What is Ulnar Nerve Entrapment?
Ulnar nerve entrapment usually happens either at the elbow, in what is known as the cubital tunnel, or at the wrist, in the ulnar tunnel. The symptoms a patient experiences depend on where the nerve is being compressed. For a better understanding of these symptoms, it’s important to know about the ulnar nerve’s structure and location.
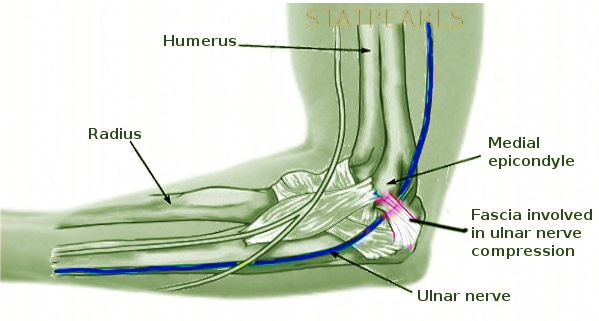
The ulnar nerve continues from the inner part of the bundle of nerves in your upper arm (medial cord of the brachial plexus). It’s located behind and toward the middle of the main artery in your arm (brachial artery). The nerve penetrates through the tissue separating muscles in the arm at a place known as the arcade of Struthers, about 8 cm above the bony point of the elbow (medial epicondyle). From there, it runs behind the elbow’s inner bump (medial epicondyle) and enters the forearm through an area called the cubital tunnel. This tunnel is a space bordered by certain ligaments. The most common cause of compression in this area is usually due to pressure from Osborne’s ligament.
In the forearm, the ulnar nerve passes between two muscles responsible for bending the wrist and fingers. It provides movement to these muscles, allowing us to bend the smallest two fingers at the farthest joint.
At the wrist, the ulnar nerve, along with the ulnar artery, enters an area known as Guyon’s canal or ulnar tunnel. This canal is surrounded by certain ligaments and bones of the wrist. Within Guyon’s canal, the ulnar nerve further branches out into a deeper motor nerve and a more superficial sensory nerve. This canal is divided into three parts: Part 1 is before the nerve separates, Part 2 only contains the motor branch, and Part 3 only contains the sensory branch.
So, if compression occurs in the cubital tunnel or Part 1 of Guyon’s canal, this can lead to both movement and sensation problems caused by the ulnar nerve. If the issue is in Part 2 of Guyon’s canal, it will only affect motor functions, while a problem in Part 3 will only result in sensory issues.
The ulnar nerve is very important as it powers many small muscles in the hand. These muscles allow grip and intricate hand movements. It also carries sensation from the half of the ring finger and the small finger, as well as the inner part of the hand, back to the brain.
What Causes Ulnar Nerve Entrapment?
Ulnar nerve entrapment, a condition where the ulnar nerve is pinched, can happen most often in the ‘cubital tunnel’ or in ‘Guyon’s canal.’ In the cubital tunnel, the nerve can be squeezed between Osborne’s ligament (a connective tissue) and the MCL of the elbow (a ligament that provides stability to the elbow) which can then cause symptoms like pain, tingling, or numbness in the forearm and hand.
In Guyon’s canal, depending on the precise area of compression, the symptoms will differ. If the compression is at the start of Guyon’s canal (zone 1), it will likely cause both movement issues and sensory problems. This is usually due to ganglia (small sacs of fluid) or fractures in a tiny wrist bone called the ‘hook of the hamate’.
If the compression is in the middle section of the canal (zone 2) post the nerve’s split, it will just cause issues with movement of the hand. As with zone 1, this is most often caused by ganglia or fractures of the ‘hook of the hamate’.
If the compression is near the end of the canal (zone 3), it will lead to sensory issues in the hand areas served by the ulnar nerve. This is generally caused by issues with the ulnar artery like a blockage (thrombosis) or an enlarged, weakened arterial wall (aneurysm).
Risk Factors and Frequency for Ulnar Nerve Entrapment
A study from Italy found that elbow-related nerve compression issues occur twice as often in men compared to women.
Signs and Symptoms of Ulnar Nerve Entrapment
Ulnar nerve compression has a gradual onset and usually manifests as numbness and a tingling sensation in the smallest finger, half of the ring finger, and the base of the palm. Over time, weakness and hand thinning may ensue if compression occurs in a critical zone of the wrist. This can lead to clumsiness and reduced strength while pinching, often determined by a physical examination called Froment’s test. In this test, the patient is asked to hold a piece of paper between their thumb and the side of the index finger. The thumb curling or flexing at the joint to grip the paper instead of using muscles near the thumb indicates a positive Froment’s sign, revealing a dysfunctional ulnar nerve.
