What is Intracranial Hemorrhage?
An intracranial hemorrhage, or bleeding in the brain, can be of four main types:
- Epidural hemorrhage – bleeding between the outer layer of the brain (dura mater) and the skull.
- Subdural hemorrhage – bleeding between the inner layer and outer layers of the brain.
- Subarachnoid hemorrhage (SAH) – bleeding between the brain and the thin tissues that cover the brain.
- Intraparenchymal hemorrhage – bleeding directly into the brain tissue itself, usually into one of the two halves (cerebral hemispheres).
The first two types are known as ‘extra-axial hemorrhages’ and the others are ‘intra-axial hemorrhages’. The types of bleeding differ in their causes, the signs and symptoms they show, their possible outcomes and how they affect the patient’s prognosis or the likely course of the disease. This article provides an overview of the different types of bleeding in the brain.
What Causes Intracranial Hemorrhage?
An epidural hematoma is a collection of blood that can form between the skull and the outermost covering of the brain. This can happen when there’s a strong blow to the head, usually to the side of the head, or when something penetrates the skull, like a fracture. The blood usually comes from a damaged artery, often the middle meningeal artery, although any brain-covering artery can create this issue.
A venous epidural hematoma is similar, but the source of the bleeding is the veins, not the arteries. It also happens after a skull fracture, with the blood filling the same space. This is common in children.
A subdural hemorrhage is also a result of a head injury where blood leaks into the subdural space, the area between the brain and its covering. This happens when a blood vessel stretching between the brain and the skull gets stretched, broken or torn and starts leaking blood into the space. This is most common with head injuries but can also happen with something that penetrates the skull or even seemingly out of nowhere.
A subarachnoid hemorrhage refers to bleeding in the space around the brain. It can be caused by an injury or could happen without an injury. We also classified them into two types, one associated with a ruptured brain aneurysm (a bulge in a blood vessel), and one not linked to any identifiable aneurysms. In the latter case, blunt head injuries or quick changes in head motion are common causes.
Intraparenchymal hemorrhage refers to bleeding directly into the brain tissue itself. This can be caused by many different things like high blood pressure, abnormal blood vessels, aging-related blood vessel diseases, ruptured aneurysms, tumors, blood clotting issues, infections, inflammation of blood vessels, and trauma.
Risk Factors and Frequency for Intracranial Hemorrhage
Epidural, subdural, subarachnoid, and intraparenchymal are different types of head hemorrhages or bleeding in the brain. These different types of hemorrhages can occur as a result of head injuries or, in some cases, they might be linked to strokes.
- Epidural hematomas are in about 2% of head injury patients and make up 5% to 15% of deadly head injuries. Most of the time (85% to 95%), epidural hematomas come with a skull fracture. Every year, 3.1 million people globally need surgery due to a traumatic epidural hemorrhage.
- Subdural hematoma is found in between 5% and 25% of patients with serious head injuries, and happens to 1 to 5 people per 100,000 each year. It’s more common in men than in women. The likelihood of getting a subdural hematoma goes up as you get older.
- Subarachnoid hemorrhage is responsible for about 5% of all strokes and affects 2 to 25 per 100,000 people above 35 every year. This incident becomes slightly more common with age and maybe slightly more frequent in women than in men.
- Intraparenchymal hemorrhage accounts for 10% to 20% of all strokes and becomes more common in people aged 55 and above. There’s some debate about if it’s more common in men or women, but it might be slightly more common in men.
Signs and Symptoms of Intracranial Hemorrhage
An epidural hematoma is a type of head injury that often results from a heavy blow to the head like from a hammer or a fall. The unique characteristic of this condition is a period of unconsciousness, followed by a brief period of seeming normality, then eventually worsening neurological symptoms. However, this only occurs in less than 20% of cases. Other symptoms can include a severe headache, feeling sick, vomiting, feeling tired, and having a seizure.
Subdural hemorrhage, another type of head injury, is commonly associated with both minor and major head impacts. In older individuals, even mild injuries can cause a subdural hematoma. Symptoms of acute subdural hematoma include recent trauma, headache, nausea, vomiting, altered mental state, seizure, and/or lethargy. Chronic subdural hematoma, on the other hand, may present symptoms like headache, nausea, vomiting, confusion, decreased consciousness, lethargy, motor deficits, difficulty communicating, seizure, or changes in personality. Physical examination may reveal certain movement difficulties, neurological deficits, lethargy, or altered awareness.
Subarachnoid Hemorrhages are often recognized by a sudden severe headache, often described as the worst headache of one’s life. Other symptoms may include feelings of dizziness, nausea, vomiting, blurred or double vision, seizures, loss of consciousness, or neck stiffness. During a physical exam, doctors may observe specific neurological deficiencies, cranial nerve impairments, neck rigidity, or decreased or altered awareness.
