What is Rotator Cuff Tendonitis?
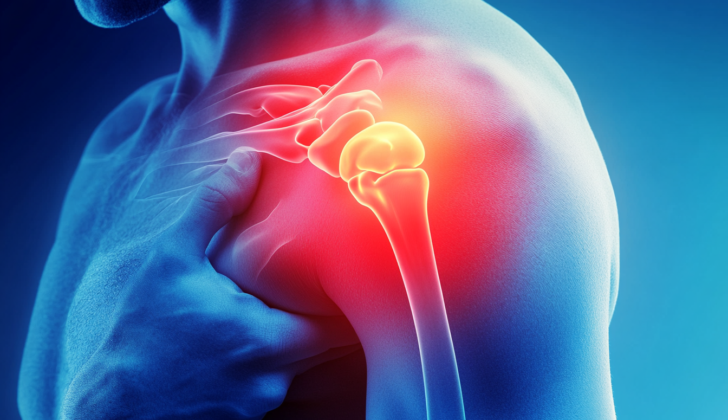
Damage to the rotator cuff, a group of muscles and tendons that stabilize the shoulder, can be simple bruises and inflammation (tendonitis) or more serious conditions like long-term tendon wear and tear (chronic tendinopathy), partial tears, and complete tears. The rotator cuff can be affected across all types of individuals, from casual exercisers to professional athletes, and across all age groups.
What Causes Rotator Cuff Tendonitis?
Subacromial impingement syndrome, which is a common cause of shoulder pain, often occurs with a condition called rotator cuff tendonitis. This condition can either appear suddenly after an injury or develop over time due to repetitive activities or sports-related demands.
Rotator cuff tendonitis often affects athletes and might happen due to a direct blow to the shoulder in contact sports, poor throwing techniques in sports like baseball or javelin, or from falling on an outstretched arm.
There are two main theories about why chronic rotator cuff tendonitis occurs:
– Extrinsic compression: This theory suggests that the injury occurs due to long-term pressure and friction between the part of your shoulder blade known as the acromion and the rotator cuff. This could be due to a wear and tear of the cushioning sac (bursa) in your shoulder, spur formation on the acromion, or certain shapes of the acromion.
– Intrinsic mechanisms: These theories suggest that the primary cause of shoulder impingement is the degeneration of the cuff itself that destabilizes the shoulder joint. Consequently, the head of the upper-arm bone moves upward, decreasing the space beneath the acromion, and making the cuff more susceptible to external pressure and damage.
The intrinsic mechanism theories also discuss the role of age-related blood circulation changes and the rotator cuff’s own wear and tear due to repetitive forces. It’s suggested that sections of the tendon lack proper blood supply, leading to an increased risk of injury. This becomes more pronounced with age, as the area with reduced blood supply becomes larger. However, other studies suggest these changes could be due to damage caused by external forces leading to blood vessel damage, cell death, and general deterioration and damage to the cuff.
It’s also worth noting that aging, sex, and genetics can cause changes in the rotator cuff, including disorganization of structural proteins like collagen and softer, gel-like changes. Studies show that the frequency of these changes—leading to rotator cuff abnormalities—increases with age, from around 5% to 10% in patients younger than 20 years, up to 60% to 65% in patients over 80 years of age.
Finally, a study suggested that the primary source of cuff damage comes from within the cuff itself as it endures significant stress during physical activity.
Risk Factors and Frequency for Rotator Cuff Tendonitis
Shoulder pain is the third most common reason for visiting the doctor for muscle or bone discomfort, coming after back and knee issues. It is responsible for 4.5 million doctor visits and costs around $3 billion each year, just in the United States. Almost 67% of people experience shoulder pain at some point in their lives. The most common reasons for shoulder pain are problems with the area below the top of the shoulder, known as subacromial impingement syndrome, and/or with the muscles in the shoulder, known as rotator cuff pathologies.
- Shoulder pain is a common reason for visiting the doctor, after spine and knee issues.
- It’s estimated to cause 4.5 million doctor visits and $3 billion in healthcare costs annually in the U.S.
- About two-thirds of people experience shoulder pain at some point in their lives.
