What is Nocardia Keratitis?
Nocardia is a type of bacteria with certain characteristics that can sometimes cause eye diseases, particularly infection of the cornea (the clear front surface of the eye). This specific condition is known as Nocardia keratitis. Because this condition is not well-known and its symptoms can be quite general, it can often look like other, more common eye infections. This can lead to missed or late diagnoses.
Another important point is that Nocardia keratitis doesn’t always respond well to the common medications used for treating bacterial infections of the cornea, such as a group of drugs called fluoroquinolones. This can potentially cause patients to experience ongoing discomfort and problems until the right diagnosis is made and the appropriate treatment is given.
What Causes Nocardia Keratitis?
Nocardia, initially identified as a type of fungus, is a group of thread-like bacteria that includes over 80 different types. These bacteria are found all over the environment, in places like water, dust, soil, mud, and decaying plants.
Nocardia doesn’t naturally occur in the eye, so Nocardia keratitis, an eye infection caused by this bacteria, must happen due to contact with the bacteria in the surrounding environment.
For many years, Nocardia asteroides, one particular species of bacteria, was mostly found in cases of Nocardia keratitis. However, new techniques in Genetic Analysis (PCR and RNA sequencing) have shown that other species such as Nocardia arthritidis are more common in some groups of people.
Studies have found that almost half of all Nocardia keratitis cases had previous exposure to soil or plant matter. The most common cause of Nocardia keratitis is injury to the cornea, the clear layer at the front of the eye. In fact, in one study, injury was the initial cause in 25% of cases. Other risk factors include having eye surgery like LASIK or PRK, use of eye drops containing steroids, and wearing contact lenses, especially if they’re worn for extended periods or not cleaned properly.
Risk Factors and Frequency for Nocardia Keratitis
Nocardia, a type of bacteria often found in the soil of South Asia, is rarely diagnosed as causing keratitis (an inflammation of the cornea in the eye) outside this region. In some studies from South India, this particular bacteria was identified in anywhere from 1.7% to 8.34% of bacterial keratitis cases.
As a general note, bacterial keratitis can be more common in males, young adults, and those living in rural locations. This could potentially be due to an increased possibility of minor eye injuries and exposure to environment factors in these groups.
Signs and Symptoms of Nocardia Keratitis
If you think there might be something wrong with your eyes, it’s important to get a thorough check-up with a healthcare provider. They’ll ask you about your history and any risk factors unique to your situation to see if you might have an eye infection. If you’ve recently traveled to Asia, they’ll look especially carefully for signs of a specific type of eye infection called Nocardia keratitis.
The common signs of Nocardia keratitis can be pretty general. They include severe eye pain, involuntary blinking or eye spasms, aversion to light, and swelling of the eyelid.
After inquiring about your history, your healthcare provider will do a detailed eye exam. They will use a device called a slit-lamp to look for signs of Nocardia keratitis or other infections. Nocardia keratitis can show up as patchy infiltrates (collections of inflammatory cells) in the front part of the stroma (a layer of the eye) arranged in a ring-like pattern, often with additional small lesions scattered about. These infiltrates are usually found in the middle and outer parts of the cornea, often near an area of the cornea that was previously injured. But Nocardia keratitis can also present in other ways, including “speckled” epitheliopathy or an ulcer studded with small, yellow infiltrates. Sometimes the infection can spread into the stroma, a deeper layer of the cornea.
- Severe eye pain
- Involuntary blinking or eye spasms
- Aversion to light
- Swelling of the eyelid
- Patchy infiltrates, often in a ring-like pattern
- Additional small scattered lesions
- “Speckled” epitheliopathy or ulcer with small, yellow infiltrates
Testing for Nocardia Keratitis
In layman’s terms, if your doctor suspects you might have Nocardia keratitis, an eye infection, they can initially make a diagnosis based on your reported symptoms and the results of their physical examination of your eyes. Despite this, the most reliable way to confirm that you have Nocardia keratitis is to get a sample from your cornea (the clear front surface of your eye) and culture it (grow it in a lab dish) to see if Nocardia bacteria grow. These bacteria can grow on different types of lab media, such as blood agar, chocolate agar, and Sabouraud agar.