- Sudden severe headache
- Feelings of dizziness
- Nausea
- Vomiting
- Blurred or double vision
- Seizures
- Loss of consciousness
- Neck stiffness
- Specific neurological deficiencies on physical exam
Intraparenchymal Hemorrhages are non-traumatic brain bleeds and are typically identified by a sudden onset of stroke-like symptoms. These symptoms can include a headache, nausea, vomiting, focal neurological deficits, lethargy, weakness, slurred speech, fainting, dizziness, or changes in sensation.
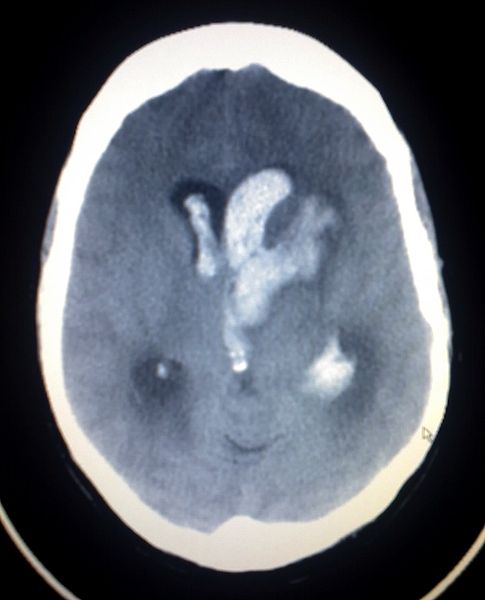
hemorrhage is observed with intraventricular bleeding on the head CT of a
patient.
Testing for Intracranial Hemorrhage
During the initial check-up, the doctor will assess your breathing, the airway, and blood circulation. A comprehensive examination of your neurological health is also necessary to check for any signs of dysfunction.
The severity of any potential neurological injury can be assessed using the Glasgow Coma Scale (GCS). This scale measures three components:
- Your eye-opening response (rated 1 to 4)
- Your best verbal response (rated 1 to 5)
- Your best motor (movement) response (rated 1 to 6)
Using these scores, any traumatic brain injury can be classified as mild (13 to 15), moderate (9 to 12), or severe (8 or less).
Your doctor may also order blood tests to check for any signs of abnormal platelet count, blood clotting issues, and any problems with your body’s chemical balance.
Imaging tests like a non-contrast CT scan of the brain might also be carried out to help with the diagnosis.
In case of a brain bleed called epidural hemorrhage, the pressure within the skull may increase, causing high blood pressure, slow heart rate, and irregularity in the breath. Special imaging can identify a dense, slightly bulging opacity, which is a common sign of this condition.
An acute subdural hematoma, another type of brain bleed, appears as a dense region on imaging, whereas a chronic subdural is less dense. A subacute subdural may have the same density as the brain, making it harder to identify.
Another kind of brain bleed called a subarachnoid hemorrhage can lead to rapid deterioration of health, and may require immediate intubation (placing a tube in the throat to help with breathing). Contrast dye during imaging can make this condition harder to see. If there’s strong suspicion of a subarachnoid hemorrhage and the CT scan doesn’t show it, a procedure to draw out cerebrospinal fluid from the lower back to look for signs of bleeding might be necessary.
It’s important to identify the cause of a non-traumatic subarachnoid hemorrhage to guide further treatment. Different imaging methods such as CT angiogram (a special type of CT scan that highlights the blood vessels), MRA (which uses magnets and radio waves to create pictures of the blood vessels), or diagnostic cerebral angiogram (X-ray image of the head and neck vessels which uses dye) may be used to check for any bulging blood vessels, abnormal vascular connections or other sources of hemorrhage.
Another condition called intraparenchymal hemorrhage appears as a dense region within the brain tissue on imaging. Additional imaging like an MRI scan of the brain, might be considered depending on the medical and physical assessments.
Depending on the type and stage of the brain bleed, MRI scans can show different patterns of result intensity. Learning about these patterns can help doctors to determine the stage of the hemorrhage; whether it is in the very early stages (<12 hours), acute stage (12 hours to 2 days), early subacute stage (2 to 7 days), late subacute stage (8 days to 1 month), or chronic (>1 month).
The most common type of brain bleed in newborns is known as germinal matrix hemorrhage or periventricular-intraventricular hemorrhage (PVIH). Depending on the extent of the hemorrhage and the areas of the brain affected, PVIH is classified into four different grades.
Finally, there are other types of brain bleeds like asymptomatic sharpened brain tissue bleed, often studied as a sign of disease severity in patients with high blood pressure-related blood vessel disease. Remote cerebellar hemorrhage (RCH) typically takes place after brain or spinal surgery and occurs away from the surgical site without any evident pathological defect.
Treatment Options for Intracranial Hemorrhage
If someone experiences a brain bleed, which we often call a hemorrhage, they should seek immediate help from a brain specialist, especially if they have alarming signs like difficulty breathing or unstable heart rates.
