What is Porcelain Aorta?
Porcelain aorta (PA) is a condition that affects the main blood vessel leading from the heart, known as the aorta. The disease is characterized by severe and widespread hardening, or calcification, of the walls of the ascending part of the aorta that extends to the aortic arch and the descending aorta. The hardening mainly affects the front of the ascending aorta and the top wall of the aortic arch, forming a complete or near-complete ring around the aorta.
The exact definition of porcelain aorta can vary depending on who is describing it. But generally, it is used to describe aortic hardening that causes difficulties in aortic cannulation (insertion of a tube into the aorta), clamping of the aorta, cutting into the aorta, or bypassing the coronary artery. These issues can require changes in surgery procedures to avoid complications. If you have PA, this could make surgical procedures more challenging and hazardous. Further, the hardening of the aorta is associated with an increased risk of complications during procedures. It’s also a predictor of a higher chance of death in patients undergoing surgery.
There are two ways to classify porcelain aorta, depending on where and how the calcium deposits form:
1. The calcium can deposit on the internal layer of the aorta, called the tunica intima, starting from the base of plaque buildup. This is known as the atherosclerotic type.
2. In the non-atherosclerotic type, the calcification typically happens in the middle layer of the aortic wall, known as the tunica media.
Based on where the calcification is in the thoracic aorta, porcelain aorta can also be categorized into two main types:
* Type I – This is where the hardening forms a ring around the ascending aorta, regardless of how far this extends. This type is then divided into two subtypes:
* Type IA has a so-called ‘calcification score’ above 75%. This score indicates the ratio of calcified aortic circumference to the full circumference of the ascending aorta. A high score like this could prevent the clamping of the aorta in heart surgeries.
* Type IB has a calcification score under 75%, meaning clamping the aorta might still be possible but comes with increased risks.
* Type II – This refers to the hardening that occurs only in the aortic arch and the descending aorta.
What Causes Porcelain Aorta?
Porcelain aorta refers to a condition where the large blood vessel that supplies blood from the heart to the rest of the body, the aorta, hardens and becomes brittle. This condition is often associated with various health issues, including long-term kidney disease, radiation that targets the middle of the chest (mediastinum), and long-term inflammation in the whole body from diseases such as Takayasu arteritis, systemic lupus erythematosus and rheumatoid arthritis.
Several risk factors have been identified that could lead to porcelain aorta according to research studies. Common factors include genetic predisposition (a family history of the disease), getting older, diabetes, radiation exposure, high levels of toxins in the blood due to kidney disease (uremia), and Takayasu arteritis, an inflammation of the arteries.
Additionally, there are other factors associated with a specific type of porcelain aorta caused by buildup of fat in the artery walls (atherosclerosis). These factors include high blood pressure, high levels of fats in the blood (hyperlipidemia), smoking, alcoholism, a lifestyle with little to no physical activity (sedentary lifestyle), obesity, and inflammatory diseases, such as systemic lupus erythematosus and rheumatoid arthritis.
Risk Factors and Frequency for Porcelain Aorta
Porcelain aorta, although relatively rare, has been more commonly identified in people aged 60 and older, especially those with issues such as heart disease, chronic kidney disease, and rigid narrowing of the aortic valve. Depending on different studies, its incidence rate can be anywhere from 1% to 20%. For example:
- In a study where 1861 patients underwent heart bypass surgery, 1.2% had a porcelain aorta.
- In a study involving a special valve placement procedure, 15.1% patients had it.
- In another study involving a special kind of valve replacement, 18% patients had it.
- Other studies found 5% and 11% incidence rates.
- A study of 240 patients found 7.5% had a porcelain aorta.
However, there seems to be differing results when it comes to whether males or females are more likely to have a porcelain aorta. Some studies show it is more common in males, other studies have found it to be more common in females. For instance, among patients having a specific kind of valve replacement for severe aortic stenosis, there was a higher incidence of porcelain aorta among females. However, among patients who underwent coronary revascularization surgery, more males had porcelain aorta.
Signs and Symptoms of Porcelain Aorta
Important details about a patient’s medical background and physical check-ups in cases of porcelain aorta are usually connected to their pre-existing health problems and risk factors.
Testing for Porcelain Aorta
Porcelain aorta is a condition that doesn’t usually have symptoms and is often found unintentionally when a patient is being checked for other heart or lung conditions. It can be noticed on chest x-rays or CT scans that were done for other reasons.
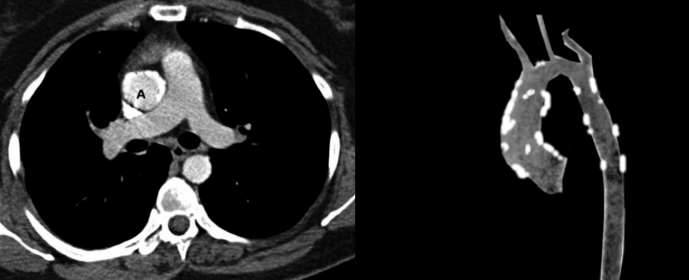
Various methods have been suggested to diagnose porcelain aorta and to understand its size and exact location before any heart procedures. Most accurately, a method called a multislice computed tomography (MSCT) is used. This can clearly diagnose porcelain aorta and give vital information about the specific level and location of the aortic hardening (or calcification). This allows for the distinction between PA, which involves hardening all around the aorta, and less widespread aortic calcification. In addition, MSCT images can be used to create a 3-dimensional (3D) map of the aortic wall. This allows for understanding the 3D distribution of the hardening.
Other methods for diagnosis include:
– A chest X-ray can sometimes show hardening in the thoracic aorta, but it is not accurate in defining PA.
– Fluoroscopy, which is used during a coronary angiogram, is somewhat good at detecting aortic hardening suggesting PA, but it lacks accuracy when assessing the distribution and location of this hardening.