- The main causes are issues in the part of the shoulder beneath the acromion (a bony projection on the shoulder blade) known as subacromial impingement syndrome, and problems with the group of muscles and their tendons in the shoulder, known as rotator cuff pathologies.
- The likelihood of sustaining a rotator cuff injury increases with age, with rates rising from 5% to 10% in people under 20 to over 60% in people over 80.
Signs and Symptoms of Rotator Cuff Tendonitis
When a doctor is examining a patient with shoulder pain, whether it’s been a long-standing issue or a recent development, they will take a detailed history. This may include details about the patient’s injury, any activities that make the pain worse such as lifting objects overhead, if the pain wakes them at night, and whether the patient participates in any sports or other physical activities. They will also ask about the patient’s job, which hand they use most often, if they have ever injured their shoulder or neck before, and if they’ve undergone any surgical procedures.
Doctors will also perform different physical examinations to help determine the cause of the shoulder pain. Some of the tests are designed to identify issues with the neck or cervical spine that could be contributing to the shoulder pain. They will examine the patient’s posture, test the range of motion in their neck, and may perform several specific tests such as the Spurling maneuver and reflex tests.
Additionally, they will also assess the patient’s shoulder in detail, looking for any visible abnormalities, feeling for tender areas, and testing both the active (patient moves themselves) and passive (doctor moves patient’s arm) range of motion. Certain types of pain and limitations in movement may point to specific problems, such as rotator cuff tendonitis.
The doctor will also test the strength of the patient’s muscles in their shoulder which can indicate issues with specific parts of the rotator cuff. There are certain examinations for each part of the rotator cuff:
- Supraspinatus: Doctors use Jobe’s test and the drop arm test.
- Infraspinatus: Tests strength and the external rotation lag sign.
- Teres Minor: Examines strength and Hornblower’s sign.
- Subscapularis: Uses the internal rotation lag sign and the lift-off test.
Moreover, other tests allow the doctor to examine the impingement or pinching of the muscles or tendons around the shoulder:
- External Impingement: Identified through Neer’s impingement sign and the Hawkins Test.
- Internal Impingement: Identified through the internal impingement test.
By taking a comprehensive history and performing these physical examinations, doctors can better diagnose and treat shoulder pain.
Testing for Rotator Cuff Tendonitis
If you’re experiencing acute (sudden or severe) or chronic (long-term) shoulder pain, it’s beneficial for your doctor to order imaging tests. Radiographs, also known as X-rays, are commonly recommended.
One type of x-ray is a true anteroposterior (AP) image of the glenohumeral joint, commonly referred to as the “Grashey” view. This is done by rotating you between 30 and 45 degrees against a cassette where your image will be captured. This x-ray allows your doctor to measure the distance between your acromion and the humeral head, known as the acromiohumeral interval. This interval is normally between 7 and 14 mm, and it can be smaller in cases of advanced arthritis and rotator cuff arthropathy (RCA) (a condition where you have shoulder pain due to a tear in the rotator cuff, the group of muscles and tendons surrounding the shoulder joint).
Additional X-rays can include a 30-degree tilted view that can reveal the presence of acromial spurring (bony growth on the acromion, the bony point of the shoulder characterising some forms of shoulder pain or discomfort). There’s also the “scapular Y” or “supraspinatus outlet” view used to evaluate the shape of your acromion.
Common findings from these x-ray views when you have rotator cuff problems can include:
– Rotator cuff arthropathy which results in the humeral head moving closer to the acromion, reducing the acromiohumeral interval to less than 7mm.
– Signs of wear and tear, such as outgrowths on the acromion, humerus or glenoid (the socket in your shoulder blade), calcification (hardening due to calcium deposits) of the shoulder ligaments, and arthritis in the acromioclavicular joint (the joint at the top of the shoulder).
– A “hooked” acromion or an Os acromiale, a condition where the acromion bone at the tip of the shoulder does not fully join, best seen on specific x-ray views.
Another diagnostic tool is ultrasound. This is effective at checking for any problems in the tendons (the tissues that connect muscles to bones) and muscles. A detailed review found it very reliable for diagnosing rotator cuff tears.
