What is Angular Chelitis?
Angular cheilitis (AC) is a term used to describe an inflammatory skin condition that affects the angles of the mouth. The word “angular” refers to a specific inflammation of the lips that occurs at the corners of the mouth, which is different from other types of lip inflammation caused by various factors. The corners of the mouth are where the skin of the face and the inner lining of the mouth meet. This area moves a lot and experiences more pulling forces compared to the rest of the lips. As a result, it’s more prone to certain stresses.
There are other types of lip inflammation, known as diffuse cheilitides, which can be caused by environmental, chemical, or infectious factors, or may reflect an internal health issue or deficiency. These include conditions like eczematous cheilitis, contact cheilitis, drug-induced cheilitis, infective cheilitis, actinic cheilitis, glandular cheilitis, granulomatous cheilitis, exfoliative cheilitis, plasma cell cheilitis, and nutritional cheilitis. However, we won’t discuss diffuse cheilitides in this explanation.
Angular cheilitis has several other names, such as angular cheilosis, angular stomatitis, commissural stomatitis, rhagades, or perleche (which is French for “through licking”). The term rhagades generally refers to skin cracking in areas that move a lot, especially at the corners of the mouth and nose.
What Causes Angular Chelitis?
Various changes in the structure of your mouth can alter the closing of your lips and cause increased saliva buildup and skin softening at the corners of your mouth. These changes can be due to:
* The normal loss of skin firmness because of aging, smoking, or quick weight loss
* Changes in facial structure due to severe tooth wear, loss of teeth, and poorly fitted dentures which increase the upper lip overhang onto the lower one
* Incorrect jaw alignment
* Deepening wrinkles around the corners of the mouth
* Conditions associated with larger lips such as oro-facial granulomatosis (OFG)
* Down syndrome, which may cause an enlarged tongue and drooling
Atopic Dermatitis
Contact dermatitis caused by allergies or irritants causes up to 22% of cases of Angular Cheilitis (AC). This may be due to nickel (found in braces), food (due to flavorings and preservatives), toothpaste, mouthwash, expired lip balm, cosmetics (due to preservatives and other ingredients), acne products, and chewing gum.
Immune deficiencies can also cause AC, often through the development of a type of mouth infection known as oral candidiasis or thrush. Conditions like chronic use of steroids, HIV/AIDS, and certain blood disorders and malignancies can lead to immune suppression and increase the risk of AC.
Nutrition deficiencies, though less common in developed countries, also contribute to AC. This might occur in certain groups, such as the elderly, people with coeliac disease, the poor, vegans, and babies who are solely breastfed without vitamin supplementation.
People with immune conditions like Sjogren Syndrome and Inflammatory Bowel Disease can also have conditions like AC. Sjogren syndrome is a disease characterized by a dry mouth and decreased salivation, while Inflammatory bowel disease can contribute to AC due to nutrition deficiencies.
Infections are also a leading cause of AC and certain organisms can be found in over 50-80% of cases. This is because of increased exposure to infection-causing microbes or factors that increase skin flora such as poor hygiene, oral thrush, gingivitis, diabetes, among others.
Repeated injuring of the corners of the mouth from mechanical, chemical, and thermal factors or having chronic dry mouth can also lead to AC.
If you have AC without any identifiable cause, you might need to consider nutritional deficiencies or even the possibility of a malignancy. In rare cases, a pancreatic tumor called glucagonoma can cause AC.
Risk Factors and Frequency for Angular Chelitis
Angular cheilitis (AC) is a type of bacterial or fungal infection that affects the lips. It’s fairly common, affecting about 0.7% of people in the U.S. However, it can occur more often in certain groups. The condition primarily affects children and adults aged 30 to 60. Interestingly, AC is found in 11% of older adults, with those who wear dentures being three times more likely to develop the condition. In fact, among denture wearers, the condition can be as prevalent as 28%. Additionally, men seem to be twice as likely to develop AC, but these figures are mainly influenced by denture use and other health conditions, rather than age.
