What is Transtentorial Herniation?
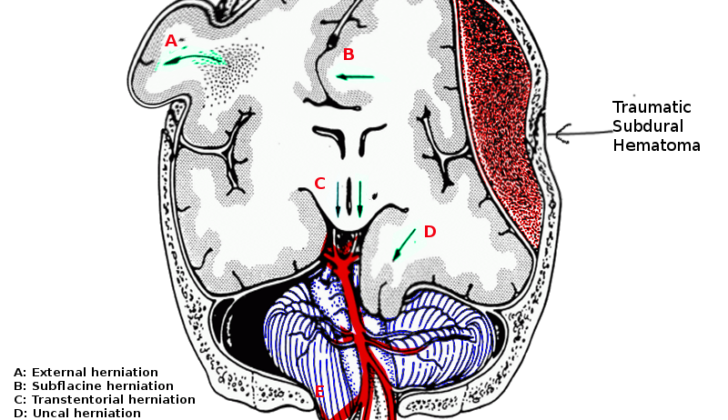
A brain herniation is when parts of the brain move into different spaces, or “compartments”, within the skull. The main compartments in the skull are the left and right areas above a tough, protective substance called the tentorium cerebelli, and the area below it, known as the posterior fossa. The tentorium cerebelli works as a divider, keeping the cerebellum and brainstem (located in the lower part of the brain) separate from the cerebral hemispheres (the large, upper part of the brain).
This divider also separates the cerebral hemispheres into left and right sections. These sections are separated by the falx cerebri, which is another protective fold located between the two hemispheres. The tentorium cerebelli also has an oval-shaped opening, known as the tentorial notch or incisor, that the midbrain passes through and connects with a part of the brain called the diencephalon.
A transtentorial herniation refers to any movement of brain tissue through the tentorial notch. There are three different kinds of these herniations: uncal herniation, central herniation, and upward herniation.
What Causes Transtentorial Herniation?
Increased pressure inside the skull (also known medically as intracranial pressure or ICP) can be caused by different issues, including:
* Hematoma, which is where blood collects outside of the blood vessels. This can happen in different parts of the brain and could be a result of a brain injury.
* Hydrocephalus is a condition where there’s too much cerebrospinal fluid (or CSF, which is the liquid that protects and cushions your brain and spine) in the brain.
* Tumors or abscesses (which are pockets of pus) can also increase pressure.
* Malignant ischemia like malignant middle cerebral artery syndrome. Ischemia means when there’s a lack of blood supply to a part of the body. So this syndrome would be a severe type of stroke that affects one of the main arteries to the brain.
* Swelling from an injury to the brain that causes widespread, microscopic damage to the nerve fibers – known medically as diffuse axonal injury.
* Pneumocephalus, which is where air gets into the cranial cavity. This could happen after a trauma or a surgery.
* Over drainage of the cerebrospinal fluid (the fluid that protects your brain and spine).
* Metabolic issues like hepatic encephalopathy, a condition where the liver disease affects brain function
* Tumefactive multiple sclerosis which is a severe form of multiple sclerosis which causes tumors or tumor-like lesions in the brain.
Risk Factors and Frequency for Transtentorial Herniation
Transtentorial herniation occurs as a response to different underlying health problems, so its exact rate of occurrence isn’t documented. However, its main cause is traumatic brain injury (TBI). In 2019, a review estimated that around 69 million people globally experience a TBI each year, with nearly 8% deemed severe. In the United States, about 30 million people need medical attention for a TBI annually.
- Transtentorial herniation doesn’t have a documented incidence rate because it’s a response to various health conditions.
- The primary cause is usually traumatic brain injury (TBI).
- A 2019 review estimates that globally, approximately 69 million people per year experience a TBI.
- Out of these cases, nearly 8% are considered severe.
- In the United States, about 30 million people require medical attention due to a TBI each year.
Signs and Symptoms of Transtentorial Herniation
Uncal herniation is a serious condition that causes an eye to become enlarged and unresponsive due to pressure on an eye nerve. It often results in some eye movement problems and a reduction in consciousness that makes it difficult to diagnose. Key symptoms like consciousness distortion and hemiplegia (paralysis of one side of the body) can occur on the same side or opposite side of the affected eye. Breathing usually remains normal, but patients may develop a pattern known as Cheyne-Stokes respiration.
This condition progresses in stages from early to late, each characterized by distinct symptoms. In the early stage, the affected eye’s pupil enlarges and reacts sluggishly to light. This stage also results in increased distortion of consciousness. The late stage features a completely dilated pupil that no longer reacts to light and potential paralysis. Finally, the last stage involves damage to the midbrain, making both pupils become fixed, and abnormal posturing may occur. At this point, uncal herniation becomes indistinguishable from central herniation.
