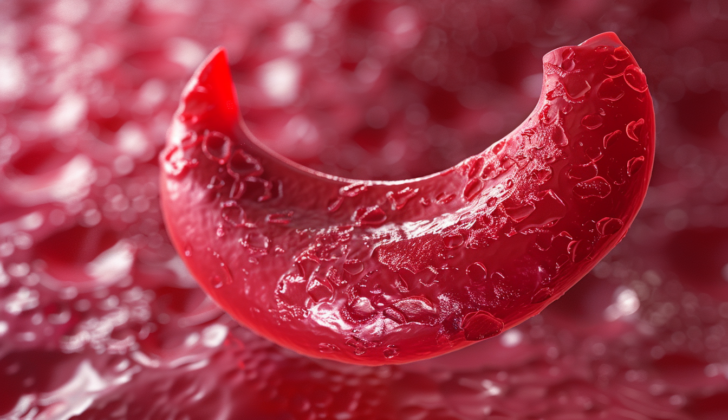
What is Sickle Cell Crisis?
Sickle cell disease (SCD) is a type of inherited condition that impacts the red blood cells. It is found in roughly 1 in 500 African American children and 1 in 36,000 Hispanic American children. SCD leads to a condition known as anemia as well as an episode known as a “sickle cell crisis” (SCC).
The most common symptom of sickle cell disease is an “acute painful crisis,” which often necessitates a hospital stay. A “sickle cell crisis” can refer to several severe conditions like the acute painful crisis, aplastic crisis, and various types of crises related to the spleen, liver, and blood cells, among others. Some of the other urgent complications include pneumonia, meningitis, sepsis, bone infections, stroke, bone tissue death, prolonged painful erection, and blood clots.
In a sickle cell crisis, the main symptoms are intense, sudden pain and problems with organ function. The symptoms can vary depending on what part of the body is affected. For example, a vaso-occlusive crisis, experienced by most patients with SCD by the age of 6 years, can cause intense pain and swelling in the hands and feet, particularly in young children. Pain can start in any part of the body but often impacts the arms, legs, back, and chest. SCD is identified via a lab test that detects abnormal hemoglobin S (HbS), a type of protein in red blood cells, with genetic testing also used to confirm the diagnosis. Treatment for SCD primarily involves managing symptoms and related complications.
Roughly a third of deaths related to sickle cell disease happen at home or within 24 hours of being admitted to a hospital. Typically, adults are more prone to pass away from long-term complications, while children’s deaths tend to be sudden. The top causes of death in sickle cell disease are vaso-occlusive crises, threats to the heart and lungs, infections, and kidney issues. Low oxygen levels in the blood can further exacerbate these problems.
What Causes Sickle Cell Crisis?
Sickle cell disease is a genetic disorder caused by a mutation or change in a specific gene. This gene mutation happens on chromosome 11, where a type of protein in red blood cells called glutamic acid is replaced with another one called valine at a certain location on the β-globin subunit. This replacement results in alterations to the physical characteristics of the globin chain.
Lots of things can trigger this change in the physical properties of the red blood cells. It could be a decrease in oxygen levels in the body (hypoxia), dehydration, exposure to cold or changes in weather, stress, and infections.
Risk Factors and Frequency for Sickle Cell Crisis
Sickle cell disease is a global health issue, impacting around 3 million people worldwide and 100,000 people in the US alone. Those living with this disease have a median life expectancy of 43 years. The disease is most common in places such as sub-Saharan Africa, South Asia, the Middle East, and the Mediterranean. The most prevalent type of this disease is characterized by a genetic feature known as homozygous hemoglobin SS (HbSS).
- Sickle cell disease affects roughly 3 million people globally and about 100,000 in the US.
- The median life span for people with this disease is 43 years.
- This disease is most common among those living in sub-Saharan Africa, South Asia, the Middle East, and the Mediterranean.
- The most commonly observed genetic form of this disease is homozygous hemoglobin SS (HbSS).
Signs and Symptoms of Sickle Cell Crisis
People with vaso-occlusive crisis (VOC), often linked with Sickle Cell Disease (SCD), typically experience moderate to severe pain, fever, and in younger children, swelling of the hands and feet. This pain can develop anywhere in the body, often noticeable in the arms, legs, back, and chest.
Another condition related to SCD is the splenic sequestration crisis. This condition causes the spleen to trap red blood cells, leading to a falling hemoglobin level and issues like abdominal pain, rapid heart rate, low blood pressure, and tiredness. If left untreated, it can result in severe conditions like multiple organ failure and can be life-threatening.
