What is Pudendal Nerve Entrapment Syndrome?
Pudendal neuralgia, caused by the entrapment of the pudendal nerve, is a long-term, often greatly disabling pain condition. This affects the region of the body that the pudendal nerve serves and can occur in both men and women. Over half of people with this condition experience pain in the area between the genitals and the anus (perineal pain) that worsens when they sit but is lessened when they stand or lie down. This condition is often either misdiagnosed or not diagnosed enough, leading to incorrect treatment, delays in correct management, and a major negative impact on the person’s quality of life.
Understanding the Pudendal Nerve
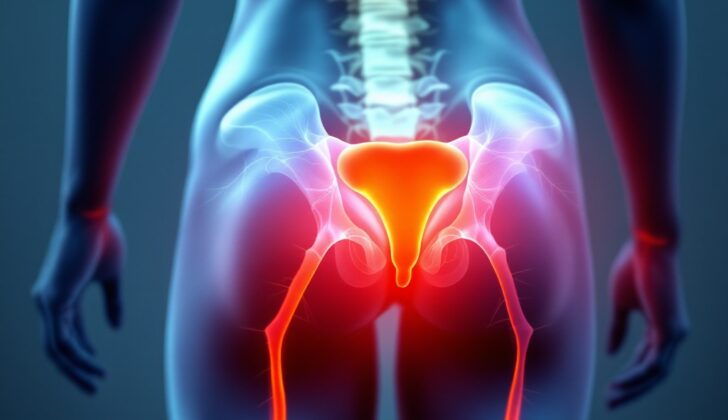
The pudendal nerve originates from the roots of the second, third, and fourth sacral nerves (S2, S3, and S4). It transmits various kinds of nerve signals, but damage to this nerve is primarily associated with sensory problems rather than motor issues. The nerve first travels between two muscles: the piriformis and the coccygeus muscles. It then leaves the pelvic area through an opening called the greater sciatic foramen, located in front of a ligament called the sacrotuberous ligament. From there, it travels under the sacrospinous ligament at the top of the ischial spine (the prominent bone at the bottom of your pelvis) and re-enters the pelvic area through the same opening. The pudendal nerve then moves into a canal called the Alcock (or pudendal) canal. The final three branches of the pudendal nerve end in an area called the ischioanal fossa. These are the inferior rectal branch, the perineal branch, and the sensory nerve that serves the penis in men or the clitoris in women. However, some documented cases have shown variations in the layout of the pudendal nerve.
Understanding Pudendal Nerve Compression
The classification of pudendal nerve entrapment syndromes is divided into four types, determined by where the compression is.
* Type I – The nerve is entrapped under the piriformis muscle as it exits an area called the greater sciatic notch.
* Type II – The nerve is entrapped between two ligaments, the sacrospinous and sacrotuberous. This is the most common site of pudendal nerve entrapment.
* Type III – The nerve is entrapped in the Alcock canal.
* Type IV – The terminal branches of the nerve are entrapped.
What Causes Pudendal Nerve Entrapment Syndrome?
Pudendal neuralgia is a condition that involves pain along the path of the pudendal nerve, which is located in the pelvic area. This pain can be caused by physical damage or non-physical causes.
Physical damage can be due to pressure, cutting, or stretching effects. Among these, compression caused by the pudendal nerve being trapped is the most usual reason. Non-physical causes of pudendal neuralgia can range from viral infections (like shingles or HIV), conditions such as multiple sclerosis, treatments like radiation therapy, or other conditions like diabetes.
The first known case of pudendal neuralgia came about due to bike riding, which led to continuous pressure on a particular part of the nerve’s pathway called Alcock’s canal.
There are multiple possible causes for Pudendal Neuralgia:
1. Surgery in the pelvic area: The most common cause is reportedly surgery for repairing a prolapse of pelvic organs, where organs drop from their normal position. The risk is higher if a special type of netting, called a mesh, is used. Persistent pain after surgery might sometimes require removing the mesh. This condition may also occur after surgeries such as a procedure to support the urethra, removal of the uterus, and repair of the front wall of the vagina.