Central herniation also progresses in stages. Early signs are progressive tiredness, behavioral changes, difficulty concentrating, or confusion due to the dysfunction of the arousal system. Typically, the pupil becomes small with slight light reaction. As the herniation progresses, the patient’s coma deepens, they lose motor localization to pain, and certain reflexes become prominent. Instances of paralysis and irregular pupil sizes can occur, leading to the loss of specific eye movements. In the terminal stage, breathing isn’t regular, heart rate slows down, and blood pressure fluctuates drastically, leading to potential cardiac arrest.
Direct pressure on the dorsal midbrain leads to the development of Parinaud syndrome, which sees the patient struggle with eye movement and enlarged pupils that won’t respond to stimuli. In severe cases, the patient’s eyes may be forced into a downward gaze. The patient may also develop a specific type of nystagmus, a condition that causes involuntary eye movement. If the passage through the midbrain becomes compressed, it may lead to obstructive hydrocephalus, symptomatic of reduced consciousness.
Testing for Transtentorial Herniation
The Glasgow Coma Scale (GCS) is commonly used to assess the level of consciousness in individuals with head injuries. But, some people argue that it may not be the most precise tool since different symptoms may result in the same GCS score. It turns out that the motor component of the GCS (observing a patient’s movement in response to stimuli) may be a more accurate way to determine the severity of a head injury.
In cases where a person shows signs of reduced consciousness, a brain scan like CT (Computed Tomography) is usually needed. It helps doctors see if there’s a structural problem in the brain that needs immediate surgery. Particularly, if a person has unequal pupils along with reduced consciousness, it indicates a high chance of a condition requiring urgent treatment.
A brain scan could show signs of a certain emergency condition called herniation syndrome, where parts of the brain move to areas they shouldn’t due to increased pressure inside the skull. This condition could also be suggested by other signs in the brain scan, like the displacement of certain brain structures or the presence of small areas of bleeding.
In cases where the posterior cerebral arteries (PCAs) are blocked, the brain scans might show signs of lack of oxygen supply to the areas supplied by these arteries. If there’s upward movement or herniation, the areas of the brain lacking oxygen are likely to be those supplied by other arteries located in the cerebellum, the part of the brain at the back of the skull. There might also be a condition called hydrocephalus, which involves an accumulation of fluid inside brain cavities known as ventricles.
Sometimes, a device might be installed to monitor the pressure inside the skull, which can provide valuable information about the patient’s condition. With herniation syndrome, this device will typically show high pressure measurements. It also graphs these pressure changes, and the shapes of these graph curves can indicate whether the brain is able to cope with any increases in pressure.
Yet, there’s ongoing debate about how helpful this pressure monitoring is. Evidence suggests that while it’s essential to control the skull’s inner pressure to achieve good outcomes in patients with traumatic brain injuries, monitoring might not always lead to better results. This is because patients with these devices tend to stay longer in critical care units and need more interventions, which sometimes leads to worse outcomes. Some studies have suggested that patients might achieve better results with treatments intended to lower pressure inside the skull without actually measuring it.
Another point for doctors to remember is the possibility of patients who initially seem fine after a head injury but then rapidly worsen into a coma. This scenario is often seen in cases involving extradural hematoma, a type of bleeding that occurs outside the brain but within the skull, which can quickly increase the pressure inside the skull.
Treatment Options for Transtentorial Herniation
When someone has a severe brain injury, one of the main ways we treat it is by controlling their intracranial pressure (ICP) – this is the pressure inside their skull. There are many ways we can do this: for example, by maintaining their oxygen levels and blood pressure, keeping their body temperature steady, treating any infections, and making sure they get enough food and fluids.
In brain injuries, it’s important to prevent things that could make the injury worse. Some of these measures are strongly supported by research:
– Keeping their blood pressure steady, because low blood pressure can double the risk of death.
– Giving anti-epileptic drugs can prevent seizures in the early stages after injury. However, they don’t seem to reduce the risk of seizures happening more than one week after the injury.
Other measures have moderate support from research:
– If the person’s score on a test called the Glasgow Coma Scale is 8 or less, we will secure their airway to make sure they can breath properly.
– We must avoid low oxygen levels in their blood. If oxygen levels are too low and blood pressure is low at the same time, this can triple the risk of death.
