What is Spider Veins?
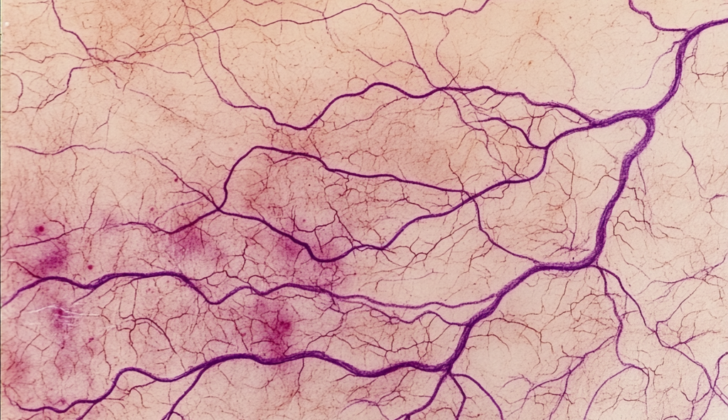
“Spider veins,” also known as telangiectasias, are small damaged blood vessels that show up on the skin’s surface. They look like thin lines, which can be purple, red, or blue. While they’re mostly found on the legs, they can also appear on other body parts, especially the face. The term “telangiectasias” comes from three Greek words — “telos” meaning end, “angeion” meaning vessel, and “ektasis” meaning dilatation. These veins are sometimes referred to by other names such as thread veins, venus flares, sunburst veins, stellate veins, and hyphen webs.
Typically, spider veins don’t lead to serious health issues, but they can occasionally cause pain. They are often considered bothersome from a cosmetic standpoint, which is why most treatments aim to improve the person’s appearance by eliminating these veins. The causes, frequency, risk factors, examination, and treatment options for spider veins will be discussed further.
What Causes Spider Veins?
Spider veins are basically abnormalities in the small blood vessels under the skin. They can come from bigger veins or smaller ones, known as capillaries. Spider veins that come from veins are raised and are usually blue or purple. They often measure between 1mm and 3mm across. On the other hand, the ones that come from capillaries are flat and can be pink or red, with a size of 0.1mm to 1.0mm.
In the legs specifically, they’re usually about 180 micrometers to 1mm deep in the skin and are made up of a main vessel and small, dilated venous offshoots found in the reticular dermis, the layer of skin that lies just beneath the surface layer.
The exact cause of spider veins isn’t entirely clear. Some people think they come from varicose veins and are caused by a similar issue. That issue is having faulty valves, which happens in chronic venous disease, a long-term condition that’s caused by poor blood flow in the veins. On the other hand, one study found that fewer than one in four patients with spider veins had signs of having faulty venous valves.
Another idea, proposed by a man named Goldman, suggests that small vessels known as telangiectasias are caused by low local oxygen levels, which leads to inflammation of the blood vessel lining and the creation of new blood vessels. These spider veins may actually be caused by a combination of factors, ranging from the more minor end of chronic venous insufficiency to the more severe end, which is varicose veins.
In the case of faulty valves in the deep venous network, the blood can flow backwards, which eventually leads to blood accumulating in small vessels close to the skin’s surface. The resulting inflammation and the development of new blood vessels from low local oxygen levels cause the small vessels to enlarge and branch out, creating a spider-like appearance.
Risk Factors and Frequency for Spider Veins
Spider veins are a common condition several studies report most adults will experience at least once in their lifetime. People usually see these for the first time when they are between 30 and 50 years old. In one study done in Scotland, it was found that 88% of women and 79% of men had spider veins on their right leg. Even though 98% of individuals with spider veins had very mild symptoms, when men do get them, it’s often more serious and they are more prone to advanced chronic venous disease.
Spider veins are more likely to be seen in women, especially those who have had more pregnancies. Your chances of getting spider veins also increase if you’re overweight, or if your job requires you to sit or stand for long periods of time. Some other risk factors for spider veins include smoking, having a personal history of venous thromboembolism in one of your limbs, and various genetic factors. Some studies also suggest that the risk is higher for non-Hispanic white people.
- Spider veins are common and most adults will have them at some point.
- They typically start showing up between the ages of 30 and 50.
- In a study done in Scotland, 88% of women and 79% of men were found to have spider veins in their right leg.
- Although men are less affected, their condition is usually more severe.
- Women have a higher risk, especially with increasing pregnancies.
- Being overweight or having a job that involves lots of sitting or standing can also increase your risk.
- Smoking and having a history of venous thromboembolism also increase your risk.
- Genetic factors can play a role, and non-Hispanic white people are at higher risk.
- Other causes could be the use of topical steroids or female hormones and low fiber diets.
Signs and Symptoms of Spider Veins
Spider veins are primarily a cosmetic problem. They are most common on the lower limbs and are often one of the top cosmetic concerns for women in the United States. Many people with spider veins don’t have any symptoms. However, a small number of people might experience discomfort in the form of burning, itching, pain, cramps, or tiredness in their legs.
People with spider veins could have one or more of these risk factors and may also have had vein-related issues before like chronic venous insufficiency (CVI), varicose veins, or venous eczema. On examination, spider veins may look like thin blue, red, or purple vessels. These could be either arterial or venous in origin, either raised or flat.
Spider veins can form on any part of the body and at any age. Nevertheless, they are most commonly found on the face and the legs.
