What is Pyogenic Granuloma?
Pyogenic granuloma (PG), also known as granuloma pyogenicum, is a common, harmless type of skin tumor, often found on the skin and mucous membranes (areas that produce mucus, like inside your nose). These growths are also scientifically known as lobular capillary hemangiomas. In the past, they were mistakenly thought to be a severe reaction to infections, leading to their name ‘pyogenic granuloma’. However, this name can be misleading.
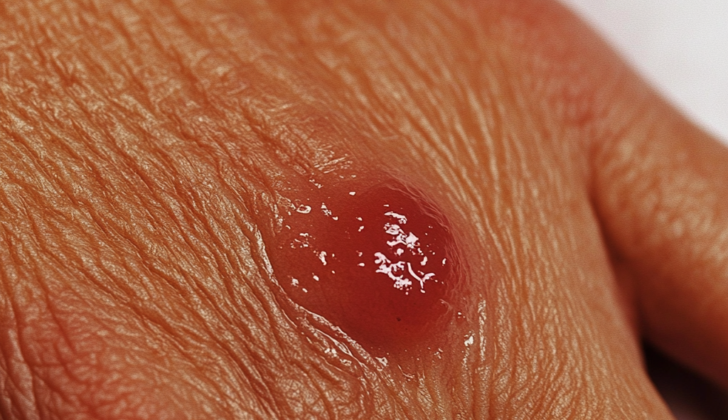
The growth itself usually appears as a single, red, raised spot that is easily damaged. Sometimes, it may appear as a flat plaque. The growth advances quickly, often causing its surface to break down or ulcerate. It’s usually seen on skin or mucous surfaces. Within these surfaces, it’s most commonly found inside the mouth. At times, it can also occur elsewhere within the gastrointestinal tract (digestive system).
Interestingly, when these growths develop in the mouth during pregnancy, particularly on the gums, they are known as granuloma gravidarum, granuloma of pregnancy, or epulis gravidarum. This usually happens in the second or third trimester of pregnancy. There have been rare cases where patients had many of these growths, especially while taking oral contraceptive pills, or after a kidney transplant.
What Causes Pyogenic Granuloma?
The exact cause of certain health conditions is not entirely known. However, it is believed that an imbalance in the body’s natural growth and control signals can lead to the rapid growth of tiny blood vessels, forming fragile, bubble-like structures. Sometimes this growth in the blood vessels could happen because of minor injury, but injury is found to be a cause in only up to 7% of cases. Other possible factors could include infections and pre-existing issues with the blood vessels.
Hormones, including those related to pregnancy, may play a role in these lesions, particularly in women during their childbearing years. However, this theory is questioned as there aren’t as many lesions found in the vaginal area as would be expected and slightly more skin lesions are found in men. It’s suggested that hormones may exaggerate inflammatory reactions in the gums during pregnancy. Further research is needed. Certain forms of this kind of lesion seem to be linked with medication use. This is most seen around the nails with medication linked up to 30% of the time and is also associated with chronic skin conditions such as eczema and psoriasis.
Medicines that are often associated with causing these lesions might include:
- Retinoids (used for skin issues)
- Antiretrovirals (used for HIV)
- Antineoplastics (used for cancer)
- Growth factor inhibitors (used for forms of cancer)
- Tyrosine kinase inhibitor (used for certain cancers)
- Mammalian target of rapamycin (mTOR) inhibitors (used in organ transplants)
- Immunosuppressive agents (used for certain rheumatoid disorders)
Disseminated pyogenic granulomas, a rare entity, have been reported to occur with isotretinoin use (a medication used for severe acne) and in patients with weakened immune systems. Conditions that affect the mouth are seen in patients on certain medications after a stem cell transplant. Several case reports support this, especially with patients treated for either acute or chronic graft versus host disease with certain medications.
These growths can occur spontaneously or following laser treatment or cryotherapy to a preexisting vascular malformation, such as a birthmark or arteriovenous malformation (an abnormal connection between arteries and veins).