– We aim to keep the level of carbon dioxide in their blood at a certain level. If we ventilate them too much, this can actually make their outcomes worse, but sometimes we might do it temporarily if their neurological condition is getting worse rapidly.
Sometimes we may need to give medications that relax their muscles, but we try not to do this if we can avoid it. This is because these drugs can cause longer stays in the intensive care unit and increase their risk of getting pneumonia.
We can also give certain medications if there are signs that pressure in their brain is causing parts of their brain to be compressed. One sign of this can be changes in their pupil size. Mannitol and hypertonic saline can be used for this. However, these agents need to be used carefully because they can affect the volume of blood and other fluids in the body.
If a person has had a traumatic brain injury, they often have other injuries too. More than half of people with a severe brain injury will have injuries in other parts of the body, and some will have fractures in their spine. About a quarter of these patients will have a problem inside their skull that could be helped by surgery.
The surgery could involve making space for the brain by draining fluid, or it could involve removing a blood clot. Sometimes, a piece of the skull bone might be temporarily removed to give the swollen brain more space. This surgery, called a decompressive craniectomy, can save lives but doesn’t always improve the overall quality of life afterwards.
Timing of the surgery can make a big difference to the results. Research has shown that for certain types of brain injury, surgery needs to be done within a few hours of the injury to reduce the risk of death and improve the chance of a good recovery.
What else can Transtentorial Herniation be?
There can be several reasons why a person’s pupil might become dilated. One of these could be if an aneurysm (a bulge in a blood vessel) in an artery in the brain is pressing on the oculomotor nerve, which controls the movement of the eye. Certain medical conditions that cause neuropathy (nerve damage), such as diabetes, can also lead to problems with pupil function. However, in these cases, people usually remain conscious.
There are also many reasons why someone might have decreased consciousness or fall into a coma. This can be due to conditions that affect the brain, such as metabolic or infective encephalopathy (brain damage). However, these conditions usually wouldn’t result in one pupil becoming dilated. Although conditions that affect large areas of the brain’s cortex or thalamus can cause changes to pupils, these changes typically affect both eyes. Seizures can also bring about changes in pupils, but these changes are usually temporary.
What to expect with Transtentorial Herniation
A transtentorial herniation is a critical medical condition that can potentially be reversed through medical treatments and surgical procedures. This condition can become fully reversible if it’s identified and treated before it starts affecting the brainstem. This is especially true in cases that involve buildup of blood outside the brain layers, such as extradural and subdural hematoma.
In such scenarios, having a surgical procedure to remove the excess blood or to reduce the size of a tumor urgently done is very important. So, the sooner the condition is diagnosed and temporary treatments are started, the better.
However, once this condition affects the midbrain and the lower part of the brainstem, the chances for the patient’s neurological condition to improve or reverse become increasingly slim. This is usually a result of irreversible reduction in blood supply to the brain. At this stage, less than 5% of patients make a full recovery. Once the condition gets to the point where it’s affecting the patient’s ability to breathe, the chances of a meaningful recovery are practically none. At this point, it’s usually not appropriate to use machines to help the patient breathe. It’s now time for heartfelt conversations with the family and discussions about organ donation.
In a review of 153 patients, patients who were in a coma, had fixed pupils, and showed abnormal body movements only had a good recovery in 9% of cases. 60% of them didn’t survive, and 10% were diagnosed as severely disabled when they were checked up again later. Hence, the younger the patient, the more likely they have a better outcome.
Possible Complications When Diagnosed with Transtentorial Herniation
Secondary brain injuries, such as herniations, can occur alongside primary brain injuries. Primary brain injuries are those that occur at the moment of impact and are irreversible, often leading to severe outcomes. These injuries can vary in severity and can even affect the visual system. In fact, about 5% of individuals with head injuries experience some sort of visual damage, including cortical blindness due to pressure on the posterior cerebral artery. In rare cases, when someone has a central herniation, damage to the pituitary stalk can happen, causing a malfunction of the pituitary gland. This is especially noted when there’s a fracture at the base of the skull.
Common effects of traumatic brain injury:
- Secondary brain injuries like herniations
- Primary, irreversible brain injuries
- Varying degrees of visual system injury
- Visual damage, including cortical blindness
- Pituitary stalk damage leading to pituitary dysfunction
Preventing Transtentorial Herniation
TBI, standing for Traumatic Brain Injury, is the most common reason for a condition called transtentorial herniation, where part of the brain shifts from its normal position through an area called the tentorium. This often occurs as a result of instances like road accidents. As such, it’s really important for public health to take steps in reducing such traumatic events to lower the occurrence of this brain condition.