What is Iatrogenic Pneumothorax (Collapsed Lung)?
A pneumothorax, or collapsed lung, is when air collects in the space between the lung and the chest wall. This can happen when air from the lung or from outside gets into this space. There are three ways this can happen: it can happen on its own (spontaneous), because of another condition (secondary), or because of a physical injury (traumatic). This article talks about a specific type of traumatic pneumothorax called ‘iatrogenic pneumothorax.’ This type happens because of a medical procedure like a lung biopsy, the placement of a central venous line, or the use of a breathing machine that provides positive pressure.
Sometimes, after such procedures, a tension pneumothorax can develop. This is a serious situation where the pressure in the space around the lungs becomes too high during all parts of the breathing process. This can reduce the amount of blood that returns to the heart, a situation called hypotension. It can also reduce the amount of oxygen getting to the tissues, known as hypoxia. A pneumothorax can have no symptoms at all, or it can be life-threateningly severe. Making sure not to cause a pneumothorax is an important patient safety consideration in the mentioned procedures.
What Causes Iatrogenic Pneumothorax (Collapsed Lung)?
An iatrogenic pneumothorax is a medical complication that can occur after certain medical procedures. The term “iatrogenic” means it’s caused by medical examination or treatment, and “pneumothorax” is when air enters the space between the lung and the chest wall, causing the lung to collapse.
This condition is often a known risk with invasive procedures like a lung biopsy, where a small piece of lung tissue is extracted for testing; the placement of a central venous line, which is a tube inserted into a large vein for administering medication or taking blood; or positive pressure ventilation, which is a type of breathing support.
Moreover, this condition can also happen after many other procedures involving the chest and abdomen. There have been instances where iatrogenic pneumothorax occurred after incorrect placement of a nebulization kit—a device used to deliver medication in the form of a mist that’s inhaled into the lungs—in a patient who was breathing on their own while intubated, or had a tube to assist with breathing. It’s also been reported after the insertion of a hypoglossal nerve stimulator, a device used to treat certain sleep disorders, and even after acupuncture, a form of traditional Chinese medicine.
That being said, the procedure most commonly associated with iatrogenic pneumothorax is subclavian insertion of a central venous line. This procedure involves inserting a tube into a vein located just below the collarbone to deliver medications or fluids, or to collect blood samples.
Risk Factors and Frequency for Iatrogenic Pneumothorax (Collapsed Lung)
An iatrogenic pneumothorax is a condition that can occur as a result of medical procedures. The chances of it happening increase with the number of invasive procedures a patient has. It’s more likely to happen in patients who are in serious condition due to trauma or emergency situations, because these patients often require invasive treatment. The risk also goes up when doctors have to use a different vein site because the internal jugular sites aren’t available.
Signs and Symptoms of Iatrogenic Pneumothorax (Collapsed Lung)
A pneumothorax, which is a collapsed lung, can cause symptoms that range from mild to severe, depending on the size and rate of development of the pneumothorax, as well as the patient’s overall lung health. Certain signs and symptoms, like sharp chest pain, shortness of breath, rapid breathing, and a rapid heart rate, can suggest a pneumothorax. A decrease or absence of sound when doctors listen to the affected side of your chest could also point to a pneumothorax. One type of this condition, called a tension pneumothorax, is especially serious, and can cause symptoms like low oxygen levels, low blood pressure, swollen neck veins, displaced windpipe, and decreased breath sound on one side.
- Sharp chest pain
- Shortness of breath
- Rapid breathing
- Rapid heart rate
- Decrease or absence of breath sounds on the affected side
- Low oxygen levels (in severe cases, like tension pneumothorax)
- Low blood pressure (in severe cases, like tension pneumothorax)
- Swollen neck veins (in severe cases, like tension pneumothorax)
- Displaced windpipe (in severe cases, like tension pneumothorax)
- Decreased breath sound on one side (in severe cases, like tension pneumothorax)
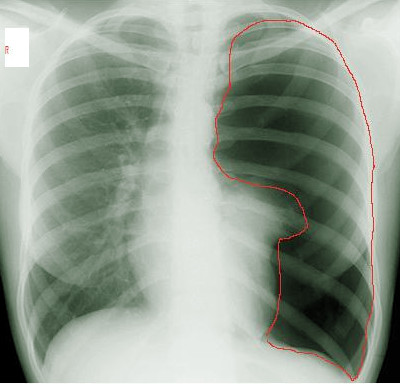
markings in the left pleural cavity (area marked with a red line), indicating
the presence of a pneumothorax. The collapsed lung is partially obscured by the
heart.
Testing for Iatrogenic Pneumothorax (Collapsed Lung)
An iatrogenic pneumothorax, a condition where air accumulates in the space around your lungs, is often diagnosed by looking at the symptoms you have. One helpful tool for doctors in diagnosing this condition is a point-of-care ultrasound. This method is quick, very precise (or ‘sensitive’), specific and can be performed multiple times if necessary.
The ultrasound may reveal a lack of ‘pleural sliding’, which means the two layers that enclose your lungs are not moving against one another as they should be. Another clue on ultrasound might be the ‘point sign’ which is when sliding and non-sliding areas of the pleura are seen side by side. This is a clear indicator of the condition.