Risk Factors and Frequency for Pyogenic Granuloma
Pyogenic granuloma can occur in people of all ages, but its distribution can vary. Some studies show it being more common in males, and typically showing up in the second decade of life. However, mucosal lesions were observed to be more common in females, usually presenting later in life, around their forties.
- Pyogenic granuloma can happen in people of all ages.
- Some studies suggest it’s slightly more common in males.
- Typically, the condition appears in the second decade (10-20 years) of life.
- Mucosal lesions, a variant of pyogenic granuloma, are usually found more in females.
- Women tend to get these lesions later in life, generally in their forties.
- When both skin and mucosal versions are considered, males generally display symptoms earlier than women, usually from childhood to late twenties.
- However, mucosal pyogenic granuloma can happen at any time in men, while in women, most cases occur before the age of forty.
- A study on children showed the average age at diagnosis was 6 to 10 years and the condition was more common in boys.

tumor that arises in tissues such as the skin and mucous membranes.
Signs and Symptoms of Pyogenic Granuloma
A lobular capillary hemangioma, also known as a pyogenic granuloma, is a type of skin growth. It usually starts as a small, red bump and grows over weeks or months, eventually stabilizing in size. The color can range from red to reddish-brown or purple. Sizes can vary widely, with small lesions being just a few millimeters in diameter, while larger ones can be several centimetres across.
These growths are typically solitary, but additional ones may develop near the original lesion. In some cases, individual growths may spread across the body. Mature lesions often have a distinctive ‘collarette’ of scale at the base. Although this can help with identifying the growth, it is not unique to this condition and can be seen with other skin conditions. These hemangiomas are often sensitive and can bleed profusely with even minor trauma. This often leads to patients covering the lesion with a band-aid to prevent further bleeding – referred to as the “band-aid sign.”
A lobular capillary hemangioma can occur anywhere on the skin or mucosal sites. Some preferential sites include the trunk and extremities in adults and the head and neck region in children. For mucosal PG, common locations include lips and gums.
There are several variants of lobular capillary hemangioma, including:
- Digital or periungual pyogenic granulomas, which may be solitary or multiple
- Satellite pyogenic granulomas that appear around the initial area
- Disseminated pyogenic granulomas, although rare, can occur after trauma, or due to certain medications
- Intraoral pyogenic granuloma, which often appears in immunosuppressed patients, especially after a stem cell transplant
Uncommonly, lobular capillary hemangiomas can be found below the skin surface or inside blood vessels. They can also appear in the gastrointestinal tract, possibly causing overt or chronic bleeding, leading to anemia.
Testing for Pyogenic Granuloma
A lobular capillary hemangioma is a type of skin growth that doctors often identify based on your medical history and certain obvious features of the growth. They’ll ask if you’ve had any injuries, if you’re pregnant or have been recently, and what medications you’re taking. Sometimes, a special skin examination with a tool called a dermoscope can be helpful.
The growth usually looks pink or red and appears solid under the skin, with a flaky, white border. Sometimes, there may be white lines through the middle of the growth, something that’s caused by fibrous tissue.
If your doctor isn’t sure after looking at the growth and talking to you, they might decide to get a sample of tissue from the growth for further testing. This is often done if there’s any uncertainty about what the growth is. There are also instances where the doctor may choose to remove the growth not just for diagnosis, but also to ease the patient’s worry. Regardless of why the growth is removed, it’s really important that the tissue is sent off for further testing to make absolutely sure it’s not something more serious.
Treatment Options for Pyogenic Granuloma
Lobular capillary hemangiomas are small, benign blood vessel tumors that often cause ulceration and bleeding. These are the usual reasons why treatment is necessary. Because there is limited research available, there isn’t a universally agreed-upon treatment plan for these lesions. The success and recurrence rates can also vary depending upon the treatment chosen. It’s important for the patient to understand that the lesion could come back even after treatment. If the lesion is not visible, the best practice is to fully remove it using local anesthesia. This method also yields the lowest chance of the lesion reappearing, and provides a good specimen for laboratory examination.
