What is Granuloma Inguinale (Donovanosis)?
Donovanosis, also known as “granuloma inguinale,” is a long-term and advancing infection caused by bacteria in the genital area. Genital sores linked to Donovanosis were first noted in India by a person named McLeod. The bacterium causing the disease was discovered by Donovan, who also identified Donovan bodies, the specific cells involved in this infection.
What Causes Granuloma Inguinale (Donovanosis)?
Donovanosis is a condition caused by a specific type of bacteria known as Klebsiella granulomatis comb. nov. This bacteria, which is categorized as ‘Gram-negative’, was initially called Calymmatobacterium granulomatis. However, the naming of this bacteria has been a topic of discussion among experts.
Fascinatingly, this bacteria was originally identified and named by researchers named Aragao and Vianna in Brazil. Later, it was discovered that it shared similarities with other bacteria in the Klebsiella family, based on different testing outcomes, structural features, and the way it appears under a microscope.
In 1999, Carter and his team decided to reclassify this bacteria from the original Calymmatobaacterium to Klebsiella, based on the study of specific genes called 16 SrRNA and phoE. To describe it more simply, the K. granulomatis bacteria are seen as small rod-shaped (coccobacillus), which means they are a bit of a mix between spherical (coccus) and rod-shaped (bacillus) bacteria. They live inside cells, they are wrapped in a protective layer (encapsulated), and can function in environments with or without oxygen (facultative aerobe).
The first effective treatment for Donovanosis took place in Brazil using a substance called emetic tartar. The first successful growth of this bacteria in a laboratory was achieved in the mid-1990s. This was done through the use of certain blood cells known as peripheral blood monocytes alongside human skin cells.
Risk Factors and Frequency for Granuloma Inguinale (Donovanosis)
There is some confusion about how donovanosis spreads as it seems to be linked with sexual contact, but there are known incidents where the disease spread without any sexual contact. Since 1947, most people have considered it a sexually transmitted infection based on certain studies at the time. Often, people with donovanosis remember some sexual contact prior to the appearance of symptoms. Furthermore, the disease is more common among sexually active age groups, particularly those between 20 and 40 years. Women with donovanosis usually have signs on their cervix, and men who have sex with men often have a higher occurrence of similar signs around the anus.
However, there are some clues that donovanosis may not only spread through sexual routes. For instance, it’s seldom seen in sex workers, and there have been reported cases of infection through fecal routes and nonsexual routes in children. Case stories mention children contracting the disease by sitting on the laps of infected adults, and babies getting the infection during vaginal birth. Other factors that may increase the chances of getting donovanosis include low cleanliness habits and being part of a low socio-economic group. Overall, the transmission rate of donovanosis is considered to be low.
In one study, two children were found to have donovanosis without any history of sexual exposure. In one case, an 8-month-old girl had a mass and discharge in her right ear; she had been treated with antibiotics and a small surgery, but came back 8 months later with more symptoms and a new brain abscess. She underwent brain surgery to drain the abscess as well as a mastoidectomy, and a tissue sample analysis confirmed that she had donovanosis.
Another case involved a 5-month-old boy with discharge from his left ear, a cranial nerve palsy, a mass at the external auditory meatus, and an abscess behind his ear. The mass was removed surgically, and the tissue sample confirmed the diagnosis of donovanosis. Again, no sexual abuse was noted.
Granuloma inguinale is rarely seen in the United States – about 100 cases are reported each year. Globally, the disease is more common in tropical and subtropical climates like New Guinea, Southern India, Southeast Asia, Brazil, Indonesia, Argentina, and the Caribbean. Australia and South Africa also used to have higher cases, but they are no longer high prevalence regions.
