What is Portal Hypertension?
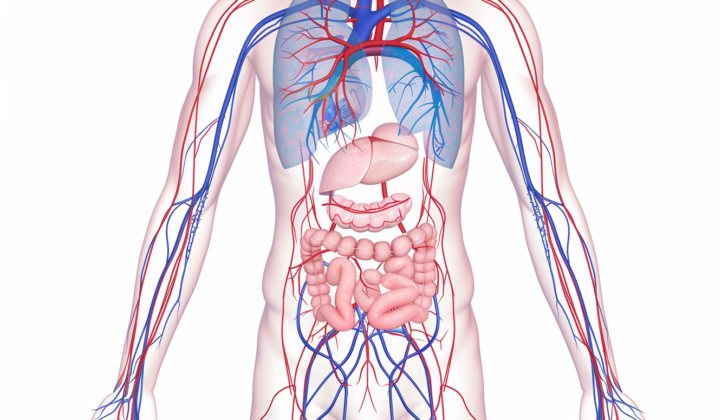
Portal hypertension is a condition where the pressure within the network of veins that carries blood from the stomach, intestine, spleen, and pancreas to the liver (also known as the portal venous system) is abnormally high. The pressure difference, or gradient, between the portal vein and the vein in the lower part of the torso (the inferior vena cava) or the liver vein, should normally be equal to or less than 5 mmHg.
If this pressure difference or gradient increases to 6 mmHg or more, then it’s closely linked to the presence of portal hypertension in many cases. Portal hypertension can become a significant health concern if the pressure gradient exceeds 10 mmHg. A pressure gradient between 5 to 9 mmHg usually indicates an underlying disease that’s not showing symptoms yet and this gradient is measured through the hepatic venous pressure gradient (HVPG).
This condition often develops when there’s an increased resistance to the flow of blood within the portal venous system. It can happen inside the liver, like in cirrhosis, or outside the liver, such as before the liver in portal vein thrombosis or after the liver in conditions like constrictive pericarditis or Budd-Chiari syndrome. Knowing where the resistance to blood flow is can help identify the cause of portal hypertension.
This health issue often causes hospitalization, bleeding in swollen veins (variceal bleed), the need for liver transplantation, and death in patients with cirrhosis. The term “portal hypertension” was first introduced by Gilbert and Carnot in 1902.
What Causes Portal Hypertension?
Portal hypertension happens for many reasons. These reasons are categorized into either pre-liver, within the liver, or post-liver.
Pre-liver causes are either due to too much blood flow or a blockage in the portal or splenic vein. Too much blood flow can occur in conditions like unexplained tropical spleen enlargement, unusual connections between arteries and veins, or a fistula (abnormal connection between organs). A blockage in the portal or splenic vein can happen due to blood clots or a tumor pressing on or invading these veins.
Causes within the liver can be sorted into pre-sinusoidal, sinusoidal, or post-sinusoidal. Pre-sinusoidal causes can happen due to diseases like schistosomiasis (a disease caused by parasitic worms), congenital hepatic fibrosis (a rare disease that affects the liver), early primary biliary cholangitis (a disease that slowly destroys the liver’s bile ducts), sarcoidosis (a disease that causes clusters of cells to form in organs), chronic active hepatitis (long-term liver inflammation), and toxins such as vinyl chloride, arsenic, and copper. Sinusoidal causes are related to conditions like cirrhosis (scar tissue replaces healthy liver tissue), alcoholic hepatitis, vitamin A intoxication, or certain drugs. Post-sinusoidal causes arise from disorders like sinusoidal obstruction syndrome or veno-occlusive disease (blockage of small veins in the liver).
Lastly, post-liver causes can occur at the level of the heart, the hepatic vein (as in Budd-Chiari syndrome), or the inferior vena cava (a large vein that carries deoxygenated blood from the lower and middle body to the heart). If these causes occur at the level of the heart, they’re due to a rise in atrial pressure, as in constrictive pericarditis (inflammation and hardening of the tissue around the heart). If they rise at the level of the inferior vena cava, they’re due to narrowing, blood clots, web-like formations, or tumor invasion.
