What is Discoid Lupus Erythematosus?
Lupus erythematosus is a condition that largely impacts the skin and can show up in many different forms. The most commonly seen variants are acute cutaneous lupus (ACLE), subacute cutaneous lupus (SCLE), and discoid lupus (DLE). Dr. James Gilliam came up with a well-known method to categorize the skin changes seen in lupus erythematosus. He divided the skin changes into two groups, which he called specific and non-specific, based on whether certain skin inflammation was seen under microscopic examination. He further divides the ‘specific’ group into acute, subacute, and chronic forms.
Among the long-lasting, or chronic, types of lupus that primarily affect the skin, DLE is the most common. People with DLE may or may not experience sensitivity to light, but often their skin changes mainly appear on sun-exposed areas and usually result in thinning or scarring of the skin. Although most DLE patients don’t report significant impacts on their overall health, around 20% of them may show it as a sign of Systemic Lupus Erythematosus, which is a more widespread form of the disease. There are other, less common, variations of chronic skin lupus, including hypertrophic lupus, tumid lupus, lupus that affects the fat layers below the skin (also called lupus erythematosus panniculitis or lupus profundus), chilblain lupus, lupus that affects the mouth, along with lupus that causes skin changes on the palms and/or soles.
What Causes Discoid Lupus Erythematosus?
Lupus erythematosus is a disease that causes the body’s immune system to attack its own tissues, leading to inflammation. It’s a type of autoimmune disease where harmful antibodies are produced, reflecting an issue with the immune system’s tolerance. It primarily affects tissues connecting the various parts of the body.
There’s a kind of lupus called discoid lupus erythematosus that doesn’t connect to systemic lupus erythematosus (a commonly known type of lupus that affects multiple systems in the body). For this specific type of lupus, it’s not clear whether cells involved in immunity and self-attacking antibodies play a role in causing the disease. However, it’s clear that skin inflammation in discoid lupus erythematosus is dominated by a certain type of immune cell (Th1), in contrast to systemic lupus erythematosus, which involves another type of immune cell (Th17).
Risk Factors and Frequency for Discoid Lupus Erythematosus
Lupus is a disease that can affect people of all ages. However, a specific type of lupus known as Discoid Lupus Erythematosus (DLE) typically occurs more often in women in their 40s and 50s. Also, a quarter of people with Systemic Lupus Erythematosus (SLE) might get discoid lesions – a typical sign of DLE – at some point in their illness. Additionally, a small percentage (1%-5%) of people with discoid lupus might develop SLE.
Besides age and gender, race or ethnicity can also affect the risk of getting lupus. The effect of ethnicity on lupus rates is almost as significant as the effect of gender. Specifically, SLE is four times more common in African-American women than in white American women. Moreover, African-Americans generally get lupus at a younger age and unfortunately, have a higher mortality rate.
- Lupus can affect all age groups but DLE is more common in women in their 40s and 50s.
- About 25% of people with SLE may develop discoid lesions during their illness.
- Between 1% and 5% of people with discoid lupus may develop SLE.
- Your ethnicity can greatly affect your risk of developing lupus.
- African-American women are four times more likely than white American women to have SLE.
- African-Americans generally get lupus at a younger age and have a higher death rate.
Signs and Symptoms of Discoid Lupus Erythematosus
DLE, or Discoid Lupus Erythematosus, is a chronic skin condition. It most frequently appears in two forms. The first, making up about 80% of cases, is localized and shows up as lesions on the face, ears, and scalp. The second type, which is 20% of cases, is known as disseminated DLE and can have lesions both above and below the neck. This second type, particularly when it affects the trunk, can increase the chance of progression to Systemic Lupus Erythematosus (SLE) by up to 28%.
It’s not common for discoid lesions to appear below the neck without also appearing above the neck. Sometimes, discoid lesions can appear on the mucosal surfaces which include lips, nose, eyes, and genitals. The development of lesions seems to have an association with exposure to the sun, but they can also occur on sun-protected skin. There is no clear link between sun exposure and the development of these lesions.