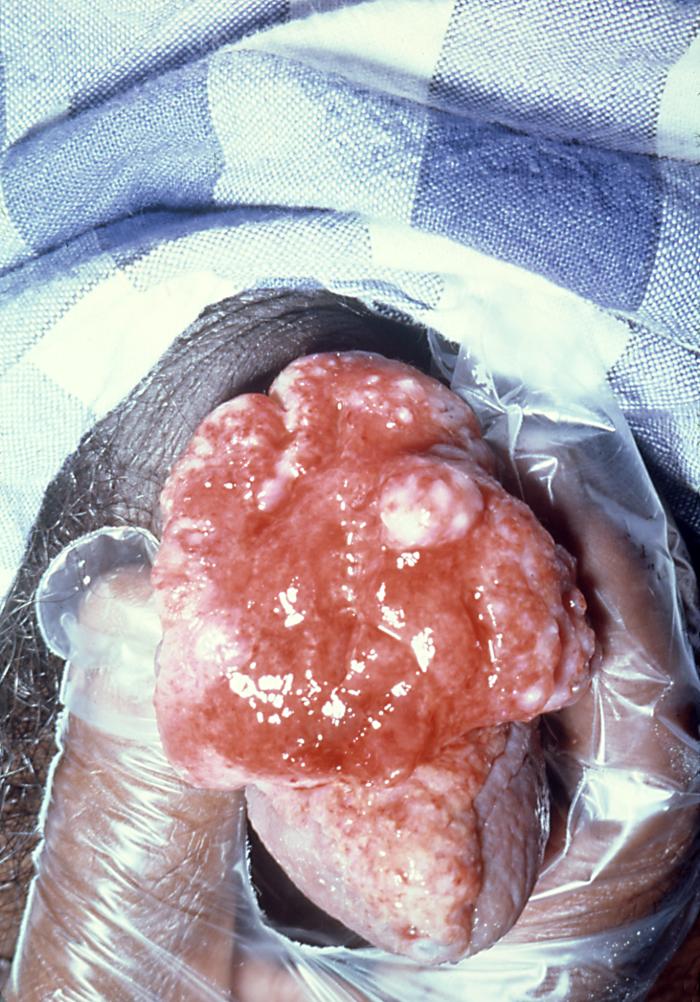
exhibited an ulcerative lesion, diagnosed as granuloma inguinale. However, due
to its appearance, it initially appeared to be carcinoma. Granuloma inguinale,
also known as donovanosis, is a sexually transmitted disease caused by the
bacterium Klebsiella granulomatis, formerly Calymmatobacterium granulomatis.
Signs and Symptoms of Granuloma Inguinale (Donovanosis)
Donovanosis is a condition where lesions, or damage in the skin or other body tissue, initially appear as a painless small raised spot or lumpy area under the skin. As they grow, these lesions develop a striking “beefy-red” color due to a high concentration of blood vessels, and they tend to bleed easily. After minor injuries, these spots often turn into sores. These lesions typically don’t come with swollen lymph nodes, but they can lead to the formation of lumpy lesions known as pseudobuboes under the skin.
The lesions tend to spread outwards from the center and have borders often described as having a “snake-like” appearance. If a person spreads the bacteria that cause the lesions to another part of their body, it may result in similar lesions appearing, often across skin folds. People often put off seeking medical attention, which causes them to come in with more advanced lesions.
Most of the time (90%), these lesions affect the genitals, and in 10% of the cases, they affect the inguinal region (the area surrounding the groin). In men, the most common sites of affliction are the skin covering the tip of the penis, the rim of the penis head, the strip of skin connecting the foreskin, the penis head, and the anus. In women, the most common sites are the inner folds of the vulva, the area of skin between the anus and the vulva in women, the cervix, and the upper part of the female reproductive tract. Lesions in pregnant women tend to progress faster and respond slower to treatment than in non-pregnant patients.
These lesions can also appear outside the genital area, such as on the lips, gums, cheek, palate, throat, voice box, and chest, though this is less common (6% of cases).
There are four types of lesions that can occur:
- Classic ulcerogranulomatous lesions: Most common and characterized by beefy-red, painless sores that bleed easily.
- Hypertrophic or verrucous lesions: Characterized by irregular raised edges and a dry texture.
- Necrotic lesions: Characterized by a foul-smelling, deep sore that causes tissue destruction.
- Sclerotic or cicatricial lesions: Marked by fibrous and scar tissue.
Testing for Granuloma Inguinale (Donovanosis)
In parts of the world where a certain condition is common, an experienced doctor can usually make a diagnosis fairly easily. However, in other areas, identifying this condition might require a bit more investigating. This could be the case with granuloma inguinale, a sexually transmitted infection.
If there’s a painless, red sore that bleeds easily in or around the genital area, it might suggest granuloma inguinale. This is especially true if other more common conditions have been ruled out.
To confirm this condition, doctors look for something called Donovan bodies, which are a kind of bacteria, in a tissue sample from the sore. There’s also a type of test called a PCR (polymerase chain reaction) that can detect the presence of the bacteria’s DNA, but it’s not widely available outside of research settings and certain public health programs.
Moreover, there are blood tests that can check for the bacteria, but they aren’t precise enough to diagnose an individual—they’re better suited for studying larger groups of people.
Treatment Options for Granuloma Inguinale (Donovanosis)
The Centers for Disease Control and Prevention (CDC) recommend that treatment for donovanosis, a sexually transmitted infection, should continue until all sores have fully healed. The first-choice treatment generally involves the drug azithromycin, and this continues until the disease is under control, but repeated episodes can happen 6 to 18 months after the first treatment that seemed successful.