Finally, magnetic resonance imaging (MRI) is beneficial for assessing the overall state of your rotator cuff and can provide very specific details about any tears such as size and location. It can also identify other potential sources of your pain like inflammation of the bursa (fluid-filled sacs in the shoulder) or issues with the acromioclavicular joint and the long head of the biceps tendons. It’s essential for the radiologist to take into account the overall picture, including your symptoms and clinical examination, when interpreting these MRI findings.
Treatment Options for Rotator Cuff Tendonitis
Rotator cuff tendonitis is a complex condition, and we recommend different ways of treatment and management based on your particular circumstances:
Group 1:
This group includes patients with Partial-Thickness (PTT) or Full-Thickness (FTT) tears in their rotator cuff but without any symptoms. Essentially, these patients have damage in their rotator cuff but are not experiencing any pain or discomfort. Sometimes, this damage is found incidentally during shoulder MRIs. Although rotator cuff disease is more common in the aging population, surgical treatment does not always prevent further damage or symptoms. Hence, the current recommendation is to manage symptoms with non-surgical methods.
Group 2:
This category includes patients with PTT who are experiencing symptoms of external or subacromial impingement syndrome but do not have FTTs. These patients have pain from pressure or rubbing of their rotator cuff against the shoulder blade bone. These patients are first treated with non-surgical means. When to move to surgery depends on different factors like the patient’s symptoms, their response to non-surgical treatment, and their personal goals. This varies widely, from 3 months to 18 months.
Group 3:
This group includes those patients with chronic rotator cuff tears who are experiencing symptoms. The current guideline from the American Academy of Orthopaedic Surgeons (AAOS) is not firm due to limited evidence comparing surgical repair to non-surgical treatment in these patients. Hence, treatment should be personalized depending on each patient’s overall clinical picture.
Non-Surgical Treatments for Rotator Cuff Syndrome:
Physical therapy (PT) is considered as the first-line treatment option. This includes programs to strengthen the rotator cuff and stabilizer muscles around the shoulder blade and range-of-motion exercises.
Non-steroidal anti-inflammatory drugs (NSAIDs) are also used alongside PT to manage pain and inflammation. Cortisone injections into the space around the rotator cuff may provide immediate pain relief and enable the patient to participate in subsequent physical therapy sessions. However, these treatments are not always effective for everyone, especially in cases of FTTs.
Another aspect of treatment is rest and modifications to daily activities. This is especially important for those activities that caused the symptoms, such as repetitive overhead activity and heavy lifting.
Surgical Management:
If non-surgical treatment fails, your doctor might recommend surgery. These range from debridement (cleaning debris from the site), subacromial decompression (removing tissue or bone to make more space for the rotator cuff), or acromioplasty (resurfacing the underside of the acromion) to rotator cuff debridement and tear repair.
In subacromial decompression, the surgeon removes debris from the subacromial space which results in pain relief. An additional procedure, acromioplasty, involves shaving the underside of the acromion (part of the shoulder blade) to provide more space for the rotator cuff. In the case of an os acromiale – a condition where a part of the shoulder blade doesn’t fuse, causing instability – a two-stage procedure often occurs. This involves initially fusing the os acromiale with a bone grafting technique and then followed by acromioplasty after healing occurs.
These surgical options can be performed either through open surgery or arthroscopy (where small incisions are made and a camera is used to view and perform the procedure). Studies have shown that both methods are effective, but patients who undergo arthroscopic surgery may return to work quicker.
What else can Rotator Cuff Tendonitis be?
Chronic shoulder pain could be caused by a number of different conditions, as listed below:
- Impingement: this can be external/subacromial, subcoracoid, due to calcific tendonitis, or internal (including SLAP lesions, glenohumeral internal rotation deficit (GIRD), little League shoulder, posterior labral tears).
- Rotator Cuff (RC) Pathology: this could be tendonitis (acute), tendinopathy (chronic or acute on chronic), or involve partial- versus full-thickness tears and RC arthropathy.
- Degenerative Conditions: advanced joint disease often associated with RC arthropathy, glenohumeral arthritis, adhesive capsulitis, avascular necrosis (AVN), or scapulothoracic crepitus.
- Proximal Biceps issues: subluxation – often seen in association with subscapularis injuries, or tendonitis and tendinopathy.
- Acromioclavicular Joint Conditions – AC joint separation, distal clavicle osteolysis, AC joint arthritis.