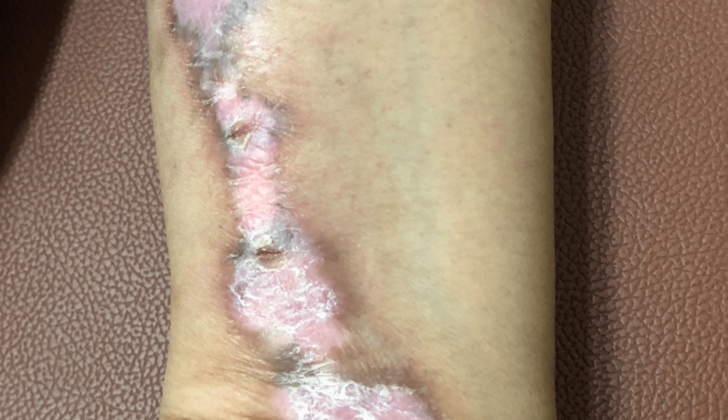
The initial sign of DLE is a distinctive round red patch or plaque of varying sizes. Then, the skin becomes hyperkeratotic, which means it thickens. When the thick layer is removed, there are tiny keratotic spikes that resemble carpet tacks, known as the “carpet tack sign”. The lesions slowly grow with inflammation and dark coloring around the edges, leading to central scarring, speckle-like blood vessels (telangiectasia), color loss, and a depressed central area. On the scalp, DLE can lead to permanent hair loss due to scarring. Although rare, these discoid lesions can turn into a specific type of skin cancer known as squamous cell carcinoma in 2-3% of cases, which typically has a poor outcome.
Patients with discoid lesions sometimes have joint pain. Over time, only about 10-20% of these patients fulfill the diagnostic criteria for SLE. The presence of wart-like, hyperkeratotic plaques is observed in the rare DLE subtype known as Hypertrophic DLE.
Testing for Discoid Lupus Erythematosus
When a doctor is evaluating a patient for discoid lupus erythematosus (DLE), they would ask about the patient’s medical history, and perform a skin examination to check for signs of any underlying systemic disease. The diagnosis of DLE is usually made based on the symptoms observed, but a tissue test may be needed to confirm it.
Patients with systemic lupus erythematosus (SLE), a type of lupus, commonly produce autoantibodies to various substances in their body, including SSA/Ro, SSB/La, U1RNP, histones, and ssDNA. However, these antibodies aren’t specific to any particular form of lupus, so other indicators are needed to differentiate the subtypes of cutaneous lupus erythematosus (CLE), a form of lupus that affects the skin.
One potential disease marker is annexin 1 autoantibodies. Annexin 1 is believed to help prevent autoimmune diseases. A recent study found that DLE patients tended to have a significantly higher level of anti-annexin 1 antibodies. This finding suggests these antibodies could potentially be used as a new diagnostic marker for DLE. However, there wasn’t a correlation found between the level of anti-annexin 1 antibodies in the blood and the severity of DLE symptoms.
Treatment Options for Discoid Lupus Erythematosus
Early intervention for discoid lupus, a chronic skin condition, can clear skin lesions. However, unsuccessful treatment can cause permanent scarring, hair loss, and changes in skin color, which can be particularly disfiguring for those with darker skin. To manage this condition, it’s advised that patients avoid sunlight, stop smoking and regularly apply sunscreen, as skin lesions can worsen with sun exposure. Also, smoking can increase the severity of the disease and could lead to less effectiveness of medications.
The first steps in treatment typically involve protecting the skin from the sun, along with the use of creams or injections that contain corticosteroids, and medicines that suppress parts of the body’s immune system. Topical corticosteroids are generally used to treat acute flare-ups of discoid lupus, with improvement usually seen within two weeks. Chronic use of these creams, however, can lead to skin thinning. Creams containing calcineurin inhibitors are also used, mostly for facial lesions, as it doesn’t cause skin thinning but can be more expensive and results may take longer to show.
If the skin doesn’t respond to these treatments, different injectable corticosteroids or topical calcineurin inhibitors should be used. If this fails, other treatments can be considered, including antimalarial drugs like hydroxychloroquine, which is the preferred first-line systemic therapy for this condition due to its low risk of side effects.
Alongside these treatments, retinoids, high doses of vitamin A with anti-keratinizing and anti-inflammatory effects, may be used, but there is limited evidence of their effectiveness. Other treatments, such as methotrexate and mycophenolate mofetil, can be used for more severe or stubborn cases of discoid lupus, usually when the condition is resistant to other treatments.