People with weakened immune systems are also at risk. For example, up to 10% of people living with HIV may develop oral thrush and AC as well. People with inflammatory bowel disease (IBD), such as Crohn’s disease and ulcerative colitis, also have a higher chance of developing AC – 7.8% and 5% respectively. Even in rare conditions like orofacial granulomatosis, AC can occur as often as in 20% of cases.
Signs and Symptoms of Angular Chelitis
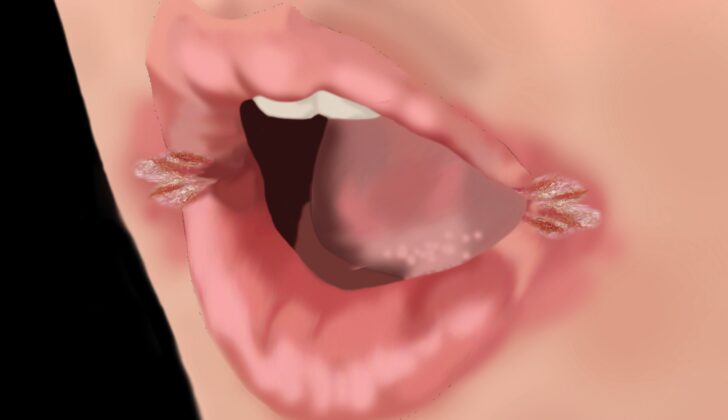
Angular cheilitis is a type of inflammation that causes red, swollen, sometimes painful patches of skin at the corners of the mouth. The condition has different levels of severity, ranging from mild cases where the lips are normal or a little chapped and the affected areas may appear pinkish-red, to severe cases where the skin can bleed and have crust build-up. The inflamed skin can look bluish or white and be covered by a flaky skin. If angular cheilitis is caused by bacteria, it might have a honey-colored exudate, pustules, or oozing pus.
The inflammation usually just affects the corners of the mouth and rarely spreads to the nearby facial areas or lips. If it does spread beyond the border of the lips, it forms fissures (cracks in the skin) that follow the natural lines on the face, typically made by salivary flow. Angular cheilitis frequently affects both corners of the mouth equally unless there’s another risk factor that affects one corner more than the other. If the condition appears more on one side than the other without a clear cause, this could be a sign of less common causes.
It’s always important to check the mouth for thrush (oral candidiasis) when examining angular cheilitis, and treat it if present. Oral candidiasis can have several formations:
- Acute or chronic pseudomembranous (thrush) – white, defined patches on the inside cheeks, tongue, palate, and uvula; spots may turn red and sometimes bleed when scraped off
- Acute or chronic atrophic or erythematous patches and plaques – large, diffuse, clearly outlined, on the palate and tongue that can be associated with soreness
- Chronic hyperplastic nodules or plaques – hard, leathery, non-removable lesions on the inner cheeks, palate, tongue, and corner of the mouth; they can also extend to the skin and nails.
There are a number of conditions associated with angular cheilitis along with other symptoms such as:
- Vitamin B2 deficiency: Can lead to angular cheilitis, sensitivity to light, magenta glossitis (inflammation of the tongue), mouth inflammation, throat, inflammation, and seborrhea-like dermatitis of certain body parts. This deficiency can impair iron absorption, leading to a type of anemia.
- Vitamin B3 deficiency: Symptoms can include skin inflammation, diarrhea, dementia, glossitis, and angular cheilitis.
- Vitamin B6 deficiency: This can result in angular cheilitis along with a range of conditions including anemia, depression, elevated blood pressure, and high homocysteine levels.
- Zinc deficiency: Symptoms can include mouth ulcers, hair loss, diarrhea, dermatitis, and angular cheilitis.
Testing for Angular Chelitis
The most common cause of angular cheilitis (AC), a condition characterized by red, swollen patches in the corners of the mouth, is infection. Usually, this diagnosis is made just by examining the affected area, but laboratory testing can be useful, particularly if initial treatments aren’t working.
In some cases, the doctor might decide to investigate for contributing underlying medical conditions. This could include issues like nutritional deficiencies, an immune system that’s not working properly, or systemic diseases. If the AC doesn’t get better after 2-3 weeks of standard antifungal and antibiotic treatment, the doctor might arrange further tests. These tests could check the levels of substances like hemoglobin (Hgb), mean corpuscular volume (MCV), iron, ferritin, folate, and vitamins B2/B6/B12, along with testing for diabetes by checking fasting blood glucose levels.
