What is Silent Myocardial Ischemia?
Silent myocardial ischemia is a condition where blood flow to the heart muscle (also known as myocardium) is reduced, yet it doesn’t cause noticeable symptoms such as chest pain or discomfort. This condition is the most typical way coronary artery disease (CAD) appears. Coronary artery disease is when your heart’s major blood vessels become damaged or diseased. Different tests such as EKG (heart’s electrical activity test), echocardiography (heart ultrasound), and detecting abnormalities in blood perfusion (flow) can identify silent heart damage. Silent ischemia is often seen in patients with stable CAD, but it can also occur in people who have no history of CAD.
Silent ischemia is a significant indicator of a higher risk of death. Between 70% to 80% of short episodes of decreased blood supply to the heart do not show symptoms of chest pain. The risk is that because there’s no pain in silent ischemia, patients might not seek medical help on time, which can increase their risk of severe health problems and even death. Elderly patients with diabetes or those who’ve had a history of heart muscle injury or treatment to improve blood flow to the afflict area are more prone to this condition.
The diagnosis of silent ischemia requires evidence of reduced blood supply, which can be determined by changes in heart activity during a walk or stress test, differences in heart wall movements during exercise or a specialized test using a drug called dobutamine, or abnormalities in blood flow at rest using a nuclear scan.
Now, regarding heart’s anatomy, it’s a muscle organ in your chest, slightly to the left of centre. It has four parts: the right and left atriums, where blood enters the heart, and the right and left ventricles, which pump out blood to your lungs and the rest of your body. The heart is covered by a protective bag called the pericardium.
The coronary arteries branch out from a larger artery (the aorta), bringing oxygen-rich blood to your heart muscle. The left coronary artery splits into the left anterior descending and circumflex arteries. The former provides blood to the front wall and parts of the inner wall of the left ventricle, and the latter supplies the left ventricle’s side wall. The right coronary artery supplies the right atrium and ventricle, and the back wall of the left ventricle.
These coronary arteries go into the heart muscle and form a network of smaller arteries that deliver oxygen and nutrients needed for the heart to work properly. If blood flow through these arteries is disrupted by conditions like hardened arteries (atherosclerosis) or coronary artery disease (CAD), it may lead to regional wall motion abnormalities.
The heart muscle has specialised tissue that allows your heart to contract and relax. When the heart contracts efficiently, it can distribute blood throughout your body effectively. Any abnormal wall movement, picked up by tests like echocardiography, may suggest damage or dysfunction in specific heart regions. This dysfunction could be due to inadequate blood supply from blocked coronary arteries, leading to conditions like heart muscle damage or ischemic heart disease.
Your heart’s electrical system initiates from the sinoatrial node, which creates the electrical signals responsible for starting each heartbeat. These signals spread through the atriums, seen as the P wave on the EKG. After a short delay at the atrioventricular node, the signal travels through the bundle of His, bundle branches, and Purkinje fibers, causing the ventricles to contract, depicted by the QRS complex on the EKG. The recovery phase is shown as the T wave on the EKG.
Silent myocardial ischemia often occurs due to blockages in the coronary arteries, causing insufficient blood flow to the heart muscle without noticeable symptoms. Understanding the detailed relationship between the structures of the heart and coronary arteries, and the function of the heart muscle is crucial in managing and determining the best treatment methods for patients with silent myocardial ischemia.
What Causes Silent Myocardial Ischemia?
Silent myocardial ischemia, a condition where the heart muscle doesn’t get enough oxygen, can be caused by various things. These include the rupture of a fatty deposit in the arteries (atherosclerotic plaque), spasm or inflammation (vasculitis) of the arteries, injury, blockage of a blood vessel (coronary embolism), certain drugs like cocaine, and imbalance of oxygen supply to the heart and its demand.
Risk factors also play an important role in this condition. They increase the likelihood of having silent myocardial ischemia, meaning the patient experiences no symptoms. These factors include:
Diabetes: If you have diabetes, you’re at a high risk of developing coronary artery disease (CAD), which is closely related to silent myocardial ischemia. This is often due to dysfunction in the part of your nervous system that regulates your heart (cardiac autonomic function). Studies have shown that if you have a harmful type of cholesterol in your blood (atherogenic dyslipidemia), you’re more likely to have silent myocardial ischemia. Therefore, managing your cholesterol levels is beneficial.