Risk Factors and Frequency for Portal Hypertension
Cirrhosis, also known as liver scarring, is the main reason behind high blood pressure in the large vein that carries blood to the liver, known as portal hypertension, in Western countries. On the other hand, in Africa, where there is a high occurrence of a disease called schistosomiasis, this disease is the leading cause of portal hypertension.
Signs and Symptoms of Portal Hypertension
Often, people living with portal hypertension do not experience symptoms until complications occur. One of the most frequent signs of this condition is vomiting blood, which originates from ruptured varices or blood vessels. Some patients might have black, tarry stools (also known as melena) without any bleeding.
The majority of portal hypertension cases are caused by liver cirrhosis, thus patients could also show signs of this underlying condition. These symptoms include:
- Yellowing of the skin and eyes, known as jaundice
- Enlargement of the male breasts or gynecomastia
- Red palms or palmar erythema
- Small, spider-like blood vessels visible on the skin, known as spider nevi
- Shrinking of the testicles or testicular atrophy
- Fluid accumulation in the abdomen or ascites
- Swollen feet or pedal edema
- Trembling or flapping of the hand when extended due to buildup of toxins in the blood or asterixis
Additionally, there might be visible veins on the abdominal wall, a result of the body’s attempt to redirect blood flow around the blockage in the portal vein. These may present as caput-medusae, where the blood flows away from the belly button, or in cases of inferior vena cava obstruction, where the blood flow is towards the belly button.
In Cruveilhier-Baumgarten syndrome, the patient has prominent abdominal wall veins and a humming sound near the belly button due to increased blood flow. There may also be an arterial systolic murmur, often associated with liver cancer or alcoholic hepatitis.
An enlarged spleen or splenomegaly is commonly found in patients with portal hypertension. In fact, if the spleen is not enlarged, doctors may question the diagnosis of portal hypertension. However, while a rigid liver often indicates cirrhosis, an enlarged liver doesn’t necessarily correlate with the severity of the portal hypertension.
Testing for Portal Hypertension
The process of diagnosing potential liver diseases involves getting detailed patient history and conducting specific lab tests. A complete blood count can highlight clues such as thrombocytopenia (low platelet count), which tends to be a result of an enlarged spleen, and anemia that might be due to blood loss through the digestive system. A comprehensive metabolic panel can spot kidney failure as well as disturbed liver functions. It can detect viral hepatitis, liver diseases, or low protein levels in your blood (hypoalbuminemia).
To understand how well your liver is creating proteins that help your blood to clot, a coagulation profile test may be performed. Combined with a low protein blood level, a longer prothrombin time might suggest an issue with the liver’s ability to function. Additionally, Doppler ultrasound tests of the portal vein can disclose any potential narrowing (stenosis) or clots (thrombosis) in the blood vessels.
The ultrasound can also show the direction of the blood flow in the liver. A healthy liver would typically have blood flowing towards it, while the direction of blood flow could vary in case of portal hypertension. An abdominal ultrasound can show signs of liver damage (cirrhosis), fluid build-up in the abdominal cavity (ascites), and an enlarged spleen (splenomegaly).
An endoscopy procedure can be performed to examine the digestive tract for swollen veins (varices). If there’s fluid build-up in the abdomen, a procedure called paracentesis may be needed to find out the cause and rule out any bacterial infection.
In cases where signs of portal hypertension are clearly seen through tests and symptoms, there might not be a need to measure portal pressure. The open or closed state of the portal and liver veins can be assessed via duplex Doppler ultrasound, magnetic resonance, or CT angiography. Direct methods to measure portal pressure can be invasive, expensive, and complex. Thus, indirect methods are preferred. These might involve inserting a tube into a liver vein and taking a pressure reading. Another indirect technique involves blocking a liver vein and measuring the pressure.
