What is Serotonin Syndrome?
Serotonin syndrome, also known as serotonin toxicity, is a serious medical condition that can potentially be life-threatening. It happens when there’s too much activity from serotonin, a substance in your brain that helps regulate your mood, behavior, and other bodily functions. It’s produced naturally in your body but can also be found in some drugs, illegal substances, and supplements. Serotonin syndrome can happen after taking certain medications, mixing medications with recreational drugs accidentally, or intentionally taking too much of a substance.
The impacts of serotonin syndrome can greatly vary. In some people, symptoms could be mild, but for others, it may be deadly. Common symptoms of this syndrome include changes in mental state, problems with bodily functions like heart rate and digestion, and muscle over-excitement.
Diagnosing serotonin syndrome can be tough as it is based on symptoms and can happen rapidly. The best way to diagnose it usually involves the Hunter criteria, which are a set of symptoms most commonly associated with the condition. Doctors would need to get a full medical history and look at your current medications to make a correct diagnosis.
Treatment for serotonin syndrome chiefly involves stopping the use of the drugs causing it and providing additional care as needed. Mild cases often go unnoticed and typically do not require hospital treatment. In contrast, severe cases usually require hospital care and may need specific drugs to counteract the serotonin toxicity. It’s common for serotonin syndrome to start within one day of a change in your medication routine, whether it’s from starting a new drug, changing the dosage, or using other substances.
Preventing serotonin syndrome comes down to being careful with your medications, especially those that increase serotonin levels, and seeking advice from healthcare professionals if you’re worried about possible interactions between your drugs.
What Causes Serotonin Syndrome?
Serotonin, also known as 5-hydroxytryptamine or 5-HT, is a brain chemical that plays various roles in our bodies. It’s mostly produced in our guts and peripheral nervous system, affecting our gut movements, uterus contractions, blood vessel narrowing, and airway constriction. Serotonin is also created in different parts of our body like skin cells, respiratory system’s neuroendocrine cells, and taste receptor cells on our tongue. Our blood platelets also store serotonin, which helps the platelets to clump together. However, the platelets need to absorb serotonin from the plasma as they can’t make it themselves. 90% of serotonin production comes from our gut, with 8% from platelets and 2% from our central nervous system (the brain and spinal cord).
In the brain, serotonin production starts in the brainstem part called the ‘raphe nuclei’. Axons (nerve fibers) from there extend to other brain areas. Some of these fibers reach the brain’s cortical and subcortical regions, affecting alertness, attention, mood, sexual behavior, body temperature, and appetite. Other fibers reach the spinal regions affecting muscle tone and pain sensation. When activated, our blood platelets release serotonin into the plasma, which then acts on various serotonin receptors.
Serotonin usually works through receptors that are located in the brain’s neurons. When serotonin is released, it’s taken up by the ‘serotonin transporter (SERT)’, a pre-synaptic neuron that moves serotonin back. Certain antidepressants stop SERT from moving serotonin, resulting in more serotonin being available to stimulate the receptors. When serotonin is taken back into the neuron by SERT, it can also be broken down by an enzyme called monoamine oxidase. Certain antidepressants can stop the breakdown of serotonin.
Several serotonin receptor types exist, named 5-HT1 to 5-HT7. An enzyme turns L-tryptophan hydroxylase into serotonin, which is stored in vesicles inside the neuron. Once released, it can stimulate the serotonin receptors. It’s then taken back up by the SERT transporter and then broken down into 5-HIAA (5-hydroxyindoleacetic acid).
There’s a variety of 5-HT subtypes, and each has its own roles, and different drugs target these. For example, Buspirone targets 5-HT1A, and Sumatriptan and Zolmitriptan for 5-HT1B and 5-HT1D to treat migraines. Then, most second-generation antipsychotic medications target 5-HT2A receptors. The 5-HT2C is targeted by weight-loss drugs, while the 5-HT3 receptor is targeted with anti-vomiting drugs. The 5-HT4 boosts gastric movements and is targeted by prucalopride to treat constipation. The roles of 5-HT5 are not fully understood, and so far, no medications target 5-HT6 or 5-HT7 directly. However, some antidepressants and antipsychotics can unintentionally affect these. An excessive stimulation of serotonin receptors can trigger a condition known as serotonin syndrome.