Undergoing surgery: Older people who had heart surgery (coronary artery bypass grafting) experienced silent myocardial ischemia, which was detected by a special type of heart monitor (Holter monitoring). Since silent myocardial ischemia might show no symptoms, it’s often recommended monitoring with ECG during surgery. Having a previous heart attack or blocked blood vessels in the limbs (peripheral artery disease) increases the risk of having a heart attack during surgery (perioperative myocardial infarction).
Being older: Silent myocardial ischemia is more common in older people. In fact, a study of 678 healthy men and women showed that about 11.4% had silent myocardial ischemia. This group was also three times more likely to experience adverse heart-related events.
Being in intensive care: Patients in the intensive care unit (ICU) admitted for non-heart related causes are also at risk of having a sudden decrease in blood flow to the heart (acute myocardial ischemia). Having temporary heart-related blood limitations and being older are primary predictors of heart problems in these patients.
Having sleep apnea: Sleep apnea is a disorder where breathing intermittently stops during sleep. This condition is linked with silent myocardial ischemia, irregular heart rhythms, high blood pressure in the lungs (pulmonary hypertension), heart failure, blockages in the brain (transient ischemic attack), and stroke.
Risk Factors and Frequency for Silent Myocardial Ischemia
Prior heart disease is common in patients with severe heart attacks (acute myocardial infarctions). Research shows that 15% to 30% of these patients previously had silent heart attacks, those that occur without any noticeable symptoms. Additionally, 30% to 40% of patients with unstable chest pain (angina) also had experienced a heart attack. Specifically, patients who have chronic chest pain (stable angina) have a history of heart attacks in 20% to 50% of the cases. We also find that heart disease in multiple blood vessels is more common in patients whose silent heart attacks were discovered during a stress test. In a study of 937 patients with stable heart disease, around 20% showed silent heart attacks during a stress test.
In contrast, silent heart attacks are rare in individuals without prior heart disease. In a study of 4842 patients, only about 0.89% had a silent heart attack. Nonetheless, the chances of having a silent heart attack increase with the presence and number of other risk factors. For example, amongst 631 symptom-less patients with diabetes and two other risk factors, 22% had had a silent heart attack. Plus, the calcium score of the coronary artery, a measure of the amount of calcium deposit, can predict the likelihood of a silent heart attack. A higher score suggests a greater probability.
Gender influences the chances of silent heart attacks too. Men are more likely to have them than women. Despite this, both genders face a higher risk of dying from heart disease and all causes if they experience silent heart attacks. However, the increase in risk is believed to be higher for women.
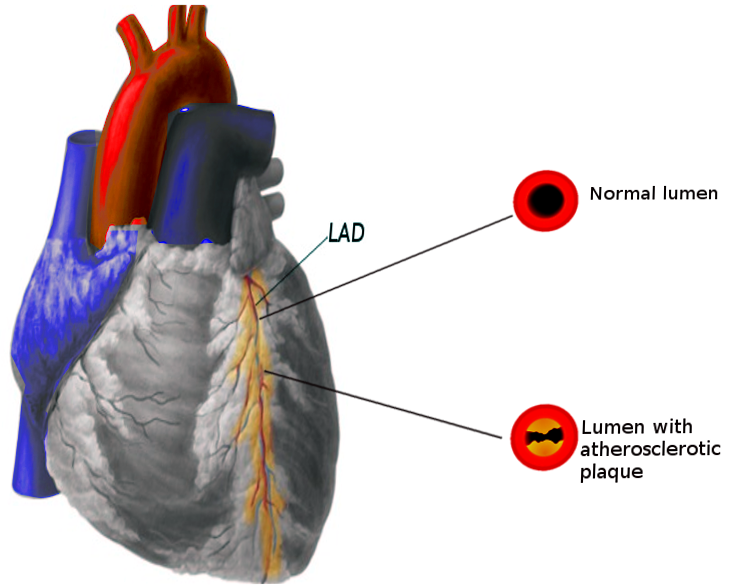
caused by an atherosclerotic plaque that blocks the lumen of a coronary artery,
typically the left anterior descending artery.