X-rays (specifically upright posteroanterior chest radiography) are another way to detect a pneumothorax, with a success rate of about 83% in revealing the condition. See image labelled ‘Left Pneumothorax on X-ray’.
A chest CT scan can also help diagnose a pneumothorax – in fact, it’s more sensitive than an x-ray. However, it has the disadvantage of delaying treatment due to the time it takes to complete the scan. See image labelled ‘CT Scan, Pneumothorax’ for an example.
Treatment Options for Iatrogenic Pneumothorax (Collapsed Lung)
When diagnosing a pneumothorax (a collapsed lung), the first step is to determine if the patient is stable. To ensure the patient is getting enough oxygen, supplemental oxygen is given as needed. While some individuals with minor cases of collapsed lung may recover simply by being observed and undergoing periodic check-ups, more severe cases often require treatment.
Different treatments for a collapsed lung include needle aspiration, chest tube drainage, video-assisted thoracic surgery (or VATS, a type of minimally invasive surgery), and open surgical intervention. “Needle aspiration” involves inserting a needle into the space around the lungs to remove excess air. “Chest tube drainage” involves placing a tube in the chest to remove air. In more severe cases, one of the surgical methods might be needed to treat the condition.
Patient treatment should always take priority over imaging studies like X-rays or CT scans. If a patient is unstable, the first step is to provide immediate relief by performing needle decompression or aspiration, meaning a needle is placed in the chest to let out the excess air.
Another recently used technique is called finger thoracostomy. To perform this technique, a health care provider makes an incision in the chest, inserts a finger in, and uses it to guide the process of creating an opening to the outside. This procedure is carried out in a “safe triangle” on the chest wall, which is formed by the locations of different muscles and ribs. This procedure is considered quick and low-risk, since it does not cause an additional collapse and is suitable for patients with larger body sizes.
Thoracostomy is the definitive treatment. It uses a device that creates a water seal to generate negative pressure and remove the air, effectively re-inflating the lung. Chest tubes, used to drain air, can be placed in different areas of the chest depending on the specific circumstances of the patient and the pneumothorax.
Lastly, if conditions are severe enough, two surgical treatments are possible. Video-Assisted Thoracic Surgery (VATS) is a minimally invasive surgery, while an open surgical intervention involves more traditional surgical procedures. These are usually reserved as last-resort treatments for severe cases.
What else can Iatrogenic Pneumothorax (Collapsed Lung) be?
When someone comes in with chest pain, it’s important for doctors to consider many possibilities to make an exact diagnosis. The person might have a pneumothorax, which is a collapsed lung, but there are other medical conditions that could cause similar symptoms. These can include:
- Heart attack (myocardial infarct)
- Decreased blood flow to the heart (myocardial ischemia)
- Blocked blood vessel in the lungs (pulmonary embolus)
- Inflammation of the covering of the heart (pericarditis)
- Inflammation of the lining of the lungs and chest (pleurisy)
- Lung infection (pneumonia)
What to expect with Iatrogenic Pneumothorax (Collapsed Lung)
The chance of a pneumothorax, or a collapsed lung, happening again is estimated to range from 23% to 50% over a period of 1 to 5 years. The risk is highest during the first month. Unfortunately, there’s no information about how often this happens specifically due to medical procedures.
Patients who have had a tube thoracostomy, which is a medical procedure that drains air or fluid from around the lungs, can fly as soon as 72 hours after the tube is removed without any increased risk of the pneumothorax happening again.
Possible Complications When Diagnosed with Iatrogenic Pneumothorax (Collapsed Lung)
The biggest complication of any pneumothorax, which is a collapsed lung, is tension pneumothorax. This is a dangerous situation that is a threat to life and needs immediate treatment. Another major complication of pneumothorax is continuing air leaks and failure of the lung to reinflate properly, usually needing extra surgery for treatment.
Common Complications:
- Tension pneumothorax – life-threatening and requires immediate intervention
- Persistent air leak – this usually requires further surgical intervention
- Failure of lung re-expansion – this usually requires further surgical intervention
Preventing Iatrogenic Pneumothorax (Collapsed Lung)
A collapsed lung, or pneumothorax as it’s medically called, happens when air gathers in the space between your lung and chest wall. This can occur either because air has leaked from the lung or because air has entered from the outside. Sometimes, a lung can accidentally collapse during a medical procedure, which is known as an “iatrogenic pneumothorax”. Symptoms you might experience include sharp chest pain and difficulty in breathing. In some cases, if the air leak is tiny, you might not feel anything unusual.
This can be a serious condition needing immediate medical attention. The treatment primarily involves removing the trapped air from the space between your lung and chest wall. This could be accomplished with a needle, a scalpel, a finger, or a tube inserted into the chest. This tube remains in place until your lung has fully expanded back to its normal size. For more severe cases, surgery may be necessary. Even after successful treatment with a chest tube, it’s possible – although not likely – for the condition to happen again. As a precaution, those who have experienced a collapsed lung should avoid activities like scuba diving and plane travel for at least 72 hours.