What is Glomus Jugulare?
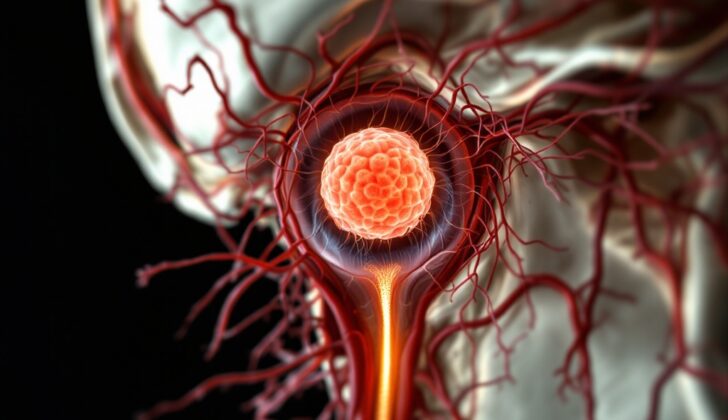
A glomus jugulare is a rare and slowly developing tumor that is part of a group called paragangliomas. These are found in the head and neck region and typically begin within a part of the skull called the jugular foramen. More explicitly, they’re found in a small hollow area within the temporal bone at the base of the skull, known as the jugular fossa. Paragangliomas are generally not cancerous and they come from cells related to the nervous system, known as paraganglia.
Sometimes, these tumors are also referred to as chemodectomas. They’re not very common, with only about 1 to 3 occurrences for every 100,000 people. There are two kinds of paragangliomas, sympathetic and parasympathetic, and most of the ones in the head and neck, including the glomus jugulare tumors, are of the parasympathetic type.
Paragangliomas can occur at a variety of sites in the head and neck. They could be close to the split in the main artery of the neck (a carotid body tumor), close to a group of nerves located in the chest and abdomen known as the superior vagal ganglion (a glomus jugulare tumor), at a branch of a nerve in the ear (glomus tympanicum tumor), or at the inferior vagal ganglion (glomus vagale tumor). Glomus tumors, while generally slow-growing, may lead to serious complications if they become sizable. This growth can cause pressure, and even damage to the surrounding body structures.
Managing a glomus jugulare can be challenging because they tend to have a lot of blood vessels, have a difficult to reach location, and are often at an advanced stage when diagnosed.
What Causes Glomus Jugulare?
Glomus jugulare tumors are typically noncancerous tumors that develop from specific cells, known as paraganglia cells, in the wall of the jugular bulb, located within the jugular foramen (the area where the jugular vein exits the skull). These tumors grow slowly and are usually not harmful. However, because of their location near the temporal bone in the skull, as they grow, they can cause pressure and potentially erode the bone.
Interestingly, only 1% to 5% of these tumors are cancerous. The majority of these tumors – around 80% – occur randomly with no known cause (these are called sporadic), while the rest are inherited or passed down from family members (hereditary). Those with the inherited form often start noticing symptoms at a younger age and can have tumors on both sides. However, the good news is inherited forms are less likely to be cancerous compared to the sporadic ones.
Risk Factors and Frequency for Glomus Jugulare
Glomus jugulare tumors are a rare type of tumor, with approximately one case occurring yearly for every 1.3 million people. The typical age of diagnosis is 56 years, and it’s more commonly seen in women by a factor of 3 to 6.
- Amongst all paragangliomas (a type of tumor) found in the head and neck:
- About 44% to 48% are carotid body tumors.
- 16% to 24% are glomus jugulare tumors.
- 20% are glomus tympanicum tumors.
- 8% are glomus vagale tumors.
Signs and Symptoms of Glomus Jugulare
Patients with this condition often come with symptoms like hearing loss, pulsatile tinnitus (a type of ringing in the ear), and lower cranial nerve neuropathy, which is nerve damage in the lower cranial region. Roughly 75% of patients display these symptoms. Another symptom that is seen in about 10% of cases are deficits in the lower cranial nerve. This results in neurological violations, causing facial paralysis, difficulty in swallowing, hoarseness, weakened shoulders, and tongue deviation. Some other symptoms can include earache, ear discharge, and bleeding from the ear.
