What is Tarsal Tunnel Syndrome?
Tarsal tunnel syndrome (TTS), also known as “tibial nerve dysfunction” or “posterior tibial nerve neuralgia,” is a condition caused by pressure on certain structures, especially the posterior tibial nerve, within the tarsal tunnel in your foot. This is similar to carpal tunnel syndrome in the wrist, where severe, rubber band-like pressure on the nerve causes pain and discomfort. Although, TTS is much rarer than its wrist counterpart. The condition is usually diagnosed based on the symptoms, but sometimes medical tests can help identify what is causing the compression and rule out other serious conditions.
Let’s break down the tarsal tunnel’s structure for you. Think of the tarsal tunnel as a small, tight space on the inside of your ankle. It has a hard floor made of the bones of your foot (the tibia, talus, and calcaneus), and a soft roof made of a band of tissue (the flexor retinaculum) stretched from your ankle bone to the heel.
This tight tunnel contains several important structures, including certain tendons (tibialis posterior, flexor digitorum longus or FDL, and flexor hallucis longus or FHL), the posterior tibial artery and vein for blood flow, and a nerve that runs from the lower back to the foot (the posterior tibial nerve). The arrangement of these structures in the space is quite unique. The tendons, artery, vein, and nerve all lay next to each other in a specific order from inside to outside and from front to back of the ankle.
The posterior tibial nerve splits into the medial and lateral plantar nerves within this tunnel. In some people (around 5%), this split happens before the nerve enters the tunnel. These nerves play different roles in sensation and movement in your foot, like feeling the inside of your foot or moving your toes.
Another nerve, the medial calcaneal nerve, usually branches off from the posterior tibial nerve before it enters the tunnel, and it provides sensation to the inner side of your heel. In about 25% of people, this nerve takes a different path, either branching off the lateral plantar nerve or running on top of the tissue forming the roof of the tarsal tunnel.
What Causes Tarsal Tunnel Syndrome?
The causes for TTS, or Tarsal Tunnel Syndrome, can be divided into two categories: intrinsic and extrinsic.
Intrinsic causes are related to certain abnormalities in the tarsal tunnel region, which is the part of the ankle that carries nerves and tendons from your leg into your foot. These abnormalities can include inflammation or damage to tendons (tendinopathy), inflammation of the protective sheath around tendons (tenosynovitis), overgrowth of fibrous tissue around nerves (perineural fibrosis), and certain bone deformities (osteophytes). Other structures that can take up too much space in the tunnel like enlarged veins (varicose veins), fluid-filled sacs (ganglion cysts), fat tissue (lipomas), tumors (neoplasms), and nerve tumors (neuromas) can also cause TTS.
Meanwhile, extrinsic causes are outside, or related to general conditions affecting the tarsal tunnel. These can include wearing shoes that don’t fit well, injuries, foot or ankle deformities (like “tarsal coalition” when bones in the foot join together, or “valgus” or “varus” when the foot twists at the ankle), swelling in the lower leg, arthritis related inflammation, diabetes, and scar tissue after surgery.
In about 80% of TTS cases, the trigger can be identified. TTS without any known cause is rare. Also, lack of proper blood supply, or arterial insufficiency, can lead to a state of blood shortage (nerve ischemia) in the affected area.
Risk Factors and Frequency for Tarsal Tunnel Syndrome
Takotsubo syndrome (TTS) is a fairly uncommon condition and it’s often not diagnosed correctly making it hard for us to know exactly how often it happens. What we do know is that it’s more common in females than males and it can occur at any age.
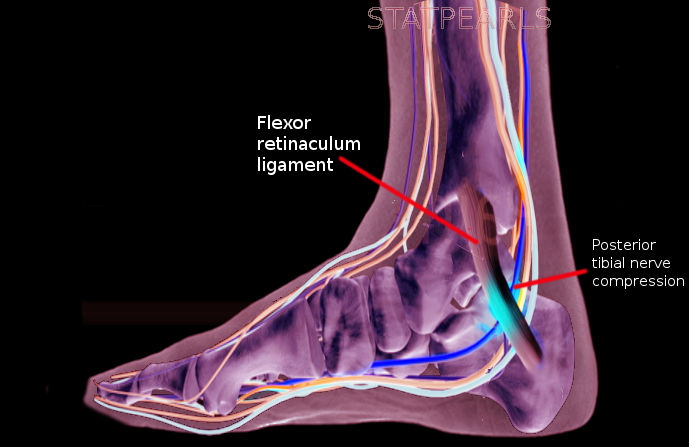
compression against a confined bony space by the flexor retinaculum.
Signs and Symptoms of Tarsal Tunnel Syndrome
Tarsal Tunnel Syndrome (TTS) is a condition that often causes foot pain and discomfort. Patients typically complain of pain over the tarsal tunnel, which goes to the arch and bottom of the foot. This pain can sometimes extend up to the calf or higher.