There are different types of brain bleeds, and how we treat them depends on various factors:
Epidural Hemorrhage: This is a type of brain bleed that occurs outside the brain but inside the skull. The best treatment is usually to remove the pooled blood (we call this a hematoma) and stop the bleeding. However, if the bleed is small and the person doesn’t have serious symptoms, we can sometimes manage it without surgery, simply monitoring the person until the hematoma resolves itself.
Subdural Hemorrhage: This type of bleed happens between the brain and its outermost covering. The best treatment here is also to remove the hematoma, but in some cases, the hematoma may resolve itself with careful monitoring. In these cases, we might do repeat scans to check that the hematoma isn’t growing, try to reverse any blood-thinning medications the person might be on, and give them platelet transfusions to help their blood clot more effectively. We might also watch them closely for any worsening symptoms and try to keep their blood pressure under control.
Subarachnoid Hemorrhage: This happens when blood fills the space between the brain and the skull. We also manage this conservatively, closely monitoring the person’s vital signs and neurological status. If the person is unconscious, they might need a procedure to monitor or relieve the pressure inside their skull. If the hemorrhage wasn’t caused by an injury, the treatment will depend on what did cause it. For example, they might need treatment for a bulged blood vessel or other underlying issues.
Intraparenchymal Hemorrhage: This is a bleed that happens inside the brain tissue itself. The treatment depends mainly on what caused the bleed. Options can include removing the hematoma surgically, dissolving it with a catheter, or just keeping a close eye on it. Keeping blood pressure under control and reversing any blood-thinning medications are also important. Sometimes, trying to remove the hematoma can do more harm than good, so we might need to do a different kind of surgery to relieve pressure on the brain instead.
In some cases, surgery may be needed to remove a mass of small blood vessels known as a cavernoma, especially if it’s causing severe symptoms or it’s located near the surface of the brain.
What else can Intracranial Hemorrhage be?
When a doctor is trying to diagnose a brain bleed, also known as an intracranial hemorrhage, they will also consider other conditions which might mimic a hemorrhage. These conditions may appear the same on a scan, but they require different treatments. Here are some possibilities:
- Infection: For instance, a Subdural empyema is an infection that may look like a subdural hemorrhage, a type of stroke caused by bleeding on the surface of the brain.
- Recent contrast administration: Sometimes, the substances used to improve the visibility of structures or fluids within the body during medical imaging can create appearances that look like hemorrhaging.
- Subdural hygroma: This is a condition where cerebrospinal fluid accumulates under the outermost membrane that covers the brain. It may look like chronic subdural hemorrhage.
- Tumors: For example, Meningiomas, which are mostly non-cancerous tumors, can mimic an extradural hemorrhage, another type of bleeding in the brain.
What to expect with Intracranial Hemorrhage
The outlook for a patient after a brain bleed depends on several things. The patient’s age, other health conditions, if they take blood thinners or platelet inhibitors, their level of consciousness when they arrive at the hospital (measured by the Glasgow Coma Scale), the size of their pupils, where the bleeding occurred in the brain, if there are other injuries, and how quickly they can get surgery if needed, all play a role in their recovery.
The ICH Score is a way doctors determine how severe the brain bleed is and calculate the chance of death. This score is calculated based on different aspects such as:
1. The Glasgow Coma Scale score:
- A score of 3 to 4 gives 2 points
- A score of 5 to 12 gives 1 point
- A score of 13 to 15 gives 0 point
2. Age:
- If the patient is 80 years or older 1 point is given
- If the patient is younger than 80, the score is 0 point
3. The location of the bleed:
- If it is below the tentorium (part of the brain), 1 point is given
- If it is above the tentorium, it’s 0 point
4. The size of the brain bleed:
- If the bleed is greater than or equal to 30 cubic cm, 1 point is given
- If it is smaller than 30 cubic cm, it’s 0 point
5. If there is a bleed into the ventricles of the brain:
- If there’s a bleed into the ventricles, 1 point is given
- If the bleed didn’t affect the ventricles, it’s 0 point
The risk of death is evaluated using this ICH score as follows:
- 0 points: 0% risk
- 1 point: 13% risk
- 2 points: 26% risk
- 3 points: 72% risk
- 4 points: 97% risk
- 5 points: 100% risk
- 6 points: 100% risk (estimated)
Possible Complications When Diagnosed with Intracranial Hemorrhage
Intracranial hemorrhage, or brain bleeding, can lead to several serious complications. These include neurological deficits (problems with the nerves’ function that affect movement, speech, and bodily functions), brain herniation (when the brain shifts out of its normal position), infarcts (dead tissue due to lack of blood flow), rebleeds (recurrence of bleeding), vasospasm (narrowing of the blood vessels), seizures, and even death.
Possible Complications:
- Neurological deficits
- Brain herniation
- Infarcts
- Rebleeds
- Vasospasm
- Seizures
- Death
Preventing Intracranial Hemorrhage
Patients should be informed about how vital it is to follow their rehab program and take their medication as directed while they’re recovering. They shouldn’t drive unless the doctor has confirmed it’s safe for them to do so.