What is Hemangioma (Strawberry Marks)?
Hemangiomas, also known as infantile hemangiomas (IH), are the most common non-cancerous tumors found in infants. They’re many times referred to as “strawberry marks” because of how they look. They occur when the cells that line blood vessels grow very quickly. There are various types of hemangiomas. Some hemangiomas can be seen at birth, while others might appear later during the infant’s first year. The typical course for these later-appearing hemangiomas is a fast growth phase followed by a gradual shrinking phase.
What Causes Hemangioma (Strawberry Marks)?
Doctors aren’t completely sure why infantile hemangiomas, a common type of birthmark that appears at birth or in the first or second week of life, develop. However, there are a few theories. One popular theory suggests that a lack of oxygen increases the production of GLUT 1 and VEGF, proteins involved in growing new blood vessels. This process could activate certain early-stage cells, known as endothelial progenitor cells, marked by proteins like CD133 and CD31.
Another theory proposes that cells from the placenta might be a source of stem cells – cells that can serve as a repair system for the body – that lead to hemangiomas. Yet another theory believes that these birthmarks form from both entirely new blood vessels, and from the sprouting of existing ones. This is a process known as vasculogenesis and angiogenesis, respectively.
In addition to these theories, some suggest that angiogenic factors, substances that aid in the formation of new blood vessels, act on the cells lining the blood vessels and accompanying cells called pericytes. Together, they could start the formation of a capillary network or a web of tiny blood vessels, which is a key characteristic of a hemangioma.
Risk Factors and Frequency for Hemangioma (Strawberry Marks)
Infantile hemangioma is a common non-cancerous tumor in babies, affecting around 4% to 5% of newborns. It’s caused by an unusual bunch of small blood vessels that appear during the baby’s first year of life. The condition is more common in Caucasian babies and is seen more in girls than boys, with a female to male ratio as high as 5:1.
- Infantile hemangiomas are more likely in premature infants or those with low birth weights.
- Babies born to older mothers or babies who didn’t get enough oxygen before birth are also more prone to develop these tumors.
- The condition is often seen in multiple births such as in twins or triplets.
- It’s also more common in cases where an early pregnancy test called a chorionic villus sampling has been done.
- Most cases happen randomly, but it’s also been seen as a condition that can run in families.
- There’s a link to a certain type of inherited condition called autosomal dominant, yet no specific genes are identified as being the cause.
Signs and Symptoms of Hemangioma (Strawberry Marks)
Infantile hemangioma, a common type of birthmark, is typically not present at birth but appears within the first few weeks. They start as various types of skin changes, which could be a pale spot, a red or bruise-blue patch. They can occur anywhere on the body, including skin and mucous membranes. Most of the time, there will be only one infantile hemangioma, but in some cases, there can be multiple or large ones. About 60% of these birthmarks are found on the head and neck, 25% on the trunk, and the remaining 15% on the arms and legs.
Infantile hemangiomas can be either on the surface of the skin, deeper beneath the skin, or both. Surface ones appear as raised, bumpy, bright red spots. Deeper ones come from lower layers of the skin and look like blue bumps, plaques, or larger growths. Mixed ones have characteristics of both.
These birthmarks tend to develop and change over three phases:
- Early growth phase, where they grow quickly in the first three to eight months. Especially deep ones may continue to grow until the child’s first birthday.
- Plateau phase, where the birthmark stops growing and stays the same size for a few months, usually between 6-12 months old.
- Involution phase, where the birthmark starts to get smaller and change color from bright red to purple or gray. This can start within the first year and continue for several more, often leading to a soft, compressible birthmark. The skin may return to normal, or there may be leftover changes in the skin, like extra fatty tissue, small visible blood vessels, or loose skin.
Testing for Hemangioma (Strawberry Marks)
If your doctor suspects that your child may have an infantile hemangioma, which is a type of birthmark that appears as a bright red birthmark and shows up at birth or in the first or second week of life, the condition is usually diagnosed simply through a physical examination. However, if there is any uncertainty about the diagnosis, a skin biopsy can be done. A skin biopsy involves taking a small sample of skin for testing. In this case, the sample would be checked for something known as GLUT 1, which is usually found in infantile hemangiomas.
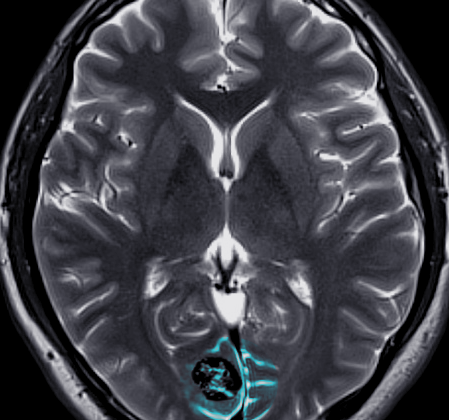
There are also certain imaging tests that can be useful in diagnosing this condition and working out how extensive it is, as well as to rule out any related abnormalities and to ensure it’s indeed an infantile hemangioma rather than another type of tumor. These imaging tests might include an ultrasound (which uses sound waves to create pictures of structures inside the body), a CT scan (which uses x-rays to create detailed images of the body), or an MRI (which uses a large magnet and radio waves to create images of the body).