Treatment Options for Portal Hypertension
The treatment for portal hypertension, which is high blood pressure in the portal vein that carries blood from the intestines and spleen to the liver, largely depends on its underlying cause. If the cause is reversible, such as a blood clot in the portal vein or the main vein in the body due to a condition where your blood clots more easily than normal, the first line of treatment would be to manage this condition which often involves the use of blood thinners.
The treatment may change based on any accompanying health complications. If a patient suffering from this condition also has liver cirrhosis, a disease caused by long-term damage to the liver, they should undergo a medical procedure called endoscopy to check for varices, which are enlarged veins. If they have large varices or those at high risk of bleeding, they should start treatment with either non-selective beta-blockers, which are medications used to lower blood pressure, or a procedure where enlarged veins are tied off.
In case of an sudden bleed from their varices, a minor surgery or the placement of a bypass within the liver is necessary. The patient should also start taking antibiotics to prevent the risk of bacterial infection in the abdomen.
If the patient has ascites, which means they have fluid buildup in the abdomen, treatment might include eating a low-sodium or salt diet, taking water pills, having the fluids drained, the bypass within the liver placement, or even a liver transplant – all of which depends on the severity of the patient’s liver disease and their response to other treatments.
In the end, the most thorough treatment for portal hypertension resulting from cirrhosis is a liver transplant, which means the damaged liver is replaced with a healthy one from a donor.
What else can Portal Hypertension be?
- Budd-Chiari syndrome (a rare condition affecting the liver’s blood flow)
- Cirrhosis (scarring of the liver)
- Constrictive pericarditis (inflammation and thickening of the heart’s outer lining)
- Myeloproliferative disease (increase in certain blood cells)
- Polycystic kidney disease (cysts in the kidneys)
- Sarcoidosis (inflammation that produces tiny lumps of cells in various organs)
- Tricuspid regurgitation (a heart valve condition where the tricuspid valve doesn’t close tightly)
- Tuberculosis (an infectious disease that primarily affects the lungs)
- Vitamin A deficiency (lack of sufficient Vitamin A in the body)
- Wilson disease (a rare genetic disorder causing copper to accumulate in the body)
What to expect with Portal Hypertension
The outlook for a patient largely depends on what is causing their portal hypertension.
Possible Complications When Diagnosed with Portal Hypertension
Complications of a medical condition called portal hypertension, which is high blood pressure in the portal veins of your liver, can include:
- A decrease in platelets due to liver congestion, also known as thrombocytopenia
- Formation of branches of blood vessels on the abdominal wall
- Bleeding from varices, abnormal and enlarged veins in the esophagus, rectum, or other areas
- Acute bleeding or iron deficiency anemia due to chronic blood loss from an unhealthy stomach or intestines, or blood clotting disorder related to portal hypertension
- Ascites, or fluid buildup in the abdomen
- Spontaneous bacterial peritonitis, a serious infection of the fluid in the abdomen
- Hepatic hydrothorax, or fluid in the lungs related to liver disease
- Hepatorenal syndrome, a serious condition affecting your liver and kidneys
- Hepatic encephalopathy, a brain disorder caused by liver disease
- Hepatopulmonary syndrome, a lung disorder caused by liver disease
- Portopulmonary hypertension, a form of high blood pressure affecting the lungs and heart
- Cirrhotic cardiomyopathy, a heart disorder caused by liver disease
Preventing Portal Hypertension
Patients should be taught about the harmful effects of alcohol, which is a frequent cause of cirrhosis, a disease causing scarring and poor function of the liver. Doctors should also explain the possible complications from portal hypertension, a condition where there’s high blood pressure in the liver’s blood vessels. The more patients know, the more likely they are to get medical help sooner, leading to less sickness and lower chances of death.