What is Inferior Alveolar Nerve and Lingual Nerve Injury?
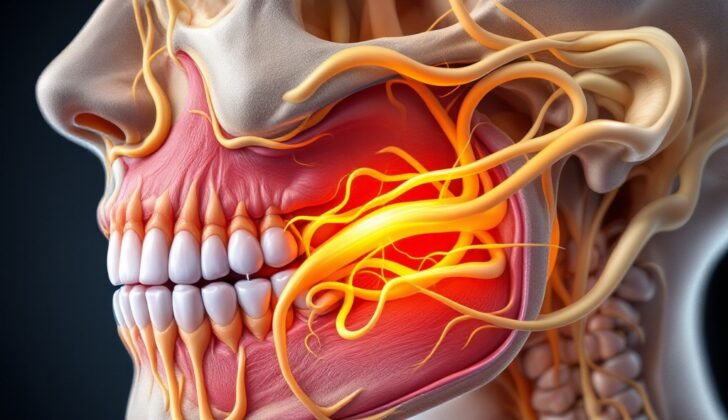
The inferior alveolar nerve (IAN) and the lingual nerve (LN) are offshoots of the third division of the trigeminal nerve, one of the key nerves in our face. The IAN is responsible for feeling in the chin, lower lip, the lower part of the gums, molars, premolars, and the bone that holds our teeth. The LN is responsible for sensation in the inner side of the gums and the front two-thirds of the tongue.
While it’s relatively rare, these nerves can be harmed during surgeries or procedures undertaken near the jaw or lower face. Certain types of jaw fractures and tumors can also damage these nerves. Patients with these injuries may feel considerable discomfort when performing everyday activities like chewing, eating, and talking. It’s important for health and dental professionals to identify and properly manage these injuries to reduce the chance of any permanent loss of sensation.
What Causes Inferior Alveolar Nerve and Lingual Nerve Injury?
To avoid harming certain nerves, it’s crucial to know about their positions in the body. Specifically, the mandibular branch (V3) of the trigeminal nerve is important. This nerve comes out of the skull and goes into a hollow space in our jawbone, where it divides into two more nerves – the inferior alveolar nerve (IAN) and lingual nerve (LN). The IAN goes into a hole in the jawbone and is responsible for sensation in the bottom teeth, surrounding gums, and skin of the chin and lower lip.
The LN, on the other hand, travels downwards between the jawbone and muscle on the inside of the jaw. It moves forward near the crest of the jawbone and once it has gone beyond the area behind the molars, it continues forward, along the side of the hyoglossus muscle, and beneath the mylohyoid muscle. The LN is responsible for sensations on the gums and the front two-thirds of the tongue. It’s also important to know that another nerve that gives us our sense of taste, called the chorda tympani nerve, hooks up with the LN near a muscle in the cheek. Any damage to the LN might also hurt the chorda tympani nerve, affecting taste and sensation.
Local anesthesia, a medication to numb feeling in a specific area, is often given before surgeries. But, both the IAN and LN could potentially be harmed during efforts to create numbness around them. Although rather uncommon, the needle or anesthesia itself could directly or indirectly damage the nerve. The risk goes up when anesthetizing the IAN as the needle travels very close to both the IAN and LN, near the jawbone. There are several theories as to how nerves might get damaged in such cases:
1. The needle might directly harm the nerve, causing damage to nerve cells.
2. The needle might harm small blood vessels around the nerve, causing a small blood clot that puts pressure on the nerve or leads to scarring.
3. The chemicals from the numbness medication might harm tissues while being broken down in the body.
Another reason for IAN and LN injuries is tooth extraction, especially the removal of a wisdom tooth. During the process, nerves might be injured by surgical tools, or pieces of tooth. The LN can also be hurt by surgical cuts or by being pulled too hard or stitched up too tightly. In addition, jawbone surgery sometimes fractures the mandible and may harm the IAN by exposing or touching the nerve in its canal.
Other causes of these nerve injuries include jaw fractures due to accidents or fights, and dental implant placement. The IAN might get harmed directly or from heat during the drilling process. Root canal treatment can also result in nerve damage due to excessive use of tools and chemicals during the procedure.
Risk Factors and Frequency for Inferior Alveolar Nerve and Lingual Nerve Injury
Injury to the inferior alveolar nerve (IAN) and lingual nerve (LN) can happen for various reasons, and the frequency of these incidents varies widely. Injuries related to local anesthetic injections are rare, and patients usually regain their nerve function independently 85-94% of the time.
Removal of the lower third molar (wisdom tooth) is the top surgical reason for IAN and LN injury. However, the rates change depending on the surgeon’s expertise and method.
- A 2012 study reported that these injuries occurred in 0.4 to 13.4% of cases for IAN and 0 to 11% of cases for LN after third molar extractions.
- Continuous IAN dysfunction was present in 0 to 1.6% of patients.