If it’s suspected that a Candida infection (a type of yeast) is causing the AC, a sample can be taken from the sore area and looked at under a microscope. The sample can be treated with a variety of techniques to help highlight whether there are any infectious cells (known as hyphae) indicative of a Candida infection. There are also a number of other methods your doctor can use to test for Candida, including various types of cultures and tests.
If a bacterial infection is suspected, a sample can be sent off to the lab to identify the specific bacteria involved, and to determine which antibiotics it is likely to respond to.
Your doctor might suggest other investigations depending on context. For instance, if oral candidiasis (a fungal infection in the mouth) is confirmed, tests for HIV or diabetes might be arranged. If a nutritional deficiency is suspected, then blood and urine tests could be done to assess levels of important nutrients. Patch testing can diagnose allergic dermatitis, a skin reaction caused by an allergy. Lastly, if your doctor is worried about the possibility of cancer, they might arrange a biopsy, where a small sample of the affected area is removed and examined under a microscope.
Treatment Options for Angular Chelitis
Treatment for a condition depends on whether or not it was caused by an infection. A common approach is to address the infection first, as this is often the root cause. In many cases, the key to smoother, healthier lips is keeping them moisturized with lip balm or petroleum jelly. These simple measures are often enough to relieve the condition in cases of oral yeast infection that have no identifiable cause.
For yeast infections, fungicidal, or anti-fungal, medications can help alleviate symptoms. These medications are applied to the corners of the mouth usually three times a day for two weeks.
If a bacterial infection is present, it might be necessary to use topical antiseptics or antibiotics. In cases where there is a recurrent infection due to bacterial presence, it is advised to apply the chosen medication to the front part of the nostrils for 1 to 2 weeks. This can prevent the infection from recurring.
On rarer occasions, it might be necessary to take oral antifungal treatments, especially in cases of severe oral yeast infection. Some of these systemic or body-wide antifungals can avoid the need for topical treatment, but they may interact with other medications due to their mode of action in the body (via inhibiting the hepatic cytochrome P450 system). Fluconazole is most commonly used because of its documented effectiveness.
Oral antibiotics might be required for more extensive cases or when the topical ones don’t work. If this happens, it is recommended to have bacterial culture and sensitivity tests and reevaluate your diagnosis to ensure the accuracy of the treatment plan.
Topical glucocorticoids, drugs that reduce inflammation, are another option for severe inflammatory cases or as an additional treatment to antifungal or antibacterial products. They can help decrease inflammation, promote healing, and prevent recurrence.
In cases connected to vitamin deficiencies or general malnutrition, it might be necessary to seek nutritional supplementation or replacement.
Having your dentist adjust misfitting dental fixtures (like dentures) is crucial to restoring your facial contour. Dentures can serve as a potential reservoir for Candida (the fungus which causes yeast infections), therefore, they should be treated with an antifungal agent and cleaned regularly. Dental realignment may also be necessary in some situations.
Sometimes people have depressions at the corners of their mouths that can be filled with injectable fillers or surgical implants to reshape the mouth. Usually, these treatments are administered by an experienced physician since this is a more complex procedure compared to the regular application of fillers.
Patients may also need to manage chronic medical conditions more effectively. For instance, better blood sugar control in individuals with diabetes and antiretroviral therapy in those with HIV/AIDS have been shown to reduce instances of oral yeast infection.
You may also find that the following habits can lead to an oral yeast infection: smoking and lip-licking. Consequently, cutting down on these habits can often lead to a decrease in oral yeast infections.
Despite treatment, there can occasionally be failures of therapy. These can result from not correctly identifying or treating oral yeast infection, or the presence of Candida species or bacterial strains that are resistant to the medications used. Other causes can be failure to address any underlying risk factors that can be changed, such as poor oral hygiene, mal-fitting dentures, or some behaviors. Systemic conditions that might have remained unaddressed, such as nutritional deficiencies, systemic inflammatory conditions or immune suppression, or an undiagnosed cancer, can also contribute to treatment failure.