- Sharp, shooting foot pain
- Numbness on the bottom of the foot
- Pain that radiates along the path of the posterior tibial nerve
- Pain when the foot is flexed or turned out
- Tingling or burning sensation
- Symptoms may worsen with physical activity, standing, or walking and improve with rest
- Weakness in the foot muscles
- Different types of discomfort that can disrupt sleep
During the physical examination, the doctor may note specific foot shapes, such as flat feet, pronated foot, or club foot. Chronic cases of TTS might show signs of muscle atrophy, foot muscle weakness, and toes bending at unusual angles. How the patient walks can also be a clue: look for excessive pronation or supination, toe inversion, odd foot movements, or pain-induced limping. Massaging deeply on the tarsal tunnel might cause tenderness.
They might test the patient’s light touch and two-point discrimination abilities for the foot’s bottom areas. Weaknesses in these areas might be a sign of TTS. However, this usually comes at a later stage.
One diagnostic method is the Tinel test, where the doctor taps on the tarsal tunnel. A positive result triggering pain or tingling can suggest surgical relief might be needed. However, this test doesn’t always detect TTS, and when it does, it’s often a late-stage sign.
Another beneficial test is the dorsiflexion-eversion test, where the doctor flexes and turns the ankle outward until it can’t go further and holds it for 10 seconds. If this reproduces the patient’s symptoms, it is most likely TTS.
The TTS severity can be scored with the TTS severity rating scale. A score of 10 is normal, while 0 indicates maximum severity. This score is based on certain symptoms and their severity.
- Spontaneous pain or pain with movement
- Burning pain
- Tinel sign
- Sensory disturbances
- Muscle atrophy or weakness
If a patient’s symptoms are unclear, this scale may not be adequate for a full evaluation. If a clinical assessment isn’t sufficient to distinguish TTS from other severe foot conditions, more tests may be needed.
Testing for Tarsal Tunnel Syndrome
: Testing for Tarsal Tunnel Syndrome (TTS), a foot condition that causes pain, isn’t straightforward. There isn’t a specific test to diagnose it, so doctors often have to determine whether you have it based on your symptoms and physical examination. However, there are imaging and certain nerve-function studies that can help your doctor determine if other conditions are causing your symptoms or contribute to their understanding of your condition.
The first test your doctor might use is an X-ray of your ankle and foot. This can help identify physical changes or injuries, such as abnormal bone growth (osteophytes), misalignment of the heel (hindfoot varus or valgus), abnormal connection between bones in the foot (tarsal coalition), or signs of a past trauma.
You might also receive a Magnetic Resonance Imaging (MRI) scan, which uses a strong magnetic field to create detailed images of your body. This isn’t usually used to directly diagnose TTS because it’s not very sensitive to the condition. However, it can help rule out other potential causes of your symptoms by providing a detailed picture of your foot’s structure.
Ultrasound imaging is another tool your doctor might use. This test uses sound waves to create a real-time image of the structures in your foot. It allows your doctor to see structures like the posterior tibial nerve (the nerve affected in TTS) and any branches coming off it. Both ultrasound and MRI can show other issues with your foot’s soft tissues, such as inflammation, growths, unusual veins, or cysts.
Finally, your doctor might suggest nerve conduction studies or electromyography. Both tests evaluate how well your nerves are transmitting signals. Although these tests can sometimes detect problems in patients with TTS, the results are not always accurate. This means that, even if the tests come back normal, you could still have TTS. So, while these tests can provide useful information, a diagnosis of TTS is usually based on your symptoms and a physical examination.
Treatment Options for Tarsal Tunnel Syndrome
Managing Tarsal Tunnel Syndrome (TTS), a condition that causes pain and numbness in the foot and ankle, can be quite complicated due to the difficulty in diagnosing it and in figuring out which patients would benefit from different treatments. Treatments can consist of conservative (non-surgical) approaches or might require surgery. The choice of treatment usually depends on the root cause of the problem, how much the foot and ankle are affected, and if there is any muscle wasting.
Non-surgical treatment success can depend on what exactly is causing the symptoms. The aim is to lessen pain and inflammation, and to relieve stress on the tissue. This can be achieved using ice to reduce inflammation and pain. Painkillers that don’t contain opioids, such as acetaminophen and anti-inflammatory drugs, can be helpful. Some medications tailor-made for nerve pain like gabapentin, pregabalin, and certain antidepressants might be trialed. Topical treatments, ones you apply directly to the skin, with lidocaine or anti-inflammatory drugs can give some relief to the symptoms. Administering cortisone, a steroid, as an injection can also be done for pain relief and to help diagnose the condition.
Physical therapy can be beneficial in regaining foot and ankle functionality. This could include methods like ultrasound, iontophoresis, phonophoresis, and electrical stimulation to the soft tissue. Strengthening the muscles of the foot and using kinesiology tape can enhance foot stability by supporting the arch of the foot and lowering stress in that area. Modifying physical activities, calf stretching exercises, and techniques to enhance nerve mobility or gliding can contribute to symptom relief.
Specialty shoes that correct biomechanical abnormalities and reduce pressure on the tarsal tunnel (the area affected in TTS) can be used. Medial heel wedges or seats can lessen nerve traction by turning the heel inwards. Night splints, certain types of walkers or walking boots might be beneficial. Shoes with good arch support can help decrease symptoms. If other non-surgical treatments have not worked, the patient might temporarily need to wear a walking boot.