- For LN cases, most healed, but 0.5-0.6% continued to have issues.
In dental implant surgery, temporary nerve damage can happen in 0 to 24% of cases, and long-lasting injuries occur in 0 to 11% of situations.
In a different form of jaw surgery (mandibular orthognathic surgery), nerve injuries vary significantly. A study reviewing 20 years of procedures reported a 20-98% chance of IAN injury, with a 0 to 82% chance of long-lasting issues.
IAN injuries are also caused by non-surgical events. For example, jaw fractures can lead to IAN damage in 46 to 81% of cases. This rate however increases to 77 to 91% if treatment includes surgery to align and fix the broken bone, with permanent issues showing up in 0 to 45% of these patients.
Signs and Symptoms of Inferior Alveolar Nerve and Lingual Nerve Injury
People with IAN (Inferior alveolar nerve) and/or LN (Lingual nerve) injuries often report changes in their senses. Common complaints include feeling different in the areas of the lower lip, chin, lower teeth, gums, and tongue. Particularly with LN injuries, people might notice changes in their sense of taste on one side of the front of the tongue due to damage to a nerve called the chorda tympani. Despite this, the movement of the tongue and lower face should still be normal because different nerves control these areas. However, changes in the sensation can affect daily tasks such as talking, eating, drinking, kissing, putting on makeup, and shaving.
The type and range of these changed sensations can greatly vary from person to person. People might feel paresthesias, which are odd but not necessarily bad sensations like pins and needles. Changes can also fall into hypoesthesia (a reduction in sensation) or anesthesia (a total loss of sensation), which can make people feel like the affected area is paralyzed, but seeing the area move in a mirror can correct this mistaken belief. On the other hand, dysesthesia is a painful or unpleasant sensation, and it includes conditions like hyperalgesia (increased sensitivity to pain), hyperpathia (pain due to repeated stimuli), anesthesia dolorosa (pain in an area that lacks sensation), and allodynia (painful response to stimuli that are usually not painful).
Testing for Inferior Alveolar Nerve and Lingual Nerve Injury
If you have injuries to your trigeminal (IAN) or lingual nerves (LN), your doctor will use a combination of methods to understand how you’re feeling and to measure any loss of sensation. Because each person experiences sensation differently, it’s important to keep track of your personal experience over time. Your doctor will ask about your pain and use surveys to measure your progress.
Objective tests can also help your doctor understand the impact of the nerve injury. These tests focus on two areas: feeling everyday touch, like a light brush, or response to pain or heat, through a pinprick or temperature test. All results will be carefully recorded for comparison over time.
Each test is connected to different types of nerve fibers, which transmit different types of sensations. For example, the light touch test uses a soft cotton or filament and checks the health of A-beta fibers. The brush test checks the nerves that feel vibration and light touch (A-alpha and A-beta fibers), and a pointy object is used to ask if you feel a single point or two separate points. The pinprick test checks the nerves that feel sharp pain (A-delta and C fibers), and a temperature test checks the nerves that register warm and cold feelings.
There isn’t a single perfect method to test the injuries of these nerves, but a common grading system classifies nerve injuries based on the test results. This system groups the nerve fibers into three levels (A, B, and C) based on which type of sensation they carry.
If you have no change in sensation, your nerves work correctly. If you fail level A tests (touch and vibration) but pass levels B (touch) and C (pain), you have a mild injury and can expect to fully recover. If you fail level A and B tests but pass level C tests, you have a moderate injury, and partial or complete recovery is possible. If you fail all the tests, your nerve is severely injured, and full recovery might not be possible.
The doctor generally starts testing with level A, progresses to level B, and finally conducts level C tests.
Treatment Options for Inferior Alveolar Nerve and Lingual Nerve Injury
To help lower the chance of injuring the Inferior Alveolar Nerve (IAN) and Lingual Nerve (LN), which are critical nerves during mouth or lower face procedures, doctors need to have a good understanding of nerve location and how they connect. However, even with the best-prepared safeguards, there can still be an accidental injury to these nerves. As such, it is crucial for doctors to communicate the risks and benefits of undergoing procedures that involve the lower face or mouth. In case of an IAN or LN injury, the extent of damage can be assessed through nerve testing. However, there is no universally accepted method for managing IAN and LN injuries, as treatment strategies can differ depending on the doctor’s experience and comfort level.
Some common treatment options for IAN and LN nerve injuries include the following:
Non-surgical treatments
* Corticosteroids: These are medications that can immediately be given after nerve injury to decrease swelling and potentially lessen nerve damage. However, there isn’t strong evidence supporting the effectiveness of corticosteroids in preventing nerve deficits, but they are commonly used in brain surgeries and have shown improvements in facial nerve paralysis.
* Topical medications: For patients suffering from pain due to nerve injury, certain medications can be applied onto the skin to provide relief. Capsaicin, lidocaine, clonidine, and clonazepam are some common examples.