2. Trauma: Pudendal neuralgia can also come from direct damage to the buttocks or back.
3. Childbirth: Giving birth through the vagina can vastly stretch the pelvic floor muscles due to the baby’s head, sometimes leading to pudendal nerve damage.
4. Chronic constipation.
Excessive bicycle riding can also cause this condition. It is presumed to be because of the chronic minor damage to the area between the anus and the genitals, which causes scarring in the pudendal canal as well as certain ligaments in the pelvic area. Sitting for too long periods can also contribute to this condition.
Risk Factors and Frequency for Pudendal Nerve Entrapment Syndrome
Pudendal nerve entrapment is a rare syndrome with an unknown precise prevalence. The International Pudendal Neuropathy Foundation estimates that the condition occurs in 1 out of every 100,000 people. However, many believe the actual number is significantly higher than reported. Roughly 1% of the general population may suffer from this syndrome. The syndrome also makes up about 4% of all patient consultations regarding pain control. Women are more than twice as likely to be affected as men.
Signs and Symptoms of Pudendal Nerve Entrapment Syndrome
Pudendal nerve entrapment is a condition that primarily causes a pain in the area between your hips (the perineal area) which gets worse when you sit and better when you stand or sit on a toilet. It can also lead to other symptoms:
- Feeling of pain, numbness, or dysfunction in the private parts, area between the hips, back passage, and lower part of the urinary system.
- Experiencing urinary issues like the constant need to pee, the need to pee frequently, and painful ejaculation in men.
- Experiencing sexual dysfunction, including unending arousal, painful intercourse, vulvodynia (pain in the external female genitalia), and erection problems in men.
- Dysfunction of the sphincter muscle (muscle used to control the exit of feces) which can lead to constipation, painful or difficult urination, inability to control bowel movements, and difficulty in beginning to urinate.
There might also be a feeling of having a foreign object in the back passage, urethra, or vagina.
In physical examinations, patients with this condition are typically normal except for the fact that they experience pain again. The symptoms depend on the exact location and severity of the entrapment. If the nerve is compromised at certain places like the ischial spine (pelvic bones) or the sacrospinous ligament, it can cause inner thigh pain. On the other hand, if the nerve gets trapped at the greater sciatic notch, there can be tenderness over this area. Entrapment at the piriformis (a muscle in the buttocks) could lead to spasms and tenderness of this muscle, while entrapment within Alcock’s canal can lead to tenderness and spasms of a muscle called Obturator Internus.
Doctors suggest undergoing rectal and vaginal examinations to rule out other possible conditions like prostatitis and also to identify any entrapments within the pelvic area.
Testing for Pudendal Nerve Entrapment Syndrome
Diagnosing pudendal nerve entrapment, a condition that can cause chronic pelvic pain, can be tough because there are no specific tests for it. It’s important for the doctor to get a thorough medical history and conduct a detailed physical examination to identify this condition. Dr. Roger Robert developed a criterion, known as the “Nantes” criteria, which can help diagnose pudendal nerve entrapment. Many European physicians have successfully used this guideline.
If every characteristic of the “Nantes” criteria is present, usually no more tests are required to diagnose this condition. If some aspects are missing, more tests may be needed.
The “Nantes” criteria includes main features, such as pain in areas where the pudendal nerve provides sensation including the genital and perineum areas. This pain usually worsens when sitting, but doesn’t affect sleep. People with this condition normally don’t suffer from a sensory loss, which if present, could indicate another type of nerve damage. Additionally, relief from pain with a pudendal nerve block is a key criterion for this diagnosis. Although, a negative block doesn’t completely rule out pudendal nerve entrapment.