However, it’s important to know that Nocardia bacteria grow slowly. Normally, these bacteria display growth in about 5 to 7 days, but sometimes it can take up to two weeks. So, it’s important to wait for at least two weeks before concluding that the culture results are negative (no bacteria have grown).
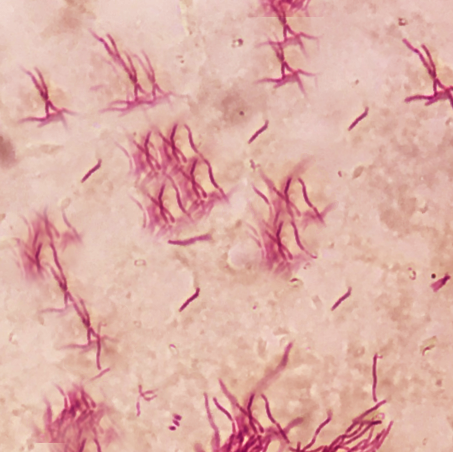
In addition to the culturing method, there are other ways to diagnose Nocardia keratitis. A study showed that using stains like Gram or 1% acid-fast (Ziehl-Neelsen) on a corneal sample could lead to an early diagnosis. Another tool is in vivo confocal microscopy (IVCM), a sophisticated, non-invasive technique that allows doctors to look at the cells of your cornea in real-time. Nocardia bacteria appear as filamentous, highly reflective structures under IVCM, similar to many fungi. If you have a history of eye trauma involving organic matter, this information can help the doctor interpret the IVCM results correctly. However, the usefulness of IVCM highly depends on the expertise of the person using it.
There is more recent evidence that suggests newer techniques like the polymerase chain reaction (PCR), gene sequencing, and DNA sequencing are becoming more commonly used in detecting Nocardia bacteria from infected tissue.
Treatment Options for Nocardia Keratitis
Nocardia keratitis, an eye infection caused by the Nocardia bacteria, can be tricky to treat as it often doesn’t respond well to regular therapies for bacterial eye infections. A drug called amikacin, applied as eye drops, remains the main treatment. If your doctor suspects Nocardia keratitis, they usually start treatment with amikacin rather than waiting for test results to confirm the bacterial source, as this can take up to a week.
Oppositely, not all cases of Nocardia keratitis respond to amikacin. If this happens, other medications like tobramycin, gentamicin, imipenem, or moxifloxacin may be used. An older treatment, sulfonamides (trimethoprim-sulfamethoxazole), isn’t commonly used anymore because amikacin has proven more effective. Eye drops that contain corticosteroids should be avoided as they may increase chances of corneal perforation and endophthalmitis, complications that may damage the eye.
Nocardia can sometimes spread beyond the eye’s surface, leading to an eye condition called scleritis. If you’ve previously suffered eye trauma and now have symptoms of scleritis, this could be due to a Nocardia infection. Immediate surgical intervention is needed before confirmatory tests are done. Along with the usual topical treatment, an injection of amikacin into the skin surrounding the eye may be needed. If this doesn’t help, oral medication trimethoprim-sulfamethoxazole may be required.
In some cases, Nocardia keratitis may not respond to medication or may cause progressive thinning of the cornea or significant damage to the sclera. Here, surgical treatment may become necessary. Some surgical procedures include lamellar keratectomy, penetrating keratoplasty, and conjunctival flap, which could help remove infected tissue and increase the effectiveness of topical antibiotics. Though reports on surgical treatment for Nocardia keratitis are few, studies indicate that outcomes can be good.
What else can Nocardia Keratitis be?