If there are no outward signs of the birthmark, these imaging tests can be particularly useful in diagnosing hidden or “deep” infantile hemangiomas. These are hemangiomas that have developed deeper in the skin, or even in the muscle or body organs, and therefore do not show the typical signs of infantile hemangiomas on the skin surface.
Treatment Options for Hemangioma (Strawberry Marks)
Most small growths that babies are born with, known as infantile hemangiomas, don’t need to be treated since they typically go away on their own. However, if a baby has a complicated hemangioma, treatment may be necessary.
Most commonly, doctors might use medication called beta blockers, a specific one being propranolol, which helps to shrink the hemangioma. This medicine needs to be taken with caution, as it could potentially slow down the heart rate, lower blood pressure, cause breathing problems, or lead to low blood sugar.
A different treatment could be a medicine called prednisone, but it also needs to be given carefully. Prednisone could lead to side effects like a change in moods, disturbance in sleep, high blood pressure, weakening of bones, and slowing down of growth.
If the hemangioma is small, superficial and uncomplicated, a topical beta blocker, such as timolol, can be applied directly to the skin. Topical or injected corticosteroids, another kind of medication, can also be used for small, focused growths.
In some cases, if medications aren’t working or if the hemangioma might cause complications, doctors may decide to surgically remove it. This procedure involves removing the fatty tissue left behind by the hemangioma, which can improve the outcome of the treatment.
Pulsed dye laser (PDL), a type of laser treatment, can be used for treating visible blood vessels called telangiectasia, but it’s use for larger, deeper hemangiomas remains a topic of debate among doctors.
What else can Hemangioma (Strawberry Marks) be?
When doctors are dealing with hemangiomas, there are different conditions that look very similar and can be confused with each other. Accurate diagnosis can only happen when each possibility is carefully considered. These conditions might include:
- Congenital hemangioma
- Pyogenic granuloma
- Kaposiform hemangioendothelioma
- Tufted hemangioma
- Venous malformation
- Capillary malformation, also known as port wine stain
- Macrocystic lymphatic malformation
- Malignant tumors such as sarcoma, or a kind of skin cancer that is a location of neuroblastoma or lymphoma
What to expect with Hemangioma (Strawberry Marks)
In simple terms, the prospects for recovery from uncomplicated Infantile Hemangioma (IH), which are noncancerous growths usually appearing during infancy, are generally excellent. It’s found that in most cases, these growths completely disappear on their own. By the age of 5 years, 50% of these growths vanish, 70% by 7 years, and up to 90% are gone by 9 years.
Nonetheless, about 8% of Infantile Hemangiomas may leave some cosmetic disfigurement and thus may require some kind of treatment to correct these changes. This means that in some instances, these growths do not entirely fade away and may affect one’s physical appearance, calling for medical or surgical interventions.
Possible Complications When Diagnosed with Hemangioma (Strawberry Marks)
The potential complications of having a hemangioma (a type of birthmark that appears at birth or in the first or second week of life) can topically depend on the person’s age and on the size and location of the hemangioma.
Common Complications:
- Ulceration: It is the most common complication and can happen in up to 10% of cases. The risk of ulceration is higher in the areas like the anogenital area, lower lip, axilla, and neck.
- Ophthalmologic complications: Issues related to vision can occur such as lazy eye (amblyopia), blurred vision (astigmatism), short-sightedness (myopia), behind-eye issues (retrobulbar involvement), and tear duct blockage.
- Airway obstruction: This complication can occur in nasal, voice box (subglottic), and windpipe (laryngeal) passages.
- Feeding difficulties: These are seen when the hemangioma is around the mouth or lip area.
- Visceral hemangiomatosis: If there are more than or equal to 5 skin lesions, liver or gastrointestinal involvement may occur.
- Cosmetic disfigurement: Large facial areas including the tip of the nose (Cyrano nose), ears, and area around the mouth can be affected.
PHACES syndrome could manifest when there is a large facial hemangioma (greater than or equal to 5 cm). The PHACES acronym stands for posterior fossa malformations – brain irregularities, hemangioma of the head and neck region, arterial anomalies, cardiac or heart issues, eye abnormalities, and defects of the chest wall or abdominal wall.
In the same vein, LUMBAR syndrome could manifest when there are lumbosacral hemangiomas (hemangiomas in the lower back or tailbone area) and may be linked to underlying development issues. The LUMBAR syndrome acronym refers to lumbosacral hemangioma, urogenital issues or problems with urinary or genital system, myelopathy or spinal cord issues, bony deformities, anal or arterial issues, and kidney irregularities.