A follow-up is recommended after 2 weeks of treatment.
What else can Angular Chelitis be?
When diagnosing certain mouth and lip conditions, doctors may need to consider several potential causes. These could include the following:
- Secondary syphilis or a syphilis sore that’s focused on the corner of the mouth, usually affecting one side
- Painful inflammatory conditions such as oral lichen planus or similar lesions in the mouth
- A skin infection caused by bacteria known as impetigo
- Skin conditions such as atopic dermatitis and seborrheic dermatitis
- Allergic reactions causing inflammation of the lips (Allergic contact cheilitis)
- Local irritation causing inflammation of the lips (Irritant contact cheilitis)
- Earlier stages or widespread inflammation of the lips (diffuse cheilitis)
- Sun-related lip damage, especially on the corners of the mouth if not protected by lip balm with sun protection (Actinic cheilitis)
- Conditions causing lip swelling (Cheilitis glandularis)
- Conditions causing lip swelling, usually due to a chronic inflammatory disorder (Cheilitis granulomatosa)
- Condition causing the lips to peel and become raw (Exfoliative cheilitis)
What to expect with Angular Chelitis
Angular cheilitis (AC), a condition that affects the corners of your mouth, is generally easy to treat and typically doesn’t pose a serious threat to your life or cause lasting disfigurement. With successful treatment, you can expect to see improvement within the first few days and complete resolution usually by two weeks. Because of this, your doctor will likely want to see you for a follow-up around the two week mark.
However, it’s worth noting that in some cases, AC might cause some skin changes at the corners of your mouth, like thinning or ‘granulation’, which is a kind of skin roughness. According to a 5-year study, AC tends to come back in about 80% of cases.
To prevent it from recurring, it’s essential to identify and manage any underlying causes. Sometimes these causes can’t be changed, or they might not be addressed, or the initial treatment for AC might not be fully completed. In those scenarios, AC commonly comes back. A repeated occurrence often happens when oral thrush (a type of mouth infection) isn’t spotted and treated, or when oral and denture hygiene stay poor.
For those who face frequent recurrences, your doctor might extend treatment beyond two weeks and include prevention tactics like applying moisturizing creams or anti-fungal treatments regularly.
Possible Complications When Diagnosed with Angular Chelitis
If angular cheilitis, which is a condition affecting the corners of the mouth, is not treated for a long time, it can lead to tissue loss and permanent scars or changes in skin color.
Preventing Angular Chelitis
In a study by Simons and colleagues, it was found that gum containing xylitol or a mix of chlorhexidine acetate and xylitol reduced AC, a type of mouth infection, in individuals over 60 years old. AC, also known as oral thrush, is a common infection caused by a yeast-like fungus and it often appears as white patches in the mouth.
If you have been diagnosed with AC due to allergic contact dermatitis, it’s important to avoid the allergen triggering your allergy to prevent further inflammation. Allergic contact dermatitis is a skin reaction caused by contact with substances your body is allergic to.
For those who have COPD (chronic obstructive pulmonary disease) or asthma and are taking inhaled corticoid steroids, rinsing your mouth out after administration can lower the chance of getting oral thrush. These steroids can alter the balance of natural organisms in your mouth leading to an overgrowth of yeast.
Persons who frequently get bacterial AC may find relief from using mupirocin or bacitracin to clear their nostrils of staph and strep bacteria. These bacteria are often found in the nose and can contribute to infections.
Dentures can be a hidden source of infection including AC, so proper cleaning and maybe even overnight soaking in hypochlorite or chlorhexidine, chemical disinfectants, can be a great help. Hypochlorite is commonly used for disinfecting and chlorhexidine is often used in mouthwashes to kill germs.
If dentures are a major risk factor, it’s crucial to see your dental specialist quickly. Dentures that poorly fit can inflame the gums, promoting the growth of yeast.
People with no natural teeth, and those with weakened immune systems, might prevent AC by using barrier ointments, like petroleum jelly and zinc oxide, or a daily imidazole cream. These substances protect the mouth’s surfaces and interfere with the growth of yeast.