- Hearing loss
- Pulsatile tinnitus (ringing in the ear)
- Lower cranial nerve neuropathy (nerve damage)
- In 10% of cases:
- Facial paralysis
- Difficulty swallowing
- Hoarseness
- Weakness in the shoulder
- Tongue deviation
- Earache
- Ear discharge
- Ear bleeding
Testing for Glomus Jugulare
During an otoscopic examination, a doctor might discover a pulsating red growth in the middle ear. This mass is often spotted behind an ear drum that is still intact. The ear drum itself might demonstrate increased blood flow and feature a red growth at its base, creating a visual effect similar to a rising sun. Sometimes, the tumor might break into the ear canal and cause bleeding from the ear.
Audiologic tests, like pure tone and speech audiometry, are typically done as well. These tests are performed to check the hearing capabilities of a person.
Scanning the head using a computed tomographic (CT) scan with finely detailed images can show destruction in the bone. The bone erosion that is sometimes seen is often referred to a “moth-eaten” appearance.
A magnetic resonance imaging scan (MRI), specifically done with an intravenous contrast-enhancement process, can help your doctor see an enhanced image of a potentially spreading lesion from the jugular bulb to the middle ear. Tumors extending to the posterior fossa and the neck area are common if left untreated. The MRI shows the tumor’s blood vessels, its progress along neural foramina, multicentricity, and should be the first imaging considered when evaluating a patient who may have a glomus jugulare tumor. On images that are T1-weighted, paragangliomas can look less intense with a spotted appearance; however, with the addition of a gadolinium-enhanced contrast, the image shows much-enhanced details due to increased blood flow in the glomus jugulare area.
Angiography is a procedure that can help differentiate paragangliomas from other issues as well as highlight the blood flow and the blood vessels feeding the tumor, which can then be blocked or embolized. The main artery providing blood to the tumor is typically the ascending pharyngeal artery, although the occipital artery can also contribute. However, branches of the internal carotid artery and the vertebrobasilar system have, at times, also been known to be involved, such as the caroticotympanic artery and the posterior inferior cerebellar artery. Balloon test occlusion studies can be performed to give doctors an understanding of whether the closure of the petrous internal carotid artery would be manageable.
When it comes to classifying these tumors, the most commonly used standards are those provided by Fisch and Glasscock-Jackson, which classify tumors based on their location and spread.
Treatment Options for Glomus Jugulare
When a patient is diagnosed with a type of tumor known as glomus jugulare, observation can often serve as a great alternative to immediate treatment. Research has shown that almost two-thirds of these tumors remain stable and might even reduce in size. However, around 40% of these tumors grow at a slow but steady rate, so it’s crucial to have regular brain scans (MRIs) to observe any changes in the tumor’s behavior and progression.
There are various treatment options for glomus tumors, each with their pros and cons, making the choice of treatment quite challenging. Conventionally, these tumors have been handled via surgical removal or radiation therapy, or sometimes both combined. However, these options can have significant side effects. As an alternative, a method called stereotactic radiosurgery (SRS) has grown in popularity. SRS is a type of radiation therapy that focuses high-power energy on a small area of the body. Reviews of the medical literature reveal that radiation therapies like EBRT and SRS can be just as effective as surgery for treating jugular paragangliomas, another name for glomus tumors.
The best course of action usually depends on individual patients. For young, healthy patients experiencing issues with their cranial nerves (nerves in the brain), surgical removal is often recommended. Sometimes, a procedure to cut off the blood supply to the tumor is performed a few days before surgery (known as embolization). In most cases, the surgery successfully removes the whole tumor. However, it can sometimes result in neurology-related side effects, and new injuries to the cranial nerves can occur in about 60% of patients. Therefore, surgeons often opt for a less aggressive approach, removing most – but not all – of the tumor to limit side effects and improve symptoms.
After surgery, radiation therapy is often used to treat any remaining parts of the tumor. This combination tends to lead to better results and lower the risk of serious side effects. Another approach involves using an instrument called an endoscope, which allows for smaller incisions and a more tailored surgical plan. This is usually reserved for tumors that have spread to the back part of the brain (posterior fossa). Over time, technological advancements have made nerve monitoring techniques available, which can help prevent nerve damage during surgery.