- Instability – Unidirectional instability, seen in association with an event/dislocation (anterior, posterior, inferior), multidirectional instability (MDI), or associated labral injuries.
- Neurovascular Conditions: suprascapular neuropathy, scapular winging, brachial neuritis, thoracic outlet syndrome (TOS), or quadrilateral space syndrome.
- Other Conditions: scapulothoracic dyskinesia, os acromiale, muscle ruptures (pectoralis major, deltoid, latissimus dorsi), or possible fractures due to an acute injury or pain resulting from long-standing deformity.
What to expect with Rotator Cuff Tendonitis
Most people who have rotator cuff tendinopathy (a condition where the tendons in the shoulder become damaged or irritated) but do not have full-thickness tears, show improvement with non-surgical treatment. The American Academy of Orthopaedic Surgeons (AAOS) gives a “moderate” recommendation for the first line of treatment to be nonsteroidal anti-inflammatory drugs (NSAIDs) and/or exercise programs. This recommendation is based on numerous high-quality studies in the field.
Possible Complications When Diagnosed with Rotator Cuff Tendonitis
Rotator cuff syndrome can have complications tied to either not having surgery or having surgery.
When not treated with surgery, patients may continue to experience pain and recurring symptoms. For instance, with Partial Thickness Tears (PTTs), there’s a possibility of the tear getting worse, poor healing, fatty changes, muscle atrophy, and muscle retraction. In 2017, one study highlighted risk factors that could cause the tear to get worse in patients managed without surgery. These included the initial existence of a Full Thickness Tear (FTT), medium-sized tears (1 to 3 cm), and smoking habits. But, note that a PTT’s presence didn’t increase the risk of the rotator cuff tear worsening. When patients deal with chronic or atrophic tears, particularly with increasing rotator cuff tear, this can lead to degenerative joint disease and rotator cuff muscle group wasting.
For patients having surgery, treatments are most effective for those showing persistent or worsening symptoms despite at least 4-6 months of intensive nonsurgical treatment. However, surgery comes with risks, including recurring pain or symptoms, infection, stiffness, possible nerve or blood vessel damage, and risks related to the use of anesthesia. After a Subacromial decompression/acromioplasty surgery, there can be Deltoid muscle dysfunction, resulting from failed repatch after an open acromioplasty or excessive tissue removal during an arthroscopic procedure.
Another potential complication is Anterosuperior escape. This happens due to aggressive coracoacromial ligament release; the coracoacromial arch and its suspensory system could be compromised. When this happens in cases of large, retracted, and irreparable rotator cuff tears, the humeral head – the ball at the top of your upper arm bone – moves upward and forward, compromising patient functional outcomes.
List of Complications:
- Persistent pain/recurring symptoms
- Increasing rotator cuff tear, poor healing, fatty changes, muscle atrophy, and muscle retraction.
- Degenerative joint disease and rotator cuff muscle group wasting.
- Possibility of recurring pain or symptoms, infection, stiffness after surgery.
- Possible nerve or blood vessel damage.
- Risks related to the use of anesthesia.
- Deltoid muscle dysfunction.
- Unfavorable patient functional outcomes from Anterosuperior escape.
Recovery from Rotator Cuff Tendonitis
After a procedure known as subacromial decompression or acromioplasty (a surgery that does not involve repairing the rotator cuff), patients are typically required to wear a sling for 1 to 2 weeks. During this time, they will start gentle, passive motion exercises as part of their rehabilitation. However, doctors need to be aware of the risk of overusing the sling, especially if it’s not necessary for healing soft tissues.
Patients are initially advised to avoid any heavy lifting and intense exercises in order to let their tissues heal properly. Some might also be given cooling therapy devices, often used for the first 10-14 days after surgery. Once the sling is taken off, patients usually begin physical therapy.
The goal is for patients to regain their full range of motion between 3 to 6 weeks after surgery. Depending on individual progress, they could resume sport-specific skills around 6 to 8 weeks, as long as their body can handle it.
Preventing Rotator Cuff Tendonitis
It’s crucial for patients to understand their current health status as well as what to expect after surgical treatment for consistent shoulder discomfort, which is medically known as impingement or rotator cuff tendonitis. It’s vital for patients to understand that even after surgical intervention, they may still experience chronic pain.