Aplastic crisis is another condition commonly seen in SCD patients. It manifests as a sudden weakness and paleness due to rapidly dropping hemoglobin levels. The main trigger for this condition is often the parvovirus B19.
Acute chest syndrome is a serious complication of SCD. It leads to symptoms like cough, fast breathing, chest pain, low oxygen in the blood, and in severe cases, respiratory failure.
Hemolytic crisis, characterized by a sudden fall in hemoglobin levels, is another complication seen in patients with SCD.
Osteonecrosis, or bone infarction, can occur in up to 50% of SCD patients. It usually affects the long bones of the body, resulting in joint pain and disability.
- Acute chest syndrome
- Aplastic crisis
- Hemolytic crisis
- Osteonecrosis
Priapism, or prolonged painful erection, is a condition that can occur in SCD. This condition can lead to pain, psychological stress, and sexual dysfunction.
Many young people with SCD have an increased renal plasma flow and glomerular filtration. However, this decreases with age leading to renal complications, including an end-stage renal disease.
Cerebrovascular accidents or strokes also occur in patients with SCD. They can lead to serious health issues, including physical and sensory deficits like pain and seizures, and cognitive defects.
Girdle syndrome is a rare condition in which vaso-occlusion occurs in the lungs, liver, and mesentery, causing a characteristic girdle-like pain.
Testing for Sickle Cell Crisis
To diagnose Sickle Cell Disease (SCD), primary methods include laboratory tests that detect unusual HbS (hemoglobin S) in the blood. This is often further confirmed by genetic testing. For patients experiencing a sickle cell crisis, more detailed evaluations are typically required. These evaluations usually consist of a complete blood count, a detailed check of young red blood cells (reticulocyte count), a full metabolic panel, and liver function tests. Doctors will also perform a comprehensive examination of the patient’s overall health.
Some scenarios may require imaging studies, such as ultrasound, magnetic resonance imaging (MRI), or Doppler scans. These scans help assess any potential complications arising from the crisis. If there is a possibility of the patient needing a blood transfusion, blood type and match screenings would also be conducted.
In case of fever, doctors might recommend tests for inflammatory markers like CRP and procalcitonin as well as broad cultures to identify the source of the potential infection.
It’s also important to screen for conditions like Acute Chest Syndrome (ACS), and doctors often use chest x-rays for early identification. An abdominal ultrasound might be conducted if there are concerns about gallstones. A test for blood gas levels (ABG) could be obtained if there is a risk of low oxygen levels and respiratory failure. In case of suspected stroke, brain scans using CT or MRI technology would be recommended.
Treatment Options for Sickle Cell Crisis
The main strategy for managing sickle cell disease (SCD) involves handling the symptoms and related complications. Newer therapies that could potentially cure the disease, like stem cell transplant and gene editing, are complex and expensive. This means they may not be available in countries dealing with high numbers of SCD cases due to limitations in their healthcare systems.
Vaso-Occlusive Crisis, a common complication of SCD, requires early diagnosis, prevention of complications, and management of damage to organs. Treatment should start by quickly assessing pain and commencing painkillers as soon as possible. Painkillers can be delivered intravenously (directly into a vein), intranasally (through the nose), or orally depending on the severity of the pain. The type, method, and dose of the painkiller should be tailored to the individual patient.
Throughout treatment, it is important to monitor the patient’s vital signs, including oxygen levels, and regularly reassess their pain. If their pain can be effectively managed, they may be discharged with a healthcare plan and oral painkillers for home use. If not, they may need to be admitted to the hospital for more potent painkillers or a blood transfusion.
Patients should be sufficiently hydrated, as dehydration is a risk factor for vaso-occlusive disease. In addition, recognizing and treating other possible causes of pain is critical. For conditions like acute chest syndrome or spleen crises, supportive care like oxygen, careful fluid administration, and blood transfusions are needed. In such cases, antibiotics and additional painkillers may also be required.
Hydrea, a chemotherapy agent, is widely used in treating SCD. It works by reducing the rate of acute chest syndrome, pain, and other complications, thereby improving the patient’s quality of life and reducing the need for hospitalization and blood transfusions. Medications like glutamine and vaxelotor are utilized to protect red blood cells and interrupt the vaso-occlusive process, while crizanlizumab is given by monthly infusion to block the adhesion of certain cells contributing to the vaso-occlusive process.
Bone marrow transplant restores the ability to produce healthy red blood cells and has been shown to potentially cure SCD. Gene therapy is another emerging treatment option, where functional genes are added to a patient’s stem cells, which are then returned to the patient. This enables the patient to produce healthy red blood cells and significantly reduces complications.