Signs and Symptoms of Silent Myocardial Ischemia
Silent myocardial ischemia, a heart condition where the heart doesn’t get enough oxygen, can show up in different ways:
- Type I: The person has no symptoms and has never had a heart attack. The condition is found during monitoring or stress testing.
- Type II: The person has no symptoms but has a history of heart problems where the heart didn’t get enough oxygen.
- Type III: The person has known heart disease, either with or without symptoms. This is the largest group.
People with this condition might have chest pain because the heart isn’t getting enough oxygen. They could have no history of heart attacks or angina (chest pain), a history of heart attacks, or both chest pain and episodes where they aren’t aware the heart isn’t getting enough oxygen.
Doctors use the person’s current symptoms and a physical exam to understand more about what’s going on. Relevant issues might include diabetes, high blood pressure, abnormal cholesterol levels, heart disease, or other risk factors for heart disease. The physical exam might not show anything unusual, or might suggest worsening heart function, such as an abnormal heart sound called an S3, or signs of lack of oxygen to the heart, such as an S4.
Testing for Silent Myocardial Ischemia
If you have an ECG (a test that measures the electrical activity of your heart) result showing a 1-mm drop or flat line, it can suggest a lack of blood flow to your heart tissue, particularly if your ECG was normal before. Blood tests for a protein known as troponin-I and the use of a wearable ECG monitor can help doctors identify if any heart damage has occurred after surgery. These tests can also be helpful for older people or patients with diabetes who are at risk of coronary artery disease, which is a condition that reduces blood flow to the heart. Tests involving radioactive substances can be especially good at finding areas of reduced blood flow in people who don’t have any symptoms.
Doctors use a few different tests to look for “silent” heart damage, meaning heart damage that doesn’t cause noticeable symptoms. They may monitor your ECG in the hospital to continuously assess your heart’s electrical activity and find changes that suggest a lack of blood flow. They can also test your blood for specific enzymes or proteins that enter your bloodstream when your heart tissue is damaged. Wearing an ECG monitor while carrying out your daily activities can provide useful information about any episodes of silent heart damage. Exercise stress testing, which measures your heart’s response to exercise, can help detect changes due to a lack of blood flow when you’re active. Imaging techniques that involve radioactive substances can assess the function of your blood flow to your heart and identify areas with reduced flow.
For patients at high risk, doctors can place monitors directly in the heart to continuously assess its function and detect any issues with blood flow in real-time. A computed tomography (CT) scan can provide a detailed picture of the structure of your heart arteries and muscle.
These tests can give valuable information about whether you have reduced blood flow to your heart tissue and how severe the problem is. This information can help guide treatment decisions and determine your risk level. Using multiple tests together can increase the accuracy of the diagnosis and improve the care and outcomes of the treatment.
Treatment Options for Silent Myocardial Ischemia
Beta-blockers are commonly used to improve outcomes for people with silent heart muscle damage, also known as silent myocardial ischemia. These medications can notably reduce the number and duration of ischemic episodes, which are periods when your heart muscle doesn’t get enough oxygen.
Calcium channel blockers (CCBs) are another effective treatment option. They are typically the first choice for patients with conditions that respond well to these drugs, like vasospastic angina, which is a type of chest pain, or for patients who cannot tolerate beta-blockers.
In addition, aspiring is used for its antiplatelet properties to help prevent blood clots from forming, and statins are used to lower cholesterol levels. For some patients, doctors may recommend a combination therapy of beta-blockers, nitrates, and CCBs especially if the patient continues to show signs of ischemia as observed on ambulatory monitoring or radionuclide scans, which are types of tests that monitor heart health.
Regarding coronary artery revascularisation, a process to restore blood flow to the heart, decisions about its need are not solely dependent on findings of silent myocardial ischemia. The evidence supporting the effective use of this procedure to treat this condition is limited. One study found no significant difference in death rates between patients who had revascularisation and those who continued with medical therapy. However, for patients with high-risk features, such as ischemia affecting large areas of the heart muscle, this procedure can be considered.