There are additional guys of this condition, these can include pain described as burning, sharp or stabbing, increased sensitivity to pain, sensations as if a foreign body is present, pain that increases as the day progresses, and pain that is worse on one side or after certain activities.
The criteria also has certain features that if present would exclude pudendal nerve entrapment as the diagnosis. For instance, if the pain is only in a region not served by the pudendal nerve, is accompanied by itching, or comes and goes quickly, it might be a different condition. Other symptoms associated with this condition include pain in other areas such as the buttock, inside of the thigh, or lower abdominal area, as well as sexual dysfunction.
In terms of diagnostic tests, a few can help in identifying pudendal nerve entrapment. The warm sensory threshold test measures how a patient senses gradual temperature changes due to the fact that affected nerves may have trouble in transmitting these sensations. Another test that can be performed is the pudendal nerve terminal motor latency test. It’s a bit more invasive since it measures how long it takes for a nerve signal to travel from the pelvic region to the anal sphincter. High-frequency ultrasonography can be used to locate where the nerve is compressed, and magnetic resonance imaging (MRI) can be used to rule out other causes of chronic pain.
Pudendal nerve block injections with a local anesthetic can also serve to confirm the diagnosis. If the patient experiences pain relief immediately following the procedure, it suggests that pudendal nerve damage is the likely cause of the pain. A lack of pain relief does not necessarily mean that it’s not pudendal entrapment, as the injection might have been incorrectly administered. Using imaging can increase the reliability of nerve blocks. However, about 20% of pudendal nerve blocks may fail due to various reasons.
Treatment Options for Pudendal Nerve Entrapment Syndrome
If you’re experiencing intense, recurring pain due to an issue with your pudendal nerve, there are several treatment options available ranging from lifestyle adjustments, physical and behavioral therapies, medication, and surgery. The pudendal nerve plays a crucial role in muscle control in your pelvic area, transmitting sensation and pain signals to your brain, so dealing with problems here might require a tailored approach.
Often, the first step is to avoid activities that intensify your pain. For instance, if you feel pain due to certain activities like cycling, jogging, or long periods of sitting, try to either modify how you do these activities, or stop them altogether. Around 20-30% of patients get relief from taking these steps alone.
You might also benefit from physical therapy if your pain is due to muscle spasms. Over a course of 6 to 12 weeks, you can learn exercises to help relax your pelvic floor muscles, releasing spasms and lengthening muscles. Additionally, a treatment called transcutaneous electrical nerve stimulation (TENS) is often beneficial. This technique is safe, easy to do, doesn’t break the skin, and generally isn’t too costly.
If you’re also dealing with anxiety, depression, or other psychological difficulties (which are common in people with long-term pain), you might find cognitive behavioral therapy helpful. This type of therapy helps you address and manage negative thought patterns and behaviors.
Pain relief medications, muscle relaxants, and other drugs are often used to manage pudendal nerve issues. There isn’t a one-size-fits-all approach, so your doctor will likely try a combination of medications to find what works best for you. However, opioids are generally avoided due to their potential risks.
If your pain is focused in a specific part of the pudendal nerve, getting a nerve block might be an option. This involves having a local anesthetic or steroid injected near the nerve to numb it and reduce pain. This treatment can be repeated when necessary, and around 25% of patients experience pain relief for over a month afterwards.
If other treatments are unsuccessful, there are a few surgical options available. One approach is surgical decompression, where the surgeon works to free the pudendal nerve from any trapped or compressed areas. This can be quite effective, with about a 70% success rate. Another approach uses an electronic nerve stimulator to manage the pudendal nerve. Initial results seem promising, though more research is needed.
Other treatments, such as radiofrequency ablation, cryotherapy and lipofilling, are newer and may be considered for chronic cases that haven’t responded to other treatments. As with any medical treatment, it’s important to have a conversation with your healthcare provider about all your options and the potential benefits and risks.
What else can Pudendal Nerve Entrapment Syndrome be?