A test known as Tinel’s sign might cause tingling sensations and numbness to recur, suggesting probable nerve damage at that area. Another physical exam, Wartenberg’s sign, checks for motor weakness. In this test, the patient keeps his or her fingers fully extended. If the smallest finger drifts away from the others, it’s a positive Wartenberg sign, indicating a deficiency in palmar muscles innervated by the ulnar nerve. These symptoms point to a compressed nerve at that location.
Deciphering the difference between additional conditions like a C8 radiculopathy and peripheral nerve compression is essential. Nerve-related changes in the forearm as opposed to just the hand suggests C8 radiculopathy and not ulnar nerve compression at the elbow. Similarly, specific muscles of the thumb, which are controlled by the C8 nerve root via the median nerve, may show weakness in C8 radiculopathy but not in a peripheral ulnar nerve compressive neuropathy.
Last but not least, the presence of a “snapping” or “popping” sound in the elbow could reveal nerve mobility within the cubital tunnel, suggesting that repositioning the ulnar nerve could be a suitable treatment approach.
Testing for Ulnar Nerve Entrapment
If your doctor suspects that something might be pressing or squeezing your nerve (a condition often referred to as nerve entrapment), they will likely want to take X-rays of your arm, specifically focusing on your elbow and wrist. X-rays can help your doctor see if there are any issues or changes in the structures of these areas that could be causing your symptoms. They might also want to look at your neck and chest with X-rays to rule out other conditions that could be causing your symptoms. For example, an issue with the first rib or a problem in the neck could create similar symptoms. In some cases, a chest x-ray is necessary to check if a growth in the lungs (such as a tumor) is pressing on a nerve.
Your doctor may be interested in taking X-rays of your elbow to look for any developmental abnormalities, after-effect of an injury, or any misalignment in the elbow which could be potentially causing nerve issues. Similarly, by taking X-rays of your wrist, your doctor can check for any fractures in your hamate bone (a small bone in the wrist), which is a common cause of ulnar nerve compression symptoms in the hand. If there’s a high suspicion of a fracture in the hamate bone, a computed tomography (CT) scan may be ordered, as it can provide a better and more detailed image of the bone than an x-ray.
When further confirmation is needed, the doctor may order a Magnetic Resonance Imaging (MRI), a type of scan that uses strong magnetic fields and radio waves to produce detailed images. MRI is particularly helpful in confirming suspicions of problems in the neck – such as cervical radiculopathy (where a nerve in the neck is irritated or compressed), or diagnosing cysts or other masses in the wrist that are taking up space and causing issues.
An Ultrasound can also be used, where the doctor will take a look at the nerve in the elbow and wrist. Ultrasounds use sound waves to create images, and can provide details such as the size of the ulnar nerve (one of the main nerves in the arm), and if there is a clot in the ulnar artery which can lead to ulnar nerve symptoms in the hand.
To check the function of your nerves and muscles, your doctor might use a test called electromyography. This test measures the electrical activity in your nerves and muscles when they’re at rest and when they’re being used. If you have a nerve compression issue such as cubital tunnel syndrome (a condition that affects the ulnar nerve near the elbow), this test can identify a slowing of signals in the ulnar nerve where it crosses the elbow.
Treatment Options for Ulnar Nerve Entrapment
If you’re having pain or other symptoms due to ulnar nerve problems, but there’s no muscle weakness or wasting, your doctor might start with noninvasive treatments. These could involve taking anti-inflammatory medications to reduce swelling and pain, using external padding to protect the nerve, and wearing a night splint to keep the elbow at a 45-degree angle or the wrist in a neutral position, depending on the root cause of the nerve pressure. Additionally, your doctor may recommend occupational therapy to teach you how to position your arm in a way that reduces symptoms.
If you’re having a condition called cubital tunnel syndrome, and you have severe muscle weakness or wasting, or if the noninvasive treatments don’t help, your doctor might suggest surgery. In surgery, the doctor would release a tissue called Osborne’s ligament that can put pressure on the nerve, relieving the nerve tension. They might also move the ulnar nerve to a new position that reduces the pressure and traction on it when you move your elbow. But these procedures can carry risks, and other types of surgery may be used instead, like a medial epicondylectomy. A medial epicondylectomy has a lower chance of causing ulnar nerve injury but can potentially increase the risk of elbow instability and flexor-pronator weakness.