Long-term management of SCD focuses on preventing infections and damage to organs. In addition to lifelong penicillin therapy, vaccinations against certain infections are also administered. Additionally, supplements like folate are given to prevent deficiencies. COVID-19 and flu vaccinations are also recommended.
What else can Sickle Cell Crisis be?
People with a vaso-occlusive crisis often experience severe pain, but may not show clear signs of illness. What this means is, when a person with this condition is in pain, it’s important not to automatically attribute the discomfort to sickle cell disease. Instead, healthcare providers need to evaluate other conditions that could be causing the pain.
Take for example someone with a vaso-occlusive crisis who feels pain in the stomach area. This could mimic what doctors call an “acute abdomen,” a sudden, severe belly pain that requires immediate medical attention. Therefore, other health problems that also cause sudden stomach pain should be considered. These conditions can include:
- Appendicitis, which is inflammation of the appendix
- Pancreatitis, an inflammation of the pancreas
- Pyelonephritis, a kind of kidney infection
- Pelvic inflammatory disease, an infection of the female reproductive system
- Hepatobiliary disease, relating to the liver, gallbladder, or bile ducts
Furthermore, if persistent pain is felt in a specific bone, conditions like avascular necrosis (where bone tissue dies due to lack of blood supply) or acute osteomyelitis (a bone infection) should be considered. These conditions require careful differential diagnosis to ensure that the right treatment is pursued.
What to expect with Sickle Cell Crisis
Various factors may indicate a higher risk of multiple organ failure during a chest crisis. These include low blood platelet count, anemia, a higher breathing rate, worsening low oxygen levels in the body, the involvement of multiple lobes of the lung visible on a chest X-ray, and compromise of nerves.
Since infections can cause a chest crisis, it’s recommended to check for them if needed. This could be done through blood and sputum samples or through a process known as nasopharyngeal aspiration, which helps to check for respiratory viruses.
Possible Complications When Diagnosed with Sickle Cell Crisis
People with sickle cell disease often experience side effects from treatments, and sometimes the treatments don’t work effectively. Over time, these issues can add up and cause significant harm. The three most common complications found when the blood vessels get blocked (also known as vaso-occlusive crises) are infections, fever, and lung related problems.
As sickle cell disease progresses, patients’ ability to perform tasks and recover from illness might decrease. Neurological complications may include conditions like silent cerebral ischemia (an interruption in blood flow to the brain), strokes which can either be due to blood clots or bleeding in the brain, Moyamoya syndrome (a rare, progressive cerebrovascular disorder), posterior reversible encephalopathy syndrome (a brain disorder), cerebral fat embolism (the presence of fat particles in the brain), and cerebral venous sinus thrombosis (a blood clot in the brain).
Bacterial infections are a common and serious complication of sickle cell disease. This is because the irregularly shaped red blood cells can lead to a condition called functional asplenia, which makes patients more susceptible to life-threatening infections. Especially dangerous are infections from encapsuled microbes: Streptococcus pneumoniae, Neisseria meningitis, and Haemophilus influenza type b. In some parts of the world, people with sickle cell disease also face additional risks from diseases like hepatitis B, salmonella, and malaria. Poverty and inadequate health care make these problems worse.
There are known treatments for sickle cell disease but their availability is inconsistent. The Acute chest syndrome, a lung-related condition, is the leading cause of death among adults with sickle cell disease. This condition is generally driven by infections, with microbes like mycoplasma pneumonia and the respiratory syncytial virus (RSV) common in children, while chlamydia is more common in adults. Stroke is the primary cause of disability in sickle cell patients. The type of stroke varies; ischemic stroke (caused by blocked blood vessels) primarily affects children, while cerebral hemorrhage (bleeding in the brain) generally affects adults in their 30s and 40s. When a patient has a stroke, it’s critical to start an exchange transfusion protocol immediately. Without this treatment, the risk of a recurrent stroke is high. Transfusions are also required for acute chest syndrome, stroke, aplasia (a condition where the body stops producing new blood cells), and sequestration complications (where large amounts of blood get pooled in the liver or spleen). These transfusions do come with risks, however, including an immune response to the new blood cells, a delayed reaction to the transfusion, increased blood thickness, and iron overload.
Preventing Sickle Cell Crisis
Educating patients about their medical conditions can help avoid the need for hardcore treatment options later on. This is because patients can keep an eye on their condition and report any critical symptoms as soon as they start. Although patients might not have formal medical training, they and their caregivers can still learn what signs to look out for, and how best to respond. For people with sickle cell, their crises can cause ongoing damage. Therefore, the earlier these crises are managed, the better their long-term life quality will be.