Pudendal neuralgia is a condition that is quite tricky to diagnose because there isn’t a specific test that can confirm it. So, doctors usually diagnose it by ruling out other conditions first. Here are some of the other conditions that doctors may consider before finally diagnosing pudendal neuralgia:
- Compression by an external source, which could be a benign or cancerous tumor or even a spread of cancer from another part of the body.
- Skin infections that occur in areas covered by the pudendal nerve.
- Neuropathy, or nerve damage, of the sacral region which is caused by damage to the sacral nerve network.
- Trauma during childbirth that causes the area between the vagina and the rectum to stretch excessively.
- Complex regional pain syndrome, a chronic pain condition that causes pain in one of the limbs, usually after an injury.
- Chronic prostatitis, a long-term inflammation of the prostate.
- Prostatodynia, which is pain in the prostate area.
- Vulvodynia, a condition causing pain in the vulva, the outer part of a woman’s genitals.
- Vulvar vestibulitis, an inflammation of the vestibule, or entrance to the vagina.
- Chronic pelvic pain syndrome, a condition causing pain in the area below your bellybutton and between your hips.
- Coccygodynia, a condition that causes pain in the coccyx or tailbone.
- Sacroiliac joint dysfunction, a condition that causes pain in your lower back and buttocks.
- Piriformis syndrome, a condition that affects a muscle in your buttocks called the piriformis, causing buttock pain.
- Ischial bursitis, a condition that causes pain in the lower buttocks or upper hamstring area.
- Interstitial cystitis, a chronic condition causing bladder pressure and pain.
What to expect with Pudendal Nerve Entrapment Syndrome
Pudendal neuralgia, a condition caused by the entrapment of the pudendal nerve, can significantly impact your everyday life, though it doesn’t shorten your lifespan. About 80% of properly selected patients benefit from pudendal nerve blocks, a treatment that involves an injection to reduce pain. However, this relief usually lasts only about a month for most patients. After this period, they may need another injection or a different form of treatment.
The most effective long-term solution is decompressive surgery, which works for 60% to 80% of patients. This surgery aims to relieve pressure on the pudendal nerve. Even when this surgery doesn’t work, up to 80% of patients can still obtain relief from a procedure called sacral neuromodulation. This approach involves delivering electrical signals to the nerves through a small device implanted under the skin.
Possible Complications When Diagnosed with Pudendal Nerve Entrapment Syndrome
The risks associated with pudendal nerve blocks are rare, but can still occur. These might include:
- Cuts to the lining of the vagina
- Accidental injection of numbing medicine into a blood vessel, which could lead to symptoms like a racing heart, low blood pressure, slow heart rate, slurred speech, ringing in the ears, sleepiness, confusion, fainting, and seizures
- A bruise from damage to the pudendal artery or nearby blood vessels
- Infection and/or pain at the spot of the injection
- Formation of an abscess, which is a pocket of pus caused by infection
Pudendal nerve decompression surgery, another possible treatment, also has some risks, although they are pretty rare. During surgery, a small branch of the nerve might be injured but could be fixed with microsurgery if needed. A part of the ligament that helps with stabilizing the pelvis could be harmed during the surgery, leading to an unstable pelvis. To prevent this from happening, the doctor might choose to make the surgical cut (or incision) in a particular way.
Something to note is that the relief from surgery doesn’t happen immediately. The pain typically lessens gradually over a few months. While this might be seen as a downside to the surgery, it’s important to understand that this is a part of the normal healing process and is not a negative consequence of the surgery.
Preventing Pudendal Nerve Entrapment Syndrome
Doctors should advise patients to stay away from any activities or stimuli that cause them pain and to actively engage in physical therapy. It’s also beneficial for patients to make certain changes in their daily activities to help manage their condition. This could include avoiding activities that worsen their condition and ensuring they use a comfortable seating pad. These are crucial steps in the overall treatment plan.