Risk Factors and Frequency for Serotonin Syndrome
Serotonin syndrome can affect anyone, regardless of age or gender. However, it’s difficult to know exactly how common it is. This is because it doesn’t happen often, mild cases might not be correctly diagnosed or reported, and many doctors are not familiar with the condition.
In the United States, the use of antidepressants that increase serotonin levels in the brain has gone up significantly over the last 20 years. The number rose from 6% of adults in 1999 to 10.4% in 2010. This rise has continued into the 2020s.
- Medical practices in the United States reported over 54,000 cases of harmful exposure to selective serotonin reuptake inhibitors (a type of antidepressant) in 2016 to the Toxic Exposure Surveillance System, an organization that collects data on such exposures.
- In the same year, 102 deaths were linked to these antidepressants.
- Compared to 2002 data, there was an 18% increase in cases and an 8% increase in deaths by 2016.
- A study of reports to the U.S. Food and Drug Administration’s system for tracking negative side effects found that nearly half of serotonin syndrome cases were related to the use of a single antidepressant that affects serotonin levels.
Signs and Symptoms of Serotonin Syndrome
Serotonin syndrome refers to a variety of symptoms that indicate a high level of serotonin in the body. This condition can be quite challenging to diagnose because its symptoms can resemble those of other health issues. However, doctors will rely on a detailed medical history and physical examination of the patient to make a diagnosis. Laboratory tests can also be useful in ruling out other health conditions that have similar symptoms.
For the patient’s history, it’s important to gather information on the use of any medications, supplements, or illicit substances, particularly if symptoms of serotonin syndrome are suspected. It can be difficult to get a reliable history if the patient’s mental state is altered, a common occurrence in serotonin syndrome cases. The information sought includes specifics about substance names, formulations, dosage, schedules, and any details concerning changes in medication or use of new substances. Onset of symptoms and how quickly they progressed are also crucial details to note. Usually, symptoms of serotonin syndrome appear within 6 to 24 hours after the change in dosage or introduction of a new serotonergic agent.
Special consideration is given when intentional overdoses of serotonergic substances are suspected. The symptoms tend to be more severe in these cases compared to accidental exposures. Therefore, healthcare providers need to ask directly if there was a premeditated intention to overdose.
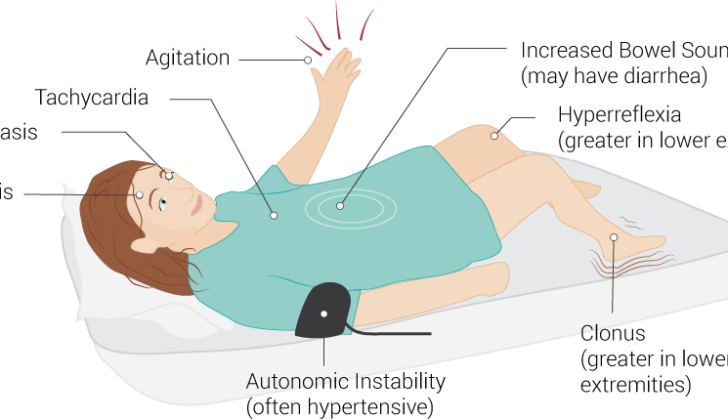
Physical examination plays a vital part in distinguishing serotonin syndrome from other health conditions with similar symptoms. While not all symptoms may be present in every case, common signs include:
- Fast heartbeat
- High blood pressure
- Fever due to serotonin toxicity affecting body’s temperature control
- Altered mental status (including agitation)
- Eye clonus (rapid, rhythmic eye movement)
- Dilated pupils
- Restlessness
- Tremors
- Deep tendon hyperreflexia (exaggerated tendon reflex)
- Inducible or spontaneous muscle clonus
- Muscle rigidity
- Positive Babinski sign (abnormal reflex)
- Flushed skin
- Excessive sweating
- Increased bowel activity
Neuromuscular symptoms are usually more pronounced in the lower extremities, with hyperreflexia and muscle clonus being the most common findings.
Testing for Serotonin Syndrome
While serotonin syndrome is diagnosed based on your symptoms and medical history, lab tests can help clarify the condition, measure its severity, and guide treatment. Typical lab results might show increased white blood cell count, decreased sodium bicarbonate, and increased creatine phosphokinase. In severe serotonin syndrome, lab tests may also reveal irregularities in blood clotting, muscle breakdown leading to elevated creatine kinase, and a disturbance called metabolic acidosis.