In some cases, fluid-filled lumps known as ganglion cysts can be drained with the help of ultrasound. Injecting cortisone into the tarsal tunnel might decrease swelling. Surgery might be required if pain and other symptoms continue despite non-surgical treatments, or if a clear cause of nerve entrapment is found, such as a space-occupying lesion. Patients whose symptoms are caused by these types of lesions generally respond well to surgical treatment. Alternatively, if nerve conduction across the posterior tibial nerve (one of the nerves at the back of the foot) is uncharacteristically slow, non-surgical treatment might not be effective.
Surgery for TTS involves removing part of the flexor retinaculum, a band of tissue in the foot near the ankle, from its attachment point near the medial malleolus (the bony bump on the inside of the ankle) downwards. Success rates for this type of surgery range from 44% to 96%. Patients who beforehand showed a positive Tinel sign (a tingling sensation when the affected nerve is tapped) generally have a better response to surgery for decompression than those who did not. Those who are younger, have a shorter history of symptoms, were diagnosed earlier, have a well-defined root cause, and had no previous problems with their ankles also generally respond well to surgery.
What else can Tarsal Tunnel Syndrome be?
For those struggling with TTS, or tarsal tunnel syndrome, it’s essential to get a clear diagnosis. This is because several other conditions can mimic TTS. So, doctors need to carefully consider these possibilities and run suitable tests to confirm the diagnosis. These conditions include:
- Achilles tendonitis
- Deep flexor compartment syndrome
- Age-related changes, such as heel bone spurs or foot joint disorders
- Inflammatory issues affecting foot and ankle ligaments and fascia (connective tissue)
- Complex overlap phenomenon of the FHL and FDL at the knot of Henry (muscles and tendons in the foot)
- Pinch or pressure on the nerves in the lower back (L5 and S1 nerve root compression)
- Morton’s metatarsalgia, a painful foot condition affecting the ball of your foot
- Neurogenic intermittent claudication, a symptom of lumbar spinal stenosis where one feels discomfort or pain in their legs due to prolonged standing or walking
- Plantar fasciitis, an inflammation of the ligament running under the sole of the foot
- Polyneuropathy, a nerve disorder causing weakness, numbness, and pain usually in hands and feet
- Retrocalcaneal bursitis, inflammation of the bursa located between the Achilles tendon and the heel bone
What to expect with Tarsal Tunnel Syndrome
The future outcomes for patients with TTS (Tarsal Tunnel Syndrome) can vary a lot. Usually, patients who have a known cause for their TTS and get diagnosed early in their disease are likely to respond well to treatment. If there’s no known reason for the TTS or if treatments like rest, ice, and medication don’t work, these patients often have worse results, even with surgery. A positive Tinel’s sign, which is a tingling sensation when the doctor taps over the affected nerve, can be a good indicator that surgery would provide relief.
Possible Complications When Diagnosed with Tarsal Tunnel Syndrome
If Tarsal Tunnel Syndrome (TTS) is not treated or if treatment doesn’t work, it can cause damage to the nerve on the back of the lower leg and its branches. This can lead to ongoing pain and the muscles might become weak and start to waste away. After surgery, complications may arise such as slow wound healing, infection, and scarring. Even after surgical relief of pressure in the tunnel, pain and other symptoms may not disappear fully.
Common Consequences:
- Damage to the nerve on the back of the lower leg and its branches
- Constant pain
- Muscle weakness
- Muscle wasting
- Slow wound healing after surgery
- Infections
- Scarring
- Persistent symptoms even after surgical pressure relief
Recovery from Tarsal Tunnel Syndrome
Rehabilitation after surgery helps safeguard the health of your joints and nerves, while also managing issues like inflammation, pain, and swelling. As you continue with your rehab exercises, both you and your therapist will focus on preventing the increase of dense scar tissue and sticky adhesions, while keeping your joints and soft tissues flexible and moving. The ultimate long-term goals are to get you back to your normal stride, be able to walk comfortably, and eventually to run as you used to.
Preventing Tarsal Tunnel Syndrome
There are no specific rules to prevent a condition known as Tarsal Tunnel Syndrome (TTS), but here are some general tips that can help:
* Use shoes that fit well and provide correct support to your feet.
* Try to limit standing or walking for a long time.
* Keep your body weight in a healthy range.
* Always make sure to warm up and stretch before you exercise or play sports.
* Work on strengthening your foot muscles.
* Rest your feet and ankles regularly to avoid overworking them.
* Make sure your workspace is designed in a way that minimizes stress on your legs and feet.
* Work on maintaining a healthy alignment of your feet when standing or walking.
It’s important to note that foot and ankle pain can have many causes, and not all of them are common. Tarsal Tunnel Syndrome is one of these lesser-known causes. If you start to feel pain in your foot or ankle and also experience symptoms like burning, numbness, tingling, and weakness in your muscles, you should seek immediate medical attention.












