What is Idiopathic Guttate Hypomelanosis?
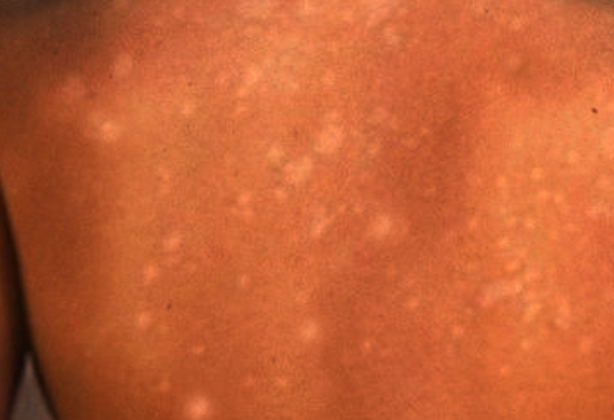
Idiopathic guttate hypomelanosis (IGH) is a harmless skin condition that doesn’t usually cause symptoms. This condition, which often causes small, light-colored spots, is most commonly seen in older people with light skin. The exact cause of IGH isn’t clear. Many people don’t realize they have it or don’t get a diagnosis.
Sometimes, IGH might affect how the skin looks, but it doesn’t cause any health risks. Once these light spots appear, they don’t go away on their own. The goal of the treatment for this condition is to improve the appearance of these spots.
What Causes Idiopathic Guttate Hypomelanosis?
The exact cause of IGH, an abbreviation for Idiopathic Guttate Hypomelanosis, is still not known. There are a few theories out there that we can consider. One is that it could just be a natural part of how skin ages. Another is that it might be due to long-term exposure to the sun over many years. Or, it might happen because of small, repeated injuries to the skin. However, none of these ideas have been confirmed yet.
Risk Factors and Frequency for Idiopathic Guttate Hypomelanosis
IGH, or idiopathic guttate hypomelanosis, is a skin condition that affects people of all races and skin types. It tends to be more noticeable in darker skin tones, but it’s often thought to happen more in fair-skinned individuals. It was previously believed to be more common in females, but recent studies show that it affects both males and females equally. What may have caused this misconception is a greater attention to cosmetic issues by females compared to males.
- The likelihood of getting IGH increases as people grow older.
- Up to 80% of people aged 70 and over have been observed to have IGH.
- A separate study found that up to 87% of patients aged 40 and above had at least one IGH spot.
- The condition can also occur in young adults in their 20s and 30s.
Signs and Symptoms of Idiopathic Guttate Hypomelanosis
Idiopathic guttate hypomelanosis (IGH) is a skin condition characterized by numerous tiny, discrete, round or oval pale patches or spots, typically 2 to 6 mm across. These spots develop gradually over several years and sometimes have larger spots up to 2.5 cm. The affected skin usually feels smooth, although there have been some cases where those spots were scaly or overly thickened (hyperkeratotic). Once the patches appear, they neither alter in size, nor disappear. Hair follicles do not seem to be influenced, and hairs within those spots typically stay their original color. While these patches often occur on areas exposed to the sun, such as the upper and lower parts of the limbs, they tend to lean toward the far ends of those limbs over closer parts. However, the condition can still affect areas untouched by the sun, such as the torso, and, on rare occasions, the face.
Testing for Idiopathic Guttate Hypomelanosis
If a doctor suspects you might have idiopathic guttate hypomelanosis (IGH), a harmless condition where small white spots appear on the skin, there’s typically no need for traditional medical tests. This means you won’t have to do any blood tests or x-rays to investigate these spots.
It’s enough for your doctor to use a tool known as a dermoscope to look at these skin spots. A dermoscope is a device that helps doctors see the skin’s surface in greater detail. Using a dermoscope, your doctor may spot different patterns that indicate IGH. These patterns include:
- Amoeboid: This looks like extensions that resemble the arms of an amoeba, a single-celled organism.
- Feathery: This pattern looks unevenly colored with feathery edges and a whitish center.
- Petaloid: This pattern has borders that look like flower petals.
- Nebuloid: This pattern has faded, blurry edges.
The nebulous pattern is usually seen in early stages of the condition, while the amoeboid, feathery, and petaloid patterns are typically found in more mature spots.
Treatment Options for Idiopathic Guttate Hypomelanosis
People should not worry as Idiopathic guttate hypomelanosis (IGH), a condition evidenced by small, benign white spots on the skin, is harmless and doesn’t typically require treatment. There’s no widely agreed upon cure or remedy for this condition.
Generally, experts agree that sun exposure could potentially make this condition worse. Thus, all patients should be encouraged to protect their skin from the sun by using sunscreens and physical barriers like clothing or hats.
While IGH is benign and usually doesn’t require treatment, some people might want to treat it for cosmetic reasons. Several treatment options can help reduce its appearance to varying degrees. These methods include cryotherapy (using cold temperatures to remove skin lesions), superficial abrasion (lightly scraping off the skin surface), and using a variety of topical treatments like steroids, retinoids, and calcineurin inhibitors.
Other techniques, like dermabrasion (a type of surgery to improve the skin’s appearance), laser treatments and light therapies, may also improve the look of the skin. It’s important to know that some treatments, like cryotherapy, can cause skin lightening, or hypopigmentation. And other treatments, like laser therapies, can cause short-term skin redness and darkening. Some recent studies suggest that using a combination of light therapies and the topical use of calcineurin inhibitors might offer better results. Other studies suggest that microneedling in combination with the application of medicine might increase the number of pigment cells in the skin, potentially providing a promising treatment option.
What else can Idiopathic Guttate Hypomelanosis be?
When trying to diagnose guttate leukoderma, a type of skin discoloration, doctors have to consider a wide range of other skin conditions that might look similar. These include:
- Idiopathic guttate hypomelanosis (IGH)
- Vitiligo
- Pityriasis versicolor
- Pityriasis alba
- Café au lait spots
- Lichen sclerosis
- Guttate morphea
- Simple post-inflammatory hypopigmentation
- Achromic verruca plana
- Pityriasis lichenoides chronica
- Disseminated hypopigmented keratoses that follow psoralen and ultraviolet A (PUVA) therapy
- Clear cell papulosis
- Atrophie blanche
Each of these conditions has a distinct pattern and unique characteristics. For instance, achromic verruca plana lesions are more likely to react to injury or irritation (a phenomenon known as koebnerization) and would show particular cells (koilocytes) when examined under a microscope. Disseminated hypopigmented keratoses usually occur after a patient has gone through PUVA therapy and appear as well outlined, small, pale, flat bumps on the trunk and limbs. Clear cell papulosis, a rare condition, usually affects young children and is characterized by multiple pale, slightly raised, small flat spots and patches, particularly on the face and trunk. Atrophie blanche, on the other hand, tends to show up on the lower legs, appearing as very white, sunken scars that are surrounded by visibly enlarged small blood vessels (telangiectasia).
What to expect with Idiopathic Guttate Hypomelanosis
IGH, or idiopathic guttate hypomelanosis, is a harmless condition and people usually have a great outcome. Though, once it’s there, it won’t go away on its own – thus, it’s mostly considered a concern for appearances. IGH could potentially signify that a person has had accumulated exposure to the sun. However, there has been no confirmed direct link established to date.