If you’ve intentionally taken too many drugs, doctors might also check your acetaminophen and salicylate levels as well the performance of your heart through an electrocardiogram. A CT scan of the head could be conducted to rule out any head injuries.
Several guidelines or criteria exist to diagnose serotonin syndrome, but the Hunter Toxicity Criteria Decision Rules are largely considered the most accurate. They correctly identify the condition 84% of the time and correctly rule it out 97% of the time.
The Hunter Criteria include a recent history of taking serotonergic drugs – drugs that affect the neurotransmitter serotonin in your brain – and having at least one of these symptoms:
- Spontaneous clonus (rhythmic muscle contractions)
- Inducible clonus (rhythmic muscle contractions that can be provoked) with agitation or excessive sweating
- Ocular clonus (rapid, rhythmic, back-and-forth movement of the eyes) with agitation and excessive sweating
- Trembling and a hyperactive reflex
- Muscle rigidity and body temperature over 100.4°F with ocular or inducible clonus
If you’ve been taking and tolerating a serotonergic drug for a while, it’s unlikely that you’ll suddenly develop serotonin syndrome. Thus, the criteria specifically look for recent changes, like starting or increasing the dose of a serotonergic drug; changes in your body that decreases how it metabolizes or processes the drug; overdosing on a serotonergic drug unless it’s a drug that specifically activates serotonin receptors; or negative interactions between the serotonergic drug and other drugs that you’re taking, unless these other drugs are direct serotonin receptor agonists.
Treatment Options for Serotonin Syndrome
If you’re told you have serotonin syndrome, it’s crucial to recognize the condition quickly and correctly. Identifying it can often be difficult, leading to misdiagnosis, which might make the situation worse. This syndrome commonly presents with unexplained fever, hence it’s not advised to continue with medications known as serotonergic agents if such symptoms occur.
The first step in controlling this syndrome is discontinuing all serotonergic agents. Serotonin syndrome is actually a form of drug poisoning, and stopping the medications involved should help clear it up. However, some of these medications, such as fluoxetine, can stay in your body for a long time, which means you might still feel sick for several days after you stop taking them.
Beyond stopping these medications, the patient should receive supportive care to help their body recover from the toxic effects of the drugs. This could include intravenous fluids and oxygen, monitoring heart function, and trying to stabilize the patient’s heart rate, blood pressure, and other vital signs. Intravenous fluids are particularly helpful in cases where the syndrome has caused a high body temperature.
With serotonin syndrome, a patient might be extremely restless and have continuous muscle contractions, which can make the high body temperature and other symptoms worse. As a result, doctors often use tranquilizing drugs to help calm the patient down. This is usually done with medications called benzodiazepines because they don’t interfere with serotonin or dopamine, both important brain chemicals, and can also help bring down a high blood pressure and fast heart rate. Diazepam is commonly used for this purpose.
The heart rate and blood pressure might both fluctuate rapidly in a patient with serotonin syndrome, due to a problem called autonomic instability. To manage this, doctors prefer using fast-acting medications like esmolol, nicardipine, or nitroprusside. Long-acting medications like propranolol are not advised because they might not be flexible enough to handle these fast changes.
One of the major complications of serotonin syndrome is a very high body temperature, or hyperthermia. The best way to bring this down is often sedation, which reduces the heat created by muscle activity. If the body temperature is extremely high, above 41.1°C (106°F), the patient might need to be put into a medically-induced coma and cared for in an intensive care unit. Standard fever-reducing drugs such as acetaminophen aren’t helpful because the high temperature isn’t due to a fever, but to the muscle activity and other effects of the syndrome. In serious cases, external cooling measures are used.
In some cases, if the patient isn’t improving with the previous measures, the doctor might decide to use an antidote called cyproheptadine. Cyproheptadine works in several ways, but mainly it counteracts the effects of serotonin, the chemical that is in excess in serotonin syndrome. It can also help to calm the patient down and promote sleep. This medicine is generally taken by mouth but can be given through a tube if necessary. Although it can be helpful, the evidence for its effectiveness is mixed.
What else can Serotonin Syndrome be?
