What is Left Ventricular Hypertrophy?
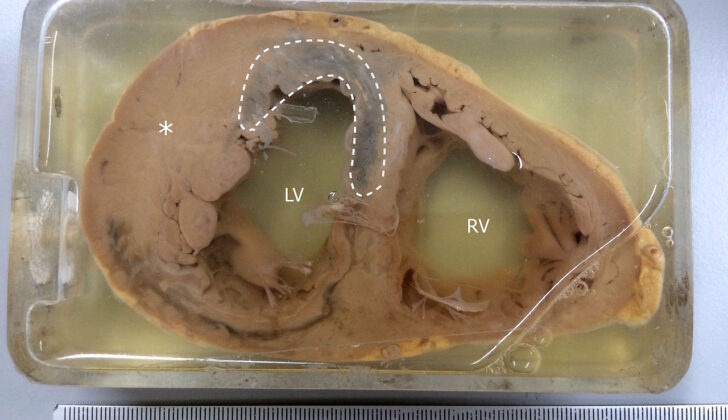
Left ventricular hypertrophy (LVH) is a medical condition where the left ventricle of your heart, which is one of its four chambers, becomes larger than usual. This enlargement can either be because the wall of the ventricle becomes thicker or because the part of the heart that holds blood gets bigger, or both. Most often, the wall of the left ventricle thickens as a reaction to extra pressure, and the chamber becomes enlarged if there’s too much volume or amount of blood.
What Causes Left Ventricular Hypertrophy?
Several health conditions can cause the thickening of the left side of your heart, a condition known as LVH or Left Ventricular Hypertrophy. The most commonly seen causes include:
1. Essential hypertension: High blood pressure that doesn’t have an identifiable cause.
2. Renal artery stenosis: The narrowing of the arteries that carry blood to your kidneys.
3. Athletic heart with physiological LVH: An enlarged heart due to high levels of physical activity.
4. Aortic valvar stenosis: The narrowing of the heart’s aortic valve.
5. Coarctation of the aorta: A birth defect that causes narrowing in part of the aorta, the major artery carrying blood from the heart to the body.
6. Hypertrophic cardiomyopathy: A disease in which the heart muscle becomes abnormally thick.
7. Subaortic stenosis: A narrowing below the aortic valve in the heart.
8. Aortic regurgitation: Leakage of the heart’s aortic valve causes blood to flow in the wrong direction.
9. Mitral regurgitation: A condition in which the heart’s mitral valve doesn’t close tightly, allowing blood to flow backward in the heart.
10. Dilated cardiomyopathy: A condition where the heart’s ability to pump blood is lessened because the heart’s main pumping chamber, the left ventricle, is enlarged and weakened.
11. Ventricular septal defect: A birth defect that involves a hole in the wall that separates the heart’s lower chambers.
12. Infiltrative cardiac processes like Amyloidosis, Fabry disease, Danon disease: These are conditions where harmful substances build up in the heart.
The top two causes, hypertension and aortic valve stenosis, make your heart work harder against high blood pressure. Another cause is the heart getting too full, as seen in conditions like aortic or mitral regurgitation and dilated cardiomyopathy. Sometimes, LVH can be a result of the heart’s healthy tissue working harder to compensate for diseased tissue, as seen in coronary artery disease.
Physical exercise can also cause LVH, where intense training leads to an increase in heart muscle size, thickness, and the size of the chambers. This condition is generally harmless, and the heart’s ability to contract and relax remains normal.
Risk Factors and Frequency for Left Ventricular Hypertrophy
Left ventricular hypertrophy (LVH), a condition where the muscle wall of the heart’s left pumping chamber becomes thickened, is found in around 15% to 20% of the general population. Certain groups are more likely to have this condition, including people of African descent, older individuals, those who are overweight, and patients with high blood pressure.
- An echocardiography study on 37,700 people showed that among those with untreated high blood pressure, 19% to 48% had LVH, and this rose to 58% to 77% among high-risk hypertensive patients.
- People who are overweight have a two times higher risk of developing LVH.
- Depending on the criteria used to define LVH, prevalence rates in the general population range from 36% (using more stringent criteria) to 41% (using less stringent criteria).
- There doesn’t appear to be a significant difference in prevalence between men and women: it’s 36.0% versus 37.9% using more conservative criteria, and 43.5% versus 46.2% using less conservative criteria.
- The subtype of LVH where the heart chamber enlarges without thickening, known as eccentric LVH, is generally more common than the subtype where the chamber wall thickens, called concentric hypertrophy.
Signs and Symptoms of Left Ventricular Hypertrophy
People can live with high blood pressure for a long time without knowing they have it. If high blood pressure is confirmed during three separate visits to the doctor, it’s important to check for signs of damage to key areas of the body. These areas often include the heart, brain, eyes, and kidneys.
