichoblastoma
- Xanthoma
What to expect with Granular Cell Tumor
Benign granular cell tumors have a very good prognosis, meaning that the recovery outlook is outstanding. This is because they can be completely removed through surgery, which typically cures the patient. A “benign” tumor isn’t cancerous; it just means it doesn’t spread to other parts of the body. There have been few instances where these benign tumors spread to other areas. If surgery completely removes the tumor, the chances of it coming back is as low as 2% to 8%. However, if some parts remain, the recurrence rate can be anywhere between 21% and 50%.
On the other hand, malignant granular cell tumors have a significantly worse outlook. The term ‘malignant’ refers to cancer that spreads to other parts of the body. Patients with these types of tumors have survival rates of 74% after 5 years and 65% after 10 years from the time of diagnosis. The tumor could reappear in 32% to 41% of cases and could spread in 11 to 62% of cases within 3 to 37 months after being diagnosed. Survival rates are lower (51%) for patients who have tumors that are larger than 5 cm compared to those with tumors smaller than 5 cm (90% survival rate). If the cancer has already spread to other parts of the body at the time of diagnosis, there is a 0% survival rate at 5 years, compared with a survival rate of 81% for those who do not have spreading.
Possible Complications When Diagnosed with Granular Cell Tumor
The possible complications after a surgery can include:
- Getting an infection at the surgical spot
- Disease recurrence
- The disease spreading to nearby or distant parts of the body
- Unattractive surgical scar
- Invasion and damage of neighboring tissues
- Discomfort due to the effects of swelling (difficulty swallowing, nerve pinching, constipation, a feeling of fullness in the abdomen, loss of peripheral vision in both eyes, and overproduction of prolactin)
Preventing Granular Cell Tumor
After the removal of granular cell tumors, patients should keep an eye out for new or returning growths. This is especially important if the tumor was cancerous. Patients should also remember to attend their scheduled check-ups for monitoring any potential spread of the tumors, or for any small tumors in the esophagus that were not taken out. Regular check-ups allow doctors to find and treat new tumors as early as possible.
Patients who have more than one granular cell tumor should also be given information about the potential link with certain genetic conditions, including neurofibromatosis I, Noonan syndrome, and LEOPARD syndrome. These conditions involve an array of symptoms like the presence of small, dark skin spots (lentigines), heart rhythm abnormalities (electrocardiogram (ECG) conduction abnormalities), widely spaced eyes (ocular hypertelorism), narrowing of the heart’s main valve (pulmonic stenosis), abnormal genitalia, slow growth, and hearing loss caused by damage to the inner ear (sensorineural deafness). Patients with signs of these conditions should have a detailed examination and further testing to confirm or rule out these diagnoses.