For lesions that are attached to the skin surface (sessile) or have come back after treatment, surgical removal with stitches is typically the preferred treatment as it reduces postoperative bleeding and lowers the chance of the lesion reappearing. Other treatment options, used particularly in cosmetic areas, include shave excision or scraping off (curettage) followed by electrocautery, which uses electricity to seal off the blood vessels, but the chance of recurrence is higher with these methods.
Alternatively, there are several non-surgical treatments such as freezing (cryotherapy), electrocautery, or chemical cautery with silver nitrate without any removal. Laser therapy like pulsed dye laser (PDL), CO2 lasers, or long-pulsed 1,064-nm Nd:YAG laser could also be used alone or with surgical methods. If the lesions are in cosmetically sensitive areas or in children, treatments like pulsed dye laser, CO2 laser removal, or electrocautery could be considered if laser therapies are not available.
Generally, managing these lesions with medication is not recommended. A variety of creams or treatments injected directly into the lesion have seen variable results. These include topical imiquimod cream, alitretinoin gel, timolol, propranolol, and even phenols for lesions near the nails. There are also injections with corticosteroids and other agents that cause the blood vessels to shrink, like ethanolamine oleate, sodium tetradecyl sulfate, polidocanol, and bleomycin, which have seen intermittent patient benefits.
In situations where the lesions are caused by pregnancy or medications, the chance of the lesion returning after treatment is higher. If possible, stop taking the medication that’s causing the lesion. If the medicine can’t be stopped, such as in the case of those used to treat cancer, the management focuses on relieving symptoms. For example, specific guidelines for preventing and treating lobular capillary hemangiomas related to cancer treatment medications have been published, recommending weekly chemical cauterization, electrodesiccation (drying out tissue with electricity), or nail removal.
What else can Pyogenic Granuloma be?
When diagnosing lobular capillary hemangioma, which is a specific kind of skin issue, doctors will look at a patient’s medical history and examine the affected area. However, they also must consider the possibility of other serious conditions. Some of these might include:
- Amelanotic melanoma
- Squamous cell carcinoma
- Basal cell carcinoma
- Angiosarcoma
In people with lowered immune systems, Bacillary angiomatosis or Kaposi sarcoma may also be possible diagnoses.
Doctors also have to distinguish the condition from benign (or harmless) skin issues, including:
- Hemangiomas
- Irritated melanocytic nevi
- Spitz nevus
- Warts
- An acquired digital fibrokeratoma
- Granulation tissue resulting from minor injury or scratching
- Glomus tumor
- Angiolymphoid hyperplasia with eosinophilia
Upon further investigating the tissue under a microscope, other diagnoses may consider are variations of capillary hemangiomas or infections such as acquired tufted angioma, glomeruloid hemangioma, bacillary epithelioid angiomatosis, and verruga peruana.
What to expect with Pyogenic Granuloma
These growths are not cancerous and won’t turn into cancer. However, they don’t vanish on their own and can cause bleeding, can turn into open sores (ulcerate), or may change the way a person looks, which can be undesirable. For these reasons, treatment may be required. For pregnant women with these types of growths in the mouth, the growths often disappear after the baby is born.
In some cases, part of the growth is removed through shave excision (surgically shaving off the growth) or curettage (scraping the growth off). However, this may lead to future regrowth; that’s why complete removal at the outset is often preferred. If the growth does return, a complete surgical removal is typically needed.
Possible Complications When Diagnosed with Pyogenic Granuloma
Lobular capillary hemangioma, a type of skin growth, can lead to several potential issues. These include:
- Ulceration, which is the development of open sores on the skin
- Bleeding if the growth is injured
- Possible infections caused by the growth
- Potential distress to the patient due to changes in appearance,
especially if the growth is on the face
Preventing Pyogenic Granuloma
People with this condition often need to be reassured because they might be fearful of serious health problems. It’s important for them to avoid scratching or picking at the affected area. Doing so could make things worse or lead to an additional infection. They should also be aware that there’s a chance the condition could come back if it’s not completely removed, and there is a risk of scarring if the whole area is surgically removed. The choice of how to treat the condition should be a joint decision made by the patient and their doctor.