What is Ichthyosis Fetalis?
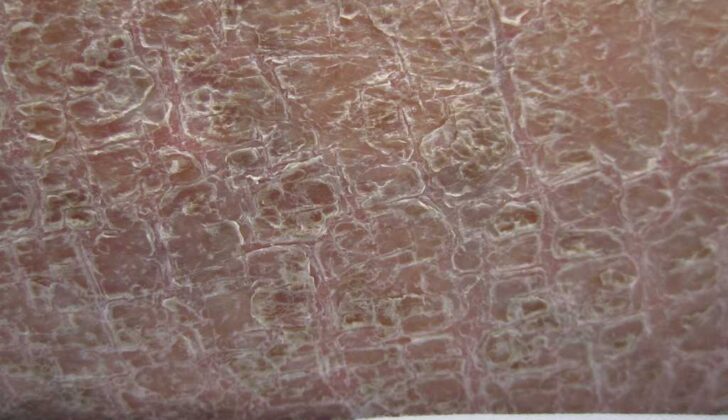
Harlequin ichthyosis, also known as ‘ichthyosis fetalis’, is a very rare skin condition from birth. It’s caused by changes in a gene known as ABCA12, and it’s the most serious type of a group of skin conditions called ichthyosis. This disease causes the skin’s top layers to become very thick and dry, looking like ‘scales’ separated by deep cracks over the entire body. Because of this, babies with this disease have a higher risk of infection as their skin doesn’t provide the protection it should.
What Causes Ichthyosis Fetalis?
ABCA12 acts like a gatekeeper in skin cells that controls the movement of fat molecules. It is part of a system known as ATP-binding cassette transporter that uses energy from ATP, the energy currency of cells, to move fat molecules across the cell membranes. ABCA12 specifically works to transfer fat molecules across cell membranes in the outermost layer of skin via small structures known as lamellar granules. These granules help in forming the fat layer of the skin, particularly in the stratum corneum, which is the outermost layer of the skin.
If there’s a change or ‘mutation’ in the ABCA12 system, it can’t transfer fats to the stratum corneum properly. This then leads to an abnormal formation of the fat barrier, causing an excess buildup of fats within the skin cells. This condition is known as hyperkeratosis. It’s this buildup of fats inside skin cells that results in the typical features seen in Harlequin Ichthyosis (HI), a severe genetic skin disorder.
Risk Factors and Frequency for Ichthyosis Fetalis
Harlequin ichthyosis, a rare skin condition, is reported to occur in about 1 in 300,000 births. The research to date shows no particular susceptibility toward either males or females. Additionally, it appears that this condition doesn’t preferentially affect any specific racial group or sex.
Signs and Symptoms of Ichthyosis Fetalis
Neonates with Harlequin ichthyosis (HI) are often born prematurely and have notably thick, hardened skin. This skin cracks to form yellow, plaque-like “armor” plates that cross the entire body, separated by deep, inflamed crevices. This hard skin restricts movement across the chest, arms, and legs.
Densely layered scales on the chest hinder normal breathing, which can lead to respiratory distress and even respiratory failure. The tension from these tight skin plates can restrict limb mobility and affect blood flow, potentially causing a lack of color in the extremities and tissue decay due to insufficient blood supply.
Thickened skin often covers swollen hands and feet in a glove-like manner. Moreover, the upper and lower eyelids tend to turn outward, a condition known as ectropion, which exposes the inner eyelid and leaves the cornea vulnerable to scrapes and dryness.
The nose might appear flat, and the nostrils may be blocked by the encroaching skin. The ears may also be flattened, with the ear canal obstructed by skin. Severe pulling on the lips leads to eclabium, in which the lips turn outward, giving the appearance of a constantly open mouth.
The dysfunction of the skin barrier results in difficulty maintaining body temperature, malfunctioning sweat glands, excessively high body temperature, and dehydration due to excessive water loss. General hair growth is usually poor, and nail deformities are commonly observed.