Neuroleptic Malignant Syndrome and Serotonin syndrome are serious conditions that can result from certain psychiatric medications. Because they have some similar symptoms, it can be challenging to diagnose them correctly. However, a thorough examination of the patient’s history and physical state can help distinguish between the two. Serotonin syndrome is triggered by medications that affect the ‘serotonergic’ system, while Neuroleptic Malignant Syndrome is caused by medicines that block the ‘dopamine’ receptors, primarily antipsychotics. Hence, it’s crucial to know the patient’s medication history. The symptoms of Serotonin syndrome often appear within a few hours of a change in serotonergic medication, whereas neuroleptic malignant syndrome manifests more slowly, over days to weeks.
There are also differences in physical symptoms. Serotonin syndrome is marked by increased neuromuscular activity, often shown by symptoms like overactive reflexes, spasmodic jerks, and tremors. On the other hand, neuroleptic malignant syndrome results in a slowed neuromuscular response, usually observed as rigidity.
Both conditions improve once the offending medication is stopped. However, serotonin syndrome resolves quickly, typically within a day, while neuroleptic malignant syndrome takes longer—about one to two weeks. Both conditions can potentially lead to fever, confusion, elevated white blood cell counts, an increase in a muscle enzyme called creatine phosphokinase, and metabolic acidosis—a condition that happens when the body produces too much acid or when the kidneys can’t remove enough acid from the body.
Another life-threatening condition, malignant hyperthermia, can be confused with serotonin syndrome, as it can also lead to a high body temperature. However, this condition typically occurs after exposure to specific anesthetics or muscle relaxants and presents severe muscle rigidity.
Anticholinergic toxicity, another condition with overlapping symptoms, like high body temperature and confusion, usually occurs in the context of medications with anticholinergic properties. Some psychiatric medicines can have these properties, and it’s possible for a patient to have a mixed serotonin syndrome with anticholinergic toxicity, particularly after an intentional overdose of psychiatric medications. Anticholinergic toxicity can also cause dry mucous membranes, difficulties urinating, and decreased bowel sounds—in contrast, increased bowel sounds are common indicators of serotonin syndrome.
Lastly, alterations in one’s mental state, with or without restlessness, are common in many conditions, making it a nonspecific clinical finding. In the case of serotonin syndrome, these changes are often accompanied by neuromuscular hyperactivity—like tremors, spasmodic jerks, and overactive reflexes—which is uncommon in most other causes of confusion or delirium.
What to expect with Serotonin Syndrome
The outcome of what’s known as serotonin syndrome greatly depends on the level of serotonin toxicity. This toxicity can occur for a variety of reasons, including from the amount and specific type of drug that affects serotonin, a chemical in your body that helps your brain cells and other nervous system cells communicate with one another.
MAO-I’s, a type of medication that treats certain conditions by increasing the levels of serotonin in the brain, are often linked to the most serious cases. However, purposefully taking too much of any drug that affects serotonin can lead to serious symptoms. Lesser cases might just need to be watched closely, while more serious cases require intensive medical care.
After serotonin syndrome has resolved, it’s important to thoroughly review the person’s situation to evaluate the pros and cons of returning to the previous treatment plan that affects serotonin levels in the brain.
Possible Complications When Diagnosed with Serotonin Syndrome
Serotonin syndrome, a potentially dangerous condition caused by excess serotonin in the brain, can usually be treated rapidly and effectively when detected early. The time it takes for the person to recover depends on several factors, including the medicine responsible and how long it stays in the body. Once the person’s mental state has returned to normal, their vitals are stable, and they show no signs of nerve overactivity (like involuntary muscle spasms or overactive reflexes), they can usually be sent home
Healthcare professionals will then review and alter the person’s medicine as needed to try and prevent another occurrence of serotonin syndrome.
- Quick and safe resolution when treated promptly
- Recovery time is dependent on various factors, mainly the medicine causing the condition
- Discharge is safe once mental state and vitals have normalized, and there are no signs of nerve overactivity
- Medications are reviewed and adjusted to prevent another episode
Preventing Serotonin Syndrome
When a doctor prescribes a medication that affects serotonin (a chemical in your brain), they might not always mention the risk of something called “serotonin syndrome.” This condition is more likely to happen if you’re taking more than one medication that affects serotonin, but it can also happen with just one drug. So, it’s crucial for you to be aware of this risk anytime you start a new medication that affects serotonin.
Also, regular check-ups can help keep an eye out for any signs of serotonin syndrome. In particular, a neurological exam, which is a check-up of your nervous system, can swiftly spot any hidden signs of this condition. These examinations are particularly beneficial for patients taking medications that influence their serotonin levels.