Finally, managing psychosocial stress is another crucial part of treatment. Mental stress can trigger silent ischemia, particularly in patients with existing coronary artery disease (CAD), which is a disease of the arteries supplying blood to the heart. Some evidence suggests that reducing behavioral stress can benefit individuals with CAD.
What else can Silent Myocardial Ischemia be?
If someone is experiencing chest pain, a doctor will consider several possible causes. These may include:
- Aortic dissection: This is when there’s a tear inside the main vessel that takes blood away from the heart (the aorta). It can lead to serious, life-threatening bleeding. The main symptom is chest pain.
- Pleurisy: This is inflammation of the lining of the lungs, which can cause sharp chest pain that gets worse when you breathe or cough. It can also lead to breathlessness.
- Pulmonary embolism: This condition happens when a blood clot blocks an artery in the lungs. It causes sudden shortness of breath and chest pain.
- Myocarditis: This is inflammation of the heart muscle. It can cause tiredness, chest pain, and shortness of breath.
- Lung diseases: Various conditions such as pneumonia, fibrosis (scarring), or lung cancer can cause problems with breathing.
- Musculoskeletal or gastrointestinal issues: Conditions affecting the muscles, bones, or digestive system can also cause chest pain or discomfort. This could be something like costochondritis (inflammation of the cartilage in the chest), acid reflux, or spasms in the food pipe.
However, not all chest pain is caused by heart disease. For example, ‘silent heart disease’ doesn’t usually cause any symptoms. But if it gets worse and turns into a heart attack, it can cause chest pain and breathing problems. Careful exploration of the patient’s medical history and well-considered diagnostic tests can help doctors tell the difference between silent heart disease and other conditions.
What to expect with Silent Myocardial Ischemia
The outcomes of silent heart disease, or ‘silent myocardial ischemia’, depend on the patient’s overall health and if they have certain risk factors or other illnesses like ischemic heart disease. Patients with a history of stable heart pain, or ‘angina’, have a worse outlook. If a patient has silent heart disease but does not report symptoms, they have double the risk of having a heart event in the future.
Patients with silent heart disease that is tracked and documented using monitoring devices stand a higher chance of succumbing to heart-related death. Additionally, silent heart disease following an episode of acute coronary syndrome (a blockage in the coronary arteries that interrupts blood flow to the heart) increases the risk of future adverse events.
If a patient does not have coronary artery disease (CAD – a condition where the heart’s arteries start to narrow due to a build-up of fatty matter), but has silent heart disease that can either be induced or detected through monitoring, this is associated with increased risk of negative heart-related events and premature death.
Individuals with a history of silent heart disease are more likely to suffer new coronary events – heart conditions resulting from the blood supply to the heart being blocked – than people without silent heart disease. Therefore, these patients must undergo rigorous tests and receive aggressive treatment. Additionally, older patients can show unusual symptoms during a heart attack, like confusion, nausea, and abdominal pain. Adopting a healthier lifestyle and managing controllable risk factors can significantly improve patients’ quality of life.
Preventing Silent Myocardial Ischemia
The main way to prevent a condition called silent myocardial ischemia, which is linked to heart disease, is by managing things that increase your risk of having heart problems. To lower the chances of developing this condition, you should adopt healthy habits like regular exercise and a balanced diet that’s low in fats and cholesterol. Keeping your weight healthy and avoiding smoking can also help. Furthermore, controlling high blood pressure and diabetes, and making sure your cholesterol levels are good, can also lower the risk. Regular health check-ups and screenings for things that increase heart disease risk are crucial. This will help to find any problems early and manage them correctly before silent ischemia develops and causes complications.
If you have been diagnosed with silent ischemia, whether it’s causing symptoms or not, it’s highly recommended to join a special heart disease management program. These programs will help you manage lifestyle factors that can be changed, manage stress, anxiety, and depression, and help you improve your ability to exercise after leaving the hospital. This approach can lower the chances of disease and death. It’s very important for those with diabetes to properly manage factors that can increase the risk of heart disease. The best practice is to have an ECG – a test that checks your heart’s activity – as part of your annual health check-up. Patients with silent myocardial ischemia often are older and have multiple health problems. A team of health professionals working together is needed to manage such patients until they complete their heart disease management program.