Thalidomide, a potent drug known to cause birth defects, has been used but typically reserved for severe cases due to its high risk of side effects. Lenalidomide, a similar drug, may also be effective but like thalidomide, patients tend to relapse once the drug is discontinued. Intravenous immune globulin (IVIG) is another treatment that can be used, although the treatment is expensive and the condition often recurs after treatment.
In sum, discoid lupus is a challenging condition to manage, but a variety of treatments are available and can be tailored to each patient’s individual needs to help manage this skin disease.
What else can Discoid Lupus Erythematosus be?
Diagnosing Discoid Lupus Erythematosus (DLE) is quite a challenge because it can look like other several diseases, like:
- Granuloma Faciale (a rare skin disease that causes red-brown, round skin lesions on the face)
- Tinea Faciei (a type of fungal infection on the face)
- Skin Tuberculosis (a bacterial infection that affects the skin)
- Cutaneous Leishmaniasis (a skin infection caused by a parasite)
- Lymphoproliferative disorders (a group of diseases that involves an overactive immune system)
- Sarcoidosis (a disease that causes cell clusters in different organs)
It gets especially tricky when DLE leaves scars on the scalp. It can look similar to other diseases like:
- Lichen Planopilaris (a type of hair loss disorder)
- Tinea Capitis (a scalp infection caused by a fungus)
- Central Centrifugal Cicatricial Alopecia (a common cause of scalp hair loss)
Moreover, a type of DLE that involves thicker skin changes can also look like other conditions such as:
- Keratoacanthoma (a fast-growing skin tumour)
- Squamous Cell Cancer (a type of skin cancer)
- Hypertrophic Lichen Planus (a rare skin condition causing thick, itchy, red patches)
- Prurigo Nodularis (a skin disease causing hard, itchy lumps)
It’s crucial that the doctor correctly identifies and rules out these similar conditions to ensure an accurate diagnosis of DLE.
What to expect with Discoid Lupus Erythematosus
DLE, or discoid lupus erythematosus, is a condition that causes skin lesions which may heal with symptoms like scarring, skin thinning, and changes in skin color. This can affect both physical wellbeing and mental health.
These lesions often get worse with sun exposure and are typically more severe in the spring and summer months. If DLE happens on the scalp, it can result in a type of baldness known as cicatricial alopecia.
There is a risk of about 28 percent that generalized DLE will develop into a more serious condition called systemic lupus erythematosus (SLE). In about 2 to 3 percent of cases, long-standing DLE lesions can transform into a type of skin cancer called squamous cell carcinoma, which often has a poor outlook.
However, if DLE is detected and treated early, it can help to minimize these adverse effects.

Possible Complications When Diagnosed with Discoid Lupus Erythematosus
DLE, which can develop into SLE, has been linked to a series of complications such as:
- Scarring hair loss
- Decrease in all types of blood cells
- Blood clots
- Joint inflammation
- Muscle inflammation
- High blood pressure
- Kidney failure
- Mental and emotional disorders such as seizures and depression
- Inflammation of the tissues that line the chest cavity and surround the heart
- Inflammation of the pancreas, inflammation of the small blood vessels in the digestive tract
- Inflammation of the optic nerve
- Side effects related to treatment
- Vitamin D deficiency
Regular monitoring of DLE lesions and potential side effects from treatment is very important to avoid complications and encourage resolution of symptoms.
Preventing Discoid Lupus Erythematosus
Doctors should educate their patients about protecting their skin from the sun and the possibility of developing skin lesions up to three weeks after sun exposure. Patients are advised to wear protective clothing and wide-brimmed hats, avoid sun exposure during the peak hours between 10:00 AM and 2:00 PM, and apply sunscreen generously. The sunscreen should have a sun protection factor of at least 30 and protect against both UVA and UVB sunlight. Patients should also avoid medicine that makes their skin more sensitive to the light and outdoor jobs with constant sun exposure.
As well as this, patients should stop smoking and avoid alcohol. Doctors should tell patients that nicotine can interfere with the uptake of their antimalarial medication and speed up its breakdown in the body – this explanation can help them understand why they should quit smoking. Ideally, they should quit smoking without using nicotine replacement therapy.
By avoiding the sun and using sunscreen, patients might not get enough Vitamin D. Therefore, doctors should suggest that they have yearly checks for vitamin D deficiency.