* Systemic Pharmacologic agents: Oral medications, such as antidepressants, anti-seizure drugs, lidocaine-related drugs, and muscle relaxants, can also be used to alleviate pain from nerve injury.
Surgical treatments
* External nerve decompression: Surgical intervention should be considered if there’s no improvement in nerve function after three months, and the nerve damage is unbearable for the patient. If the nerve damage is suspected to be caused by compression, releasing or removing surrounding structures might help alleviate pressure on the nerve.
Studies have reported an 85% rate of sensory recovery after decompression, and it may lead to faster recovery than other nerve repair treatments.
* Direct Neurorrhaphy: If a nerve is severed, it may be sewn back together if the nerve ends can meet without tension. The likelihood of restoring sensation varies widely but may be as high as 90% under ideal circumstances.
* Nerve sleeve: If the severed nerve ends can’t be joined together without strain, a collagen sleeve (a sort of protective cover) can be used to stimulate nerve regeneration. This method has a success rate of over 80%, especially when the gap between the severed nerve ends is 3 mm or less.
* Nerve Reconstruction with autogenous grafts: When an injury results in a gap larger than 3 mm, nerve or vein grafts can be used to bridge the gap. Sensory recovery rates are notably higher when nerves (87.3%) are used compared to veins (60%).
* Removal of the cause : If a foreign object is causing nerve dysfunction, it should be removed to limit inflammation and speed up recovery. For instance, if a dental implant is causing damage to the lower jaw nerve, the implant needs to be removed ideally within 36 hours of placement.
What else can Inferior Alveolar Nerve and Lingual Nerve Injury be?
While it’s less common than injuries caused by medical procedures or accidents, certain medical conditions can also affect the sensation of the trigeminal nerve, which can mimic the signs of injuries to the Inferior Alveolar Nerve (IAN) and the Lingual Nerve (LN). These conditions can include:
- Both benign (non-cancerous) and malignant (cancerous) tumors that affect the trigeminal nerve
- Autoimmune disorders like lupus, dermatomyositis, progressive sclerosis, Sjögren’s syndrome, rheumatoid arthritis, among other conditions affecting connective tissue
- Infections caused by viruses or bacteria such as herpes zoster, herpes simplex, syphilis, or leprosy
- Multiple sclerosis
- Vertebrobasilar disease, a condition that affects the blood vessels at the back of the brain
- Sarcoidosis, a disease that causes inflammation around the body’s organs
- Amyloidosis, a disorder that results in the production of abnormal protein, called amyloid
- Sickle cell anemia, an inherited condition characterized by irregular red blood cells
What to expect with Inferior Alveolar Nerve and Lingual Nerve Injury
The best-case scenario is to identify an injury to the inferior alveolar nerve (IAN) or lingual nerve (LN), which help with feeling and taste in the mouth, right when it happens. This would allow for an immediate fix, increasing the chances of regaining normal sensation. If the injury is not noticed until after the surgery, the chances of naturally getting better lessen, especially if there’s no improvement within the first three months. In such instances, more surgery may be needed to help recovery.
However, it’s not entirely clear when the best time would be to repair a nerve injured during a procedure, if it’s only discovered after the procedure was completed. The chances of regaining full sensory function after surgical repair of an IAN or LN injury can vary. But a review of studies carried out in 2021 found that earlier repairs tend to result in better recovery.
In an ideal world, the injured nerve would be repaired within 3 to 6 months of getting injured because the chances of a successful repair can decrease for injuries that are older than nine months by the time they’re fixed.
Possible Complications When Diagnosed with Inferior Alveolar Nerve and Lingual Nerve Injury
The primary problems that come from injuries to the IAN (Inferior Alveolar Nerve) and LN (Lingual Nerve) are ongoing or worsening issues with sensation. When these nerves aren’t working correctly, it can lead to uncomfortableness or frustration during everyday tasks, like biting your lip or tongue and drooling. More severe injuries might not get better on their own and may need surgery, which carries its own set of risks.
Common Problems:
- Persistent or worsening sensory issues
- Discomfort during daily activities like biting the lip or tongue
- Drooling
- The requirement of surgery for severe injuries
- The risks that come with surgical intervention
Preventing Inferior Alveolar Nerve and Lingual Nerve Injury
Damage to the inferior alveolar nerve or lingual nerve, nerves found in your mouth and face, is uncommon but can occur as a result of various dental and facial surgeries. Doctors need to know what factors could increase the risk of nerve damage. These factors might include complex facial structures or a history of previous surgeries. They will factor in these risks when deciding if a surgery on the lower face is safe and when choosing the best surgical techniques.
Besides, it’s really important for doctors to discuss with patients about potential risks, including nerve damage, and other consequences that may occur after surgery. This way, both the patient and doctor can make informed decisions together about the treatment plan.