Other medications that might be used include doxycycline, ciprofloxacin, erythromycin, and sulfamethoxazole with trimethoprim. These are alternatives to azithromycin. If a patient’s reaction to treatment is slow, they may also be given a drug called gentamicin. Erythromycin is the preferred choice for pregnant women. These recommendations stand the same for patients who also have HIV (Human Immunodeficiency Virus).
The European Guidelines issue in 2016 recommend that the use of antibiotics should go on for at least three weeks and until all symptoms have disappeared. The guidelines also suggest azithromycin as the first choice of treatment. For children with the disease or if they were exposed at birth, azithromycin should be used for three days for prevention.
A study conducted in Australia from June 1994 to March 1995 showed that azithromycin is effective in treating donovanosis. It may be given once a week for a month or once a day for a week. After six weeks, a few of the patients were healed, and everyone else saw a significant improvement. Azithromycin has the advantage of intermittent dosing, which may make it easier to use in areas where the disease is common.
Donovanosis may be treated with medications only. But if the disease has caused extensive tissue damage, surgery might be required. It is important to routinely check patients for the disappearance of the disease and for possible recurrence.
What else can Granuloma Inguinale (Donovanosis) be?
When someone has sores or ulcers in their genital area, there could be many possible causes. Doctors would consider a range of conditions, including:
- Syphilis
- Chancroid (a bacterial infection)
- Lymphogranuloma venereum (an infection caused by a type of Chlamydia)
- Genital herpes
- Cancer (neoplasm)
- Amoebiasis (a parasite)
- And other conditions
Because the risk factors for many of these diseases are similar, it’s also possible for a person to have more than one of them at the same time – this is called a coinfection. If the sores look particularly destructive or severe, the doctor should check for cancer as well as other causes. Donovanosis, a sexually transmitted infection, could lead to a condition that looks like lymphogranuloma venereum.
Women who have sores on their cervix should be tested for cancer and tuberculosis. It’s also important to test for HIV if a person is diagnosed with donovanosis, because this condition can increase the risk of HIV transmission. In fact, anyone diagnosed with a sexually transmitted disease should be considered for HIV testing.
What to expect with Granuloma Inguinale (Donovanosis)
If donovanosis, a sexually transmitted infection, is treated properly, patients usually have a good outcome. However, the infection might come back even when it seems like it’s gone. If there’s no improvement, doctors need to carry out further tests because it might mean there’s another infection or different illness present.
If it’s not treated, it can lead to severe scars and tissue damage. Additionally, an untreated donovanosis infection might turn into cancer. Therefore, seeking timely medical assistance and adhering to the treatment plan is crucial.
Possible Complications When Diagnosed with Granuloma Inguinale (Donovanosis)
There are several potential complications that can arise, such as:
- Spread of infection through the bloodstream
- Osteomyelitis, an infection in the bone
- Cancerous changes
- Polyarthritis, inflammation of five or more joints
- Pseudo-elephantiasis, abnormal swelling of tissues
- Narrowing of the urethra, vagina, or anus
- Vaginal bleeding
Additionally, an uncommon but serious complication is the spread of the disease into the abdominal cavity. Symptoms of this can include fever, general discomfort, anemia, night sweats, weight loss, and a severe body-wide infection known as sepsis.
Patients who have dealt with this disease for a long time may also experience emotional distress, as the symptoms can be both embarrassing and upsetting. It is important to consider that these patients may also have associated mental health problems, such as anxiety or depression, and it’s crucial to check for any potential thoughts of suicide.
One known case described a woman who experienced significant vaginal bleeding as a result of the disease. She arrived at Rajaji Hospital in Madurai, showing symptoms such as white vaginal discharge and abnormally long menstrual periods. Doctors found ulcers in her cervix and vagina, some which were covered with decayed tissue. After switching from one medication to a more tolerable one, her condition improved considerably. Her symptoms completely subsided two months later and she remained symptom-free after a year.
Another case involved a woman who presented to the same hospital, this time with pregnancy-related bleeding. She was found to have an ulcer growth in her vagina that looked similar to a cauliflower. Following treatment, her body responded well and her symptoms nearly disappeared after one month.
It’s also important to note the case of a man who showed a serious transformation of his symptoms. Despite being treated, a test revealed he had squamous cell carcinoma – a type of skin cancer. His initial symptom had been a sore on the penile head, which had been present for four years.
Preventing Granuloma Inguinale (Donovanosis)
The Centers for Disease Control and Prevention (CDC) suggests that everyone who has been sexually involved with a person suffering from granuloma inguinale within the two months before they started showing symptoms, should get a medical check-up and possibly treatment. However, it’s still not clear whether treating these individuals, who don’t show any usual signs or symptoms of the disease, with a trial method called ’empiric treatment’ is beneficial or not.