Most cases of high blood pressure occur due to general lifestyle factors, and this is known as essential hypertension. But sometimes, there are specific causes such as narrowing of the kidney arteries, a physical defect in the aorta, or metabolic disorders like specific adrenal gland conditions or thyroid problems. Another potential cause is sleep apnea, which has been linked to both lung-related and systemic high blood pressure.
When assessing a patient’s risk, healthcare providers should also consider factors other than high blood pressure. These might include metabolic syndrome, smoking, high ‘bad’ cholesterol levels, diabetes, obesity, a family history of early heart-related deaths, lack of exercise, and kidney abnormalities. It’s also important to note whether the patient uses any over-the-counter medications, particularly herbal ones, that could affect the heart. Excessive alcohol consumption, the use of birth control pills, and illicit drugs like cocaine or amphetamines are also considered potential risk factors.
In those with long-standing hypertension, an eye examination can reveal signs of damage due to high blood pressure, referred to as hypertensive retinopathy. Closely related is hypertensive heart disease, with symptoms typically dependent on the severity and duration of the condition, as well as specific changes to the heart’s structure. Left ventricular hypertrophy, a condition where the muscle wall of the heart’s main pumping chamber becomes thickened, is a common complication. Once developed, potential signs include a specific type of heartbeat sound known as an S4 gallop and signs of changes to the heart muscle.
People who have heart disease due to a physical defect in the aorta typically show specific signs, such as a heart murmur, noticeable when the doctor listens to the heart, or weaker pulses in the lower extremities.
Finally, valve diseases could lead to changes in heart structure, known as hypertrophy, which although initially helpful can eventually lead to heart failure. With conditions like aortic stenosis and insufficiency, patients might have specific types of heart murmurs and other clinical signs related to changes in blood pressures and flow. Notably, patients with long-term aortic insufficiency may present an increased gap between systolic and diastolic pressure, which might lead to pulsations that feel strong and rapid. They may also exhibit a form of hypertrophy resulting from changes in the volume of the left ventricle.
Testing for Left Ventricular Hypertrophy
An electrocardiogram, also known as an ECG, is a simple, quick and affordable test often used to identify a condition called Left Ventricular Hypertrophy (LVH). LVH is a condition where the muscle wall of heart’s left pumping chamber becomes thickened. But, the ECG isn’t a foolproof method as it highly depends on the measurement of the heart’s electricity, making it not very sensitive. Therefore, ECGs can miss cases of LVH, particularly in patients who are overweight, have fluid in their lungs or around the heart, and in those with Chronic Obstructive Pulmonary Disease (a type of lung disease). Also, the results can be influenced by the patient’s age and ethnicity. Nonetheless, the ECG still has its place in diagnosing and monitoring LVH.
Another more effective test for diagnosing LVH is an echocardiogram, which leverages sound waves to create detailed images of the heart. It is a much more sensitive test for LVH, and is also able to identify other heart conditions. During an echocardiogram, the thickness of the heart’s walls and its functioning can be measured, helping the doctor determine if there is LVH. The only downside is that echocardiograms are much more expensive than ECGs.
Finally, we have the ‘gold standard’ of tests for diagnosing LVH – the Cardiac Magnetic Resonance Imaging (MRI). This test is considered the most accurate and consistent method for estimating the size of the left ventricle and recognizing other abnormalities in the heart’s structure. Unfortunately, the use of cardiac MRI is often limited due to its high cost, logistics, and limited availability, but it plays a significant role in research and in assessing heart anatomy for special cases.
Treatment Options for Left Ventricular Hypertrophy
If you have Left Ventricular Hypertrophy (LVH), which means your heart’s main pumping chamber is thicker than normal, your treatment will depend on what’s causing it. Here’s what your doctor will likely recommend:
Firstly, they’ll ask you to make lifestyle changes. LVH increases your risk for heart disease and other deadly cardiovascular conditions, so it’s important to take it seriously.
If your LVH is due to high blood pressure, controlling your blood pressure is vital to prevent further heart damage. This could involve prescription medications like ACE inhibitors or ARBs, long-acting calcium channel blockers, or diuretics. These not only help to manage your blood pressure but can also reduce the thickness of your heart muscle and decrease your risk of future heart problems.
The second common cause of LVH is aortic stenosis, a condition where the gateway from your heart to your aorta (the main artery in your body) narrows. When you have aortic stenosis, it takes a lot longer for your heart to pump blood into your body, which can thickens your heart muscle over time. Most patients with aortic stenosis have a delay of 10 to 20 years before they notice any symptoms. During this time, the condition can start transforming the composition of your heart and lead to LVH.
If you have this and start to experience symptoms, your doctor will likely recommend a surgery called aortic valve replacement. If you’re not having symptoms but tests (like an echocardiogram) show your aortic stenosis is getting worse and affecting your heart function, your doctor might also recommend surgery. This can help improve your heart function and reduce your risk of dying from heart complications.