- Burning sensation
- Itching
- Pain
- Cramps
- Leg fatigue
Testing for Spider Veins
Spider veins are identified through a medical examination and the patient’s history; there are not specific lab tests for this condition. However, if the doctor suspects that you have chronic venous insufficiency, a condition where your veins have trouble sending blood from your limbs back to your heart, they may use imaging methods like duplex ultrasound (a type of test that shows how blood is flowing in your veins), contrast venography (an X-ray of your veins), and magnetic resonance venography (an image showing the blood flow within your veins).
Spider veins fall under a classification system (the Clinical, Etiological, Anatomical, and Pathological or CEAP system) that doctors use to categorize chronic venous disease. This system includes seven categories from C0 to C7.
- C0: No visible signs of venous disease.
- C1: Small veins (telangiectasias) and larger veins (reticular veins) can be seen.
- C2: Varicose veins (veins that have a diameter of 3 mm or more).
- C3: Swelling from fluid buildup.
- C4: Changes in the skin or the tissue under the skin. This can include changes in skin color (pigmentation), eczema, hardening of the skin and layer underneath (lipodermatosclerosis), or areas of whitened, scarred skin (atrophic blanche).
- C5: Evidence of a healed venous ulcer (an open sore caused by poor blood flow).
- C6: The presence of a presently open and active venous ulcer.
Another term for spider veins is telangiectasia, which technically means a cluster of small, dilated veins that are less than 1mm wide. Additionally, there’s a classification system by Redisch et al. which describes four types of telangiectasias based on how they look:
- Simple linear: sponge-like network of veins.
- Spider: Veins radiating from a central area like a spider’s web.
- Arborizing: Branch-like, tree-shaped veins.
- Papular: Small, round spots.
Treatment Options for Spider Veins
Spider veins are usually harmless and don’t cause any symptoms. But, they can be unsightly, and many people choose to have them removed for cosmetic reasons. There are several treatments available for this, including sclerotherapy, intense pulse light treatment (IPLT), thermocoagulation, and microphlebectomy. The type of treatment chosen can be influenced by factors specific to each patient, and sometimes a combination of treatments might be used.
Sclerotherapy
Sclerotherapy is often the first-choice treatment for spider veins on the legs. It involves injecting a special solution, a ‘sclerosing agent’, into the veins using a small, fine needle. This solution injures the inner lining of the veins, causing them to close off and stop blood flow. Over time, the treated veins fade away and disappear. However, sclerotherapy does not prevent new spider veins from forming, so multiple treatments might be needed. While it’s generally a safe treatment, some people might experience side effects like temporary darkening of the skin, swelling, and, less commonly, allergic reactions.
Laser Treatment and Intense Pulsed Light (IPL) Treatment
Laser and IPL therapies are non-invasive treatment options for very small spider veins or those located on the face. These treatments work by directing light energy at the veins, which is absorbed by the hemoglobin (the molecule that carries oxygen in red blood cells) in the damaged vessels. This causes the veins to heat up and clot, blocking them off. A variety of different types of lasers can be used for this therapy, each with their specific benefits and drawbacks.
Microphlebectomy
Microphlebectomy is another treatment, where spider veins are removed through tiny skin incisions using small hooks. This method avoids complications like scarring and skin discoloration that can occur with other treatments.
Thermocoagulation
Thermocoagulation is another method which damages the inner lining of the target vein by using heat from a high-frequency pulse. This leads to the vein closing off, fading away, and eventually being absorbed by the body. Remember, your doctor will consider your specific situation and preferences when recommending one or more of these treatment options for your spider vein removal.
What else can Spider Veins be?
Spider veins may indicate Chronic Venous Insufficiency (CVI), a condition that can lead to more severe health issues like varicose veins, venous skin eczema, stasis dermatitis, and leg ulcers. These conditions require medical care before addressing spider veins, which are often just a cosmetic issue. But remember, spider veins might also be an early sign of CVI, so it’s crucial that doctors look out for undiagnosed CVI in patients who show up with spider veins.
In some cases, what appear to be spider veins could actually be spider angiomas. Though these are generally harmless, they can signal more serious diseases such as rheumatoid arthritis, thyroid, and liver disease. Spider angiomas are similar in appearance to spider veins, except for a central red spot with web-like extensions radiating from it.
What to expect with Spider Veins
If spider veins are not treated, they don’t usually cause any serious health problems. They do not affect how your body functions. However, for severe cases, especially on the legs or face, they can impact a person’s self-esteem. This can lead to mental health issues, especially in young women who might be more conscious of their appearance.
Possible Complications When Diagnosed with Spider Veins
Neglected spider veins don’t often lead to complications and typically do not pose any health risks. However, in extreme cases related to varicose veins, the chances of developing skin sores or ulcers, as well as a condition called thrombophlebitis, can increase. Like any medical treatment, there’s a risk of complications when dealing with spider veins, though the risks are low.
Potential Risks:
- Skin sores or ulcers
- Thrombophlebitis (Inflamed veins)
- Other complications linked to the treatment procedure
Preventing Spider Veins
Of course, there’s not much that can be done to change certain risk factors like age, gender, background, and whether or not you’ve been pregnant. However, there are steps you can take to manage other risk factors. This includes maintaining a normal body weight, quitting smoking, staying physically active, and not wearing tight clothing around where the spider veins are. There’s also some evidence to suggest that wearing compression stockings might help avoid new spider veins from appearing after treatment.