Testing for Ichthyosis Fetalis
If a newborn baby is suspected of having Harlequin ichthyosis (HI), doctors often can tell by the distinct physical signs at birth. This disease affects that baby’s skin in a severe way and sadly can have fatal outcomes even before the baby is born. If a family has a history of HI, doctors may perform prenatal genetic testing, which involves analyzing the baby’s DNA before they’re born, to see if the baby will likely have the disease.
Doctors use two main less-invasive procedures to collect the baby’s DNA: amniocentesis or chorionic villus sampling. Both of these procedures have replaced the older, more invasive technique of taking a skin biopsy from the unborn baby. Ultrasound can also be used to look for signs of HI in unborn babies if there’s a known family history of the disease. If your doctor uses a 3-D ultrasound, they’ll look for signs like bulging eyes, a large immobile mouth, a flattened nose, underdeveloped ears, and deformed limbs.
Some other common ultrasound signs include the so-called “snowflake sign,” which refers to seeing dense, floating particles in the amniotic fluid. Other signs can include having too much amniotic fluid, called polyhydramnios, and growth restrictions. Once the baby is born, they can become vulnerable to certain complications. Since their skin is not functioning properly, they may be at risk of systemic infections, which affect the whole body. To monitor for infections, doctors will need to take blood samples on a regular basis, including doing a white blood cell count and blood cultures. If pus is seen in the baby’s skin cracks, a wound culture might be necessary to see if there’s an infection.
Watching the baby closely to make sure they’re not becoming dehydrated is also important. This involves measuring urinary output, weight and checking their electrolytes in the blood, which might be abnormal due to their impaired skin function.
Treatment Options for Ichthyosis Fetalis
Babies born with a condition called Harlequin Ichthyosis (HI) need special care in a neonatal intensive care unit designed for such complex cases. They require a team of various specialists, including dermatologists, neonatologists, plastic surgeons, geneticists, eye doctors, ear, nose, and throat doctors, physical therapists, occupational therapists, dieticians, and social workers. This team works together to provide the utmost care the baby needs.
These little ones are placed in a special isolated room in an incubator that helps maintain their body temperature. They are closely watched for any signs of bacterial infection. Regular check-ins are made to keep track of vital signs, check for any serious signs of illness, and monitor the sodium, potassium, and other minerals in the blood.
One of the problems these newborns may face is skin cracking, which can lead to water loss through the skin and unevenness in blood mineral levels. This makes monitoring the baby’s weight changes, fluid intake, and amount of urine important. If pus starts draining from the cracks in the skin, it’s possible they may have an infection and should be treated with topical antibiotics. Pain relief varies depending on how severe the pain is and can include acetaminophen, non-steroidal anti-inflammatory drugs (NSAIDs), or stronger medications if needed.
HI can also cause complications like troubles in expanding the chest wall which can affect the baby’s lungs and breathing, feeding difficulties and even the risk of respiratory failure. When a baby shows signs of severe breathing trouble, a tube is inserted into their windpipe to ensure they can breathe.
Movement restrictions can also occur in the hands and feet. Removing the plaque and keeping the skin well-moisturized can help avoid serious complications like tissue death due to lack of blood supply. These babies are also at an increased risk of dry eyes that can result in damage to the cornea. Regular eye examinations and the use of artificial tears or other eye lubricants can help prevent this.
Issues with feeding due to tightness around the mouth may require a feeding tube into the stomach. Care for the skin includes regular bathing with only water and applying mineral oil-based products to help soften the hard outer layer of the skin. But because the skin is so delicate, strong moisturizers should be avoided, and soft wraps or gauze should be used instead of tape to hold catheters or tubes in place.
Often, treatment also includes use of a type of medication called retinoids, which helps shed the hard plates on the skin and reduces scaling. Research has shown that the earlier these retinoids are used, the more beneficial they can be, even reducing the risk of tissue death on fingers and toes. Before starting these medications, certain bloodwork and a urine test are needed to assess suitability.
There are several ways to administer retinoids. If the oral method can’t be tolerated, a type of retinoid cream can also be applied on the body parts with more severe symptoms. Once the baby becomes a toddler, the systemic retinoids can be discontinued. The treatment doesn’t stop here; children with HI need regular check-ups with physical and occupational therapists, and sometimes need help from speech and language therapists too if they have cognitive and social challenges.