On the other hand, during heart surgery PA can be noticed by performing an epiaortic echocardiographic scan of the aorta and physically touching the aorta after sternotomy (an incision made in the sternum) and exposure of the aorta. This can confirm the presence of PA including its extent and exact location.
It’s important to know beforehand if a patient has porcelain aorta as the plans for a procedure often changes if it’s discovered. If PA is suspected due to incidental findings on other imaging techniques, a pre-procedure CT scan can help evaluate PA.
Treatment Options for Porcelain Aorta
During heart surgeries, advanced surgical techniques are required for patients with a condition called “porcelain aorta.” Porcelain aorta is a heavily calcified (or hardened) aorta. The aorta is the main artery that carries blood away from your heart to the rest of your body. These techniques are necessary to avoid disturbing the hardened aorta, which could lead to strokes and systemic embolism—a condition where blood clots travel through the bloodstream and block blood vessels elsewhere in the body.
Patients with porcelain aorta face increased risks during coronary artery bypass grafting (CABG), a procedure that improves blood flow to the heart. This is mainly due to the heightened risk of stroke from the heavily calcified aorta when it is handled during the operation. Such risks occur in different stages of the surgery mainly: getting into the aorta with a tube (cannulation), placing a clamp on the aorta, and partial clamping for connecting natural or artificial tubes (anastomosis).
A series of modifications have been proposed to avoid dealing with the hardened aorta directly including:
1. No-touch technique or aortic off-pump coronary artery bypass grafting: Where the surgery is done while the heart is still beating.
2. Doing the operation while the body is cooled to a very low temperature (deep hypothermic circulatory arrest).
3. Inserting a tube through the groin or underarm artery.
A popular method nowadays is the “no-touch technique,” where the surgery is done on the beating heart, thereby bypassing the need to manipulate the porcelain aorta. By using this method, fewer cases of death during or immediately after the surgery and fewer cases of stroke were recorded. However, a drawback is that not all required blood vessels could reach the heart, compared to traditional CABG surgery.
In cases where there is a portion of the aorta that is not calcified (confirmed through ultrasound), a procedure can be done where tubes are connected without the need for clamping the aorta. The effectiveness of this was shown in a couple of studies, where successful connective procedures were carried out with minimal neurological complications.
Another valuable method is doing CABG during deep hypothermic circulatory arrest. This gives the surgeon time to perform the surgery without clamping the aorta, thus decreasing the rate of brain complications.
In some cases, the porcelain aorta may prevent the usual insertion site for tubes used in heart surgeries. In such a case, other, less preferred, sites need to be used. The classic approach is to use the femoral artery, the large artery in the groin. But this carries the risk of embolism because of the blockage going backwards in the artery. Another site would be through the axillary artery, under the collarbone. This method carries less risk of brain embolization but can come with other local complications such as artery dissection and nerve injuries.
For patients with porcelain aorta who need surgery for the mitral valve (a valve in the heart that lets blood flow from one chamber to another), avoiding clamping the aorta can be achieved using body cooling and allowing the heart to fibrillate (or quiver) during surgery.
Patients with porcelain aorta and a condition known as aortic stenosis, where the heart’s aortic valve narrows preventing blood flow to the aorta, can benefit from newer methods like the transcatheter aortic valve replacement (TAVR). This method is less invasive and replaces the aortic valve without having to clamp the aorta. In studies, TAVR proved to be successful in most patients and the rates of stroke and death within thirty days were similar to patients without porcelain aorta.
What else can Porcelain Aorta be?
“Porcelain aorta” is a medical term that’s identified by looking at radiographic images (like X-rays or CT scans). It doesn’t have many conditions that look similar to it. Often, older patients show minor hardening or calcification in the thoracic aorta (the largest artery in the chest). However, porcelain aorta is considered the most severe form of this type of calcification.
What to expect with Porcelain Aorta
A porcelain aorta, a condition often found by accident, is usually linked with widespread hardening and narrowing of the arteries (atherosclerotic cardiovascular disease), chronic kidney disease or previous radiation therapy to the chest. Generally, the overall health outlook of patients with porcelain aorta is linked to their pre-existing medical conditions.
Possible Complications When Diagnosed with Porcelain Aorta
A porcelain aorta is often found by chance when people are being checked for heart or lung diseases. This condition is usually accompanied by a buildup of calcium on the heart valves and arteries, which can lead to problems with restrictive valve disorders and painful, inadequate blood supply to the heart due to coronary artery disease. Heavy calcification of the aorta can also narrow the diameter of the aortic lumen, which offers more resistance to the flow of blood pumped out of the heart’s left ventricle. Over time, this condition may cause the heart to enlarge, lead to congestive heart failure, and irregular heart rhythm. Some research has also linked a higher risk of death over time, unfavorable results related to heart problems, and strokes in patients with calcification of the aorta.
Surgery on the heart is much more complicated for patients with a porcelain aorta. Managing these patients can be difficult due to the elevated risk of atherosclerosis – a condition in which plaque builds up inside the arteries causing an operation, and aortic dissection – a serious condition involving a tear in the aorta’s inner layer, during or after surgery. Patients with a porcelain aorta are also at high risk for stroke caused by atherosclerosis getting dislodged and blocking blood flow to the brain during surgery.
Potential risks and complications:
- Restrictive valve disorders
- Inadequate blood supply to the heart
- Narrowing diameter of the aortic lumen
- Enlargement of the heart
- Congestive heart failure
- Irregular heart rhythm
- Higher risk of death over time
- Unfavorable results related to heart problems
- Strokes
- Elevated risk of atherosclerosis during or after surgery
- Elevated risk for aortic dissection during or after surgery
- High risk for stroke during surgery