If you’re an athlete and have what’s called “physiologic LVH,” you won’t need treatment. This is when the heart muscle gets thicker because of intense physical training, like what professional athletes do. If you stop training for a few months, this kind of LVH usually gets better on its own.
In cases of hypertrophic cardiomyopathy, where a part of your heart is thicker than the other parts, treatment includes medicines like beta-blockers and calcium channel blockers. These help slow your heart rate and decrease the force of your heart muscle contractions, which lets your heart fill with blood more easily. If these don’t resolve your symptoms, a type of heart surgery called a myomectomy or a procedure known as septal ablation may be needed. In this scenario, other medications like diuretics or ACE inhibitors might make your heart condition worse, so they’re typically avoided.
What else can Left Ventricular Hypertrophy be?
One of the most difficult medical challenges is distinguishing between changes in the heart’s structure (left ventricular hypertrophy) due to athletic activity and those resulting from hypertrophic cardiomyopathy, a disease that can cause sudden death during exercise in young athletes under 35. A detailed evaluation of the heart using echocardiography, a type of ultrasound test, is valuable in reaching a diagnosis.
There are several conditions that could be responsible when changes in the left side of the heart are observed:
- High blood pressure
- Narrowing of the kidney artery
- A heart conditioned by athletic activity
- Narrowing of the aortic valve
- Narrowing of the aorta
- Hypertrophic cardiomyopathy, with or without obstruction of the outflow tract
- Obstruction of the left ventricular outflow tract due to muscle or membrane
- Leaky aortic valve
- Leaky mitral valve
- Enlarged heart
- Hole in the wall between the heart’s ventricles
- Diseases in which abnormal material infiltrates the heart, like Amyloidosis, Fabry disease, Danon disease
What to expect with Left Ventricular Hypertrophy
The condition known as LVH (Left Ventricular Hypertrophy), or the thickening of the heart’s left ventricle, signals an increased chance of heart-related diseases and death. This remains true even when considering common risk factors for heart disease like age, smoking, obesity, high blood cholesterol, high blood pressure, and diabetes. What it means is that having LVH independently increases your chances of developing heart diseases.
If a patient develops LVH, it significantly raises the possibility of having heart diseases like myocardial ischemia (insufficient blood flow to the heart), a heart attack, heart failure (when the heart can’t pump blood as well as it should), abnormal heart rhythms, or even sudden death. Simply put, the higher a person’s left ventricular mass (LVM or the weight of the left side of your heart) is, the greater the risk. On a positive note, if LVH could be reversed or lessened, the risk of these heart complications decreases.
Possible Complications When Diagnosed with Left Ventricular Hypertrophy
People with left ventricular hypertrophy (LVH) often don’t show symptoms for a few years. This is because their hearts are still able to compensate for the added pressure or volume overload. However, as the condition worsens over time, it can cause problems with both the heart’s ability to contract (systolic dysfunction) and its ability to relax and fill with blood (diastolic dysfunction). This could eventually lead to final stage heart failure.
In addition to this, because the heart of a person with LVH needs more oxygen than usual, this can sometimes cause chest pain (angina) or other signs of a lack of blood flow to their heart (ischemic symptoms). LVH can also disrupt normal electrical signals in the heart causing irregular heart rhythms (arrhythmias). One such arrhythmia is a very fast, chaotic heartbeat in the upper chambers of the heart (atrial fibrillation) which can increase the risk of having a stroke due to blood clots.
Briefly, following complications can arise due to left ventricular hypertrophy (LVH):
- Development of systolic dysfunction (issues with heart’s ability to contract)
- Diastolic dysfunction (issues with heart’s ability to fill with blood)
- End-stage heart failure
- Chest pain (Angina)
- Ischemic symptoms (signs of inadequate blood flow to the heart)
- Arrhythmias (Irregular heart rhythms)
- Atrial fibrillation (increased risk of strokes)
Preventing Left Ventricular Hypertrophy
People should understand the importance of adopting healthier lifestyle habits for better control of their blood pressure. This includes quitting smoking, steering clear of inactive habits and keeping active (working out at least three times a week), lessening salt consumption (below 2 grams/day), and avoiding alcohol. People should also be aware of the dangers associated with uncontrolled blood pressure and appreciate the convenience of home monitoring devices, as well as keeping a daily record of their blood pressure readings.
Hypertension, or high blood pressure, is a frequent and easy-to-improve cause of LVH (enlargement of the heart’s main pumping chamber). Therefore, proper management is crucial as it not only averts further worsening but may also reverse LVH. Following a healthier lifestyle is as crucial to curbing cardiovascular diseases and premature death as taking prescribed medication regularly.