What else can Ichthyosis Fetalis be?
Ichthyoses are a group of skin conditions that predominantly have abnormal skin cell changes, which are often inherited dominantly from parents. A common way these conditions show up is through a ‘collodion baby’. This term is used to describe a baby who at birth appears to have a shiny, tight film on their skin. This is typical of a subset of ichthyoses known as autosomal recessive congenital ichthyoses (ARCI). ARCI includes types such as:
- Congenital ichthyosiform erythroderma (CIE)
- Lamellar ichthyosis (LI)
- Self-healing collodion baby (the initial layer sheds off with no further skin issues)
The severity of ARCI can range from very serious to less sever, depending on the type. There are also other conditions that may result in a ‘collodion baby’ presentation, including Sjogren-Larsson Syndrome, trichothiodystrophy, and neutral lipid storage disease.
What to expect with Ichthyosis Fetalis
Harlequin Ichthyosis (HI), a severe skin condition, has an extremely high mortality rate. A review of 45 cases of HI showed that out of the 45 patients, 25 survived while 20 did not, resulting in a mortality rate of 44%. The ages of survivors ranged from 10 months to 25 years.
The most common cause of death within the first 3 months was severe, widespread infection, also known as “fulminant sepsis” (75% of cases), and respiratory failure (25% of cases), or a combination of both.
It has been found that early introduction to a type of medication known as oral retinoids can potentially increase survival chances. In fact, 83% of the patients who were treated with retinoids survived, compared to 76% who did not receive retinoids and sadly passed away.
Possible Complications When Diagnosed with Ichthyosis Fetalis
Newborns commonly face serious complications including intense infection (fulminant sepsis), respiratory failure, eyelids and lips turning outwards (ectropion and eclabium), excessive water loss through the skin, imbalance of electrolytes in the body, muscle tightening (contractures), tight skin straps causing poor blood supply to limbs and fingers. Experts have also noted repetitive skin infections in early childhood and changes in the foot that can cause delay in learning to walk due to palm and sole skin thickening (palmoplantar keratoderma). Newborns may also express sensitivity to heat and cold. Skin itching has been reported in almost half of the survivors.
Issues such as slow growth of hair and nail deformities are also pretty common. Eye related problems can include persistent eyelid turning outward, repeated inflammation of the eye surface (conjunctivitis and keratitis). There could be difficulties in gaining weight even with nutrition-rich diets. Delays in hitting appropriate developmental milestones are common and their height and weight are generally below average. The abnormal thickened skin at birth generally transitions to severe scaling redness of the skin within 4 to 6 weeks. Children with this condition need long-term care from a team of health professionals.
Common Complications:
- Fulminant sepsis (Intense infection)
- Respiratory failure
- Ectropion and eclabium (Eyelids and lips turning outwards)
- Excessive water loss through the skin
- Imbalance of body electrolytes
- Muscle tightening (contractures)
- Poor blood supply to limbs or fingers due to skin tighteness
- Repeated skin infections
- Palm and sole skin thickening (Palmoplantar keratoderma)
- Sensitivity to heat and cold
- Skin itching
- Slow growth of hair
- Nail deformities
- Persistent eyelid turning outward
- Repeated inflammation of the eye surface (conjunctivitis and keratitis)
- Difficulty gaining weight
- Delays in hitting appropriate developmental milestones
- Scaling redness of the skin
Preventing Ichthyosis Fetalis
Newborns who have Hyperinsulinism (HI) can be difficult to care for, and it may be hard on their families. It might mean the child’s life could be at risk and long-term care may be needed to ensure they live a life of good quality. It’s important for families to understand all about HI. They should know that the newborn’s early symptoms of the disease may not last long, that any discomfort the child feels can be managed, and that any accompanying skin disorders can also be taken care of. Doctors have the responsibility to inform and counsel parents who might have a family history of HI, and provide them with options for genetic testing.