Radiation therapy can also be used when patients have glomus jugulare tumors on both sides of their neck or after the partial removal of large tumors. This treatment option can be administered over multiple sessions (standard fractionated radiotherapy), or in a single session (radiosurgery). Radiosurgery has the advantage of being able to precisely target the tumor while preserving the surrounding healthy tissue. This method can be beneficial for surgical high-risk patients or when the tumor is present on both sides. Research shows it can control the tumor in 92% of patients and control symptoms 93% of the time. However, it does have a minor risk of complications.
While the complete elimination of glomus jugulare tumors using embolization alone is exceptionally challenging, this technique can be useful in certain situations. Its use mainly comes in alleviating symptoms in patients with tumors that cannot be removed by surgery. However, embolization as a stand-alone treatment is generally considered to provide only temporary relief. Sometimes, a type of embolization using a substance called Onyx can be employed to manage bleeding in the ear associated with inoperable tumors. Additionally, when used before the surgery, embolization can also shorten the duration of the operation and reduce blood loss during the procedure.
What else can Glomus Jugulare be?
When it comes to certain health conditions, there are several potential causes that doctors may consider. In this case, they might investigate the following possibilities:
- Schwannoma of lower cranial nerves
- Neuroma of lower cranial nerves
- Glomus tympanicum
- Neck and head metastasis
- Bone metastasis
- Lymph node metastasis
- Meningioma
- Cholesteatoma
- Endolymphatic sac tumors
- Chordoma
- Chondrosarcoma
- Epidermoid
- Chronic mastoiditis
- Hemangiopericytoma
- Plasmacytoma
- Dural arteriovenous fistula
- Arteriovenous malformations
- High riding jugular bulb
- Asymmetry of jugular foramen size
- Tortuous internal carotid artery
- Idiopathic intracranial hypertension
What to expect with Glomus Jugulare
Recent studies show that the rate of stroke from surgery can range from 0% to 3.5%. Cranial nerve injuries, which can affect any of the 12 nerves that control our senses and movements, occur in between 5% to 39% of patients. The overall death rate from these surgeries is somewhere between 0% and 2.7%. Unfortunately, 15% of patients are unable to go back to their normal daily activities after the surgery.
With a treatment called stereotactic radiosurgery, 60% of patients showed improvement in their previous neurological problems. This type of treatment was successful in controlling the tumor in 91% of patients. The Kaplan-Meier method, which is a way to estimate how well this treatment works in the long term, shows that it works well for controlling tumors in 92.2% of cases after five years and works in 86.3% of cases after ten years.
While hearing tends to get worse after radiosurgery, symptoms like balance problems, dizziness, and tinnitus (ringing in the ears) usually improve after the treatment.
Possible Complications When Diagnosed with Glomus Jugulare
Some common side-effects or conditions that may occur are:
- Blockage of a vein in the brain (Sigmoid sinus thrombosis)
- Nerve damage in the brain (Cranial neuropathies)
- Rhythmic sound in the ears (Pulsatile tinnitus)
- Worsening of hearing ability (Deterioration of hearing)
- Inability to move the vocal cord (Vocal cord paralysis)
- Inhaling food or drink into the lungs (Aspiration)
- Inability to move the face muscles (Facial paralysis)
- Loss of hearing caused by problems with the ear canal or eardrum (Conductive hearing loss)
- Leakage of brain fluid (Cerebrospinal fluid leak)
- Dysfunction of specific nerves in the lower part of the brain (Lower cranial neuropathy)
- Dead tissue in the skull bone near the ear due to radiation treatment (Temporal bone osteoradionecrosis)
- Brain tissue damage caused by radiation (Brain radionecrosis)
Preventing Glomus Jugulare
Glomus jugulare tumors are a type of growth that develops slowly over time. Therefore, maintaining regular check-ups and monitoring over the long term is important. The care team for these situations will include professionals from various medical fields – your primary care doctor, specialists in brain surgery (neurosurgeons), ear, nose, and throat specialists (otolaryngologists), and experts in using imaging techniques to diagnose conditions in the nervous system (neuroradiologists). There will also be involvement from other healthcare providers who specialize in physical medicine, rehabilitation, and managing any complications that can arise.
Patient education is crucial, especially for those individuals who have a family history of this disease. This is because these individuals could potentially be at a higher risk of the disease. Early screening can be beneficial in these cases, as it allows doctors to detect and treat multiple occurrences of the disease at once. This early intervention can lead to better patient outcomes and a reduced risk of other health problems associated with this condition.