If you’re having a condition called ulnar tunnel syndrome, surgery would involve addressing the specific cause of the nerve pressure. If masses or cysts are causing the compression, the surgeon may remove them. The usual surgical procedure involves relieving the pressure on the nerve across all four compartments of the Guyon’s canal, a tunnel in your hand where the ulnar nerve passes through. However, if you only face motor function issues, your doctor might recommend managing with the release of a ligament in your wrist and searching for a deep ganglion cyst, a swelling filled with fluid.
What else can Ulnar Nerve Entrapment be?
C8-T1 radiculopathies are quite uncommon, especially when compared to ulnar nerve compression syndromes that affect the outer part of the arm. These two conditions often show similar symptoms, so it’s easy for doctors to overlook a C8-T1 radiculopathy. To make an accurate diagnosis, doctors need to understand the ulnar nerve’s structure thoroughly. Therefore, a detailed physical exam, which includes testing muscle and sensory functions, combined with specific diagnostic tools like electromyography and MRI scans, is essential.
The ulnar nerve powers various muscles in our hands, such as the muscles on the palm’s outer edge, the muscles between our fingers, thumb muscles, and a part of the palm muscles. The median nerve, on the other hand, enters the hand via the “carpal tunnel”, a narrow passage in the wrist. This nerve influences the remaining palm and thumb muscles, along with some finger muscles. In case of an isolated ulnar nerve compression, these five particular muscles would be expected to stay functional, while with a C8-T1 radiculopathy condition, weakness can be seen in these specific muscles.
For most people, it’s the ulnar nerve that gives sensation to their pinky finger, the half of the ring finger that is closer to the pinky finger, and a specific region of their hand, both front and back. But remember, this nerve doesn’t provide sensation to the forearm’s inner part; that’s covered by another nerve called the “medial antebrachial cutaneous nerve,” originating from a network of nerves in the shoulder (brachial plexus). If there’s a reduction in sensation in the inner forearm, it can indicate serious issues like radiculopathy or even certain kinds of lung cancer, like Pancoast tumors, affecting the brachial plexus. On the contrary, if sensation in the inner forearm is normal, the doctors may then try to explore a possibility of ulnar nerve compression syndrome.
What to expect with Ulnar Nerve Entrapment
Studies of 50 cases of ulnar nerve compression, a condition where the ulnar nerve in your arm is squeezed, indicate that non-surgical treatments can provide excellent results for patients experiencing a mild level of compression, about 50% of the time. These treatments may include anti-inflammatory medication, external supports, and changing certain positions or movements.
If surgery is needed, it can almost always completely relieve the symptoms. This is assuming that the exact place where the nerve is compressed, is correctly identified. The surgical procedure often includes moving the nerve to a different position in the arm – this is called an anterior transposition of the nerve. However, this movement should only be done when deemed necessary.
Possible Complications When Diagnosed with Ulnar Nerve Entrapment
After having surgery, the return of symptoms usually comes from either an incomplete relief of pressure on the nerve or tissue scarring around the nerve. The surgical procedure for the cubital tunnel presents risks to several structures in the area. If the medial antebrachial cutaneous nerve is damaged, it can lead to abnormal feelings of sensitivity and an exaggerated response to pain in the inner side of the forearm. There have been cases of damage to the medial collateral ligament of the elbow, a known risk in transposition operations, which can lead to chronic elbow instability. When performing the surgical release procedure of the ulnar tunnel, surgeons must be very careful. They could potentially harm the ulnar artery, which is in front of and to the side of the ulnar nerve, or the wrist ligaments, leading to a loose and unstable wrist.
Risks category:
- Return of symptoms
- Incomplete relief of pressure on the nerve
- Tissue scarring around the nerve
- Damage to medial antebrachial cutaneous nerve
- Exaggerated response to pain in inner forearm
- Damage to medial collateral ligament of the elbow
- Chronic elbow instability
- Damage to the ulnar artery
- Damage to the wrist ligaments
- Instability in the wrist
Recovery from Ulnar Nerve Entrapment
Doctors usually advise patients to start moving early after having surgery to release the ulnar nerve at the elbow. This is done to avoid severity or the sticking together of tissues (known as adhesions) and to prevent the elbow from becoming stiff.
Preventing Ulnar Nerve Entrapment
If you frequently experience numbness, weakness or pain in your little and ring fingers, there could be various reasons for it. An orthopedic doctor, who is specialized in bone and muscle conditions, can help identify the cause of these symptoms and discuss all possible treatment options with you. As per the findings, more than half of these patients see improvement with non-surgical treatment. However, there may be cases where surgery becomes necessary. In such cases, it’s crucial to know that where the problem area is and how well the surgeon can relieve pressure from it can significantly affect the success of the treatment.