Understanding the differences between Nocardia keratitis and similar conditions can be complex. Nocardia keratitis and fungal keratitis, for example, can both show clusters of infiltrates under a slit-lamp examination and have similar-looking structures in cultures. At times, Nocardia may even appear like cotton-wool infiltrates with irregular edges, which is more commonly seen in fungal keratitis. Even the characteristic “wreath-like” pattern found in Nocardia keratitis has been spotted in some cases of fungal keratitis. So, these two conditions can often be mistaken for one another.
What could help differentiate Nocardia keratitis from fungal keratitis is the patient’s history of trauma with organic matter, the longer time it takes for the infection to develop, and the granular look of the lesions under a slit-lamp examination.
- Moraxella, another bacteria that can mimic Nocardia, creates ulcers on the lower part of the cornea in specific groups of patients, such as those with diabetes, alcoholics, and malnourished people. While both Moraxella and Nocardia can grow on blood and chocolate agar, only Nocardia will show as Gram-positive and develop filamentous structures in culture. Unlike Nocardia, Moraxella keratitis usually affects the lower cornea and does not spread further.
- Mycobacteria, similar to Nocardia, are slow-progressing bacteria that cause corneal infections. Both will test positive with acid-fast (Ziehl-Neelsen) staining and can grow on blood agar. Still, Mycobacteria is more inclined to show white corneal infiltrates with a “snowflake” or “cracked windshield” appearance under a slit-lamp examination. Not like Nocardia though, Mycobacteria will also grow on Lowenstein-Jensen medium.
What to expect with Nocardia Keratitis
With the right treatment, an infection in the cornea (the clear layer at the front of the eye) caused by the bacteria Nocardia, can heal quickly. This healing usually leaves some scarring and extra blood vessels on the edges of the cornea. If the body responds well to the medicine, vision typically improves. Most patients don’t experience any symptoms and the infection doesn’t come back.
In one study, almost all patients saw an improvement in their vision equivalent to 20/25 once they were quickly diagnosed and treated. However, results can be less positive for older patients, and those where the infection has spread from the cornea to the sclera (the white part of the eye).
Possible Complications When Diagnosed with Nocardia Keratitis
If Nocardia keratitis, an infection in the cornea, isn’t diagnosed or treated well, it can spread to the nearby parts of the eye such as the sclera or the white of the eye. This can cause damage to the sclera (Nocardia scleritis) with symptoms like tissue death, bleeding, and abscesses. You may also notice the veins near the surface of the eye (episcleral veins) become enlarged. To treat this, parts of the damaged eye tissue may be removed, and a type of antibiotic called amikacin applied directly to the eye and surrounding tissues.
In very rare cases, Nocardia keratitis can also move deeper into the eye causing a severe infection known as endophthalmitis. This primarily happens due to the spread of bacteria from other infected parts of the body through the bloodstream in individuals with weakened immune systems. Symptoms of endophthalmitis include severe inflammation in the front part of the eye and accumulation of white blood cells that forms a layer in the eye. It may also present as yellowish-white bumps on the iris. Endophthalmitis due to Nocardia is often associated with grave outcomes, but if detected early and treated aggressively with topical and intravitreal (injected inside the eye) antibiotics, it’s possible to save vision.
No research reports are available on how frequently these complications occur due to Nocardia keratitis. However, any delay in treatment could result in serious conditions like the rupture of the cornea or even permanent blindness.
Common Side Effects:
- Damage to the sclera (white of the eye)
- Tissue death
- Bleeding
- Abscesses (pools of pus)
- Enlarged veins near the surface of the eye
- Severe infection deeper in the eye (endophthalmitis)
- Severe inflammation in the front of the eye
- Yellowish-white bumps on the iris
- Potential vision loss
- Rupture of the cornea
- Permanent blindness
Preventing Nocardia Keratitis
People who wear contact lenses need to be aware of how to properly take care of them and should not keep the lenses in their eyes for a prolonged period. If you spend a lot of time around dirt or plants, it’s a good idea to wear protective glasses when necessary to keep your eyes safe.












