What is Livedoid Vasculopathy?
Livedoid vasculopathy is a rare blood vessel condition that usually affects both lower legs. It’s thought to be caused by blood clots forming in the small blood vessels, due to an increased risk of clotting, a reduced ability to breakdown clots, and damage to the inner lining of the vessels.
This condition is three times more common in women than in men, particularly in those aged between 15 and 50 years. To manage this condition, doctors identify the leg lesions (damaged or abnormal areas of skin) and differentiate it from other leg lesions. A skin biopsy, where a small sample of skin is taken for testing, is also often done to confirm the diagnosis.
There isn’t a single best treatment, but general steps like quitting smoking, looking after wounds, and medical treatments such as blood thinners and medicines to stop blood clots from forming have been found to work well.
Several newer and experimental treatments have also shown promise in tough cases.
In the past, livedoid vasculopathy has been given different names such as livedo vasculitis, livedoid vasculitis, and livedo reticularis with summer ulceration.
What Causes Livedoid Vasculopathy?
Vasculopathy is a condition in which a blood clot forms inside an artery, which blocks the flow of blood. It’s different from vasculitis, which is when the walls of the blood vessels are inflamed and cause the surrounding tissues to break down and die.
Livedoid vasculopathy, a specific type of this condition, is mainly linked to situations that raise the chance of blood clotting and clot formation, which include:
* Health situations linked to static blood flow: Chronic high blood pressure in the limbs, varicose veins. Although, with vasculopathy, the skin is usually not surrounded by a net-like pattern of blood vessels (livedo reticularis).
* Autoimmune diseases impacting the tissues connecting the body parts: Conditions like systemic lupus erythematosus (SLE), antiphospholipid antibody syndrome, rheumatoid arthritis, scleroderma, and mixed connective tissue disease.
Then comes Thrombophilias, conditions that increase the likelihood of blood clotting. These can either be inherited (passed down in families) such as factor V Leiden variant, a mutation in the prothrombin gene G20210A, deficiencies in proteins such as protein C, protein S, and antithrombin, or they can be acquired, like high levels of homocysteine in the blood, cryoglobulinemia, cryofibrinogenemia, and acquired antiphospholipid antibody syndrome.
Also, certain types of cancer, such as disorders related to excessive production of white blood cells, the presence of abnormal proteins in the blood, among others. Additionally, some causes are idiopathic, which means they occur for unknown reasons.
Risk Factors and Frequency for Livedoid Vasculopathy
Livedoid vasculopathy is a rare condition that occurs in about 1 out of 100,000 people per year. This condition is more common in women than men, with women being affected three times more often. Typically, those affected are between the ages of 15 and 50. Interestingly, the number of livedoid vasculopathy cases tends to rise during the summertime. It has also been frequently observed in pregnant women.
- Livedoid vasculopathy is a rare condition.
- About one in 100,000 people are diagnosed with it each year.
- Women are three times more likely to have this condition than men.
- Most patients are between the ages of 15 and 50.
- There’s a noticeable increase in livedoid vasculopathy cases during the summer.
- The condition is frequently seen in pregnant women.
Signs and Symptoms of Livedoid Vasculopathy
Livedoid vasculopathy is a skin condition that usually shows up as painful, stubborn ulcers and white scars near the ankles. These are often associated with a painful burning sensation. This burning pain is typically the first symptom people notice. Unlike many other conditions that affect the whole system of the body, livedoid vasculopathy mostly affects the skin.
However, similar skin lesions can be seen in other diseases that relate to the immune system, blood clotting disorders, and inherited conditions that cause blood clots. Therefore, it’s important to ask about these related diseases when talking with your doctor.
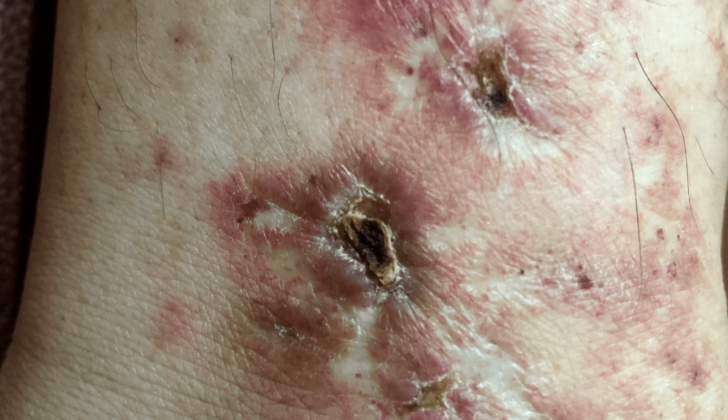
Specific signs of livedoid vasculopathy include ulcers that look like they’ve been punched out in the area around the ankle joint. These are surrounded by lace-like, net-like, red to purple streaks known as livedo reticularis. When these ulcers heal, they form white scars surrounded by small, dilated blood vessels. These scars are the result of damage to the tiny blood vessels supplying the skin. They are not specific to livedoid vasculopathy but can be seen in other conditions as well.
- White scars
- Red to purples streaks known as livedo reticularis
- White scars
- Small, dilated blood vessels
When the condition is active, it’s characterized by the presence of ulcers. Before ulceration, the net-like pattern of livedo reticularis and livedo racemosa are already present. The characteristic presentation of the disease is painful purpuric ulcers with a net-like pattern on the lower extremities, which in summary is referred to as PPURPLE. Another important feature is retiform or star-shaped purpura which is considered to be a key sign.
The majority of the time, these lesions are observed in the area around the ankle joint, but they can also appear on the lower leg and foot. In most instances, the disease affects both body sides.
Testing for Livedoid Vasculopathy
If you have skin sores that might be a condition called livedoid vasculopathy, doctors will need to ensure that this is indeed the correct diagnosis, eliminate other similar conditions that it might be, and check for any related health issues.
To confirm the diagnosis, doctors usually perform a skin biopsy. In this procedure, they would use a tool to remove a small piece of skin, about 3-4mm, from the edge of the sore or from the surrounding skin that shows a lace-like purplish pattern, known as livedo.
Your doctor might also check the blood flow in your legs by measuring your ankle-brachial pressure index and performing a lower limb venous doppler test. These tests can help them rule out chronic venous insufficiency, a condition where the veins in your legs struggle to send blood back to the heart.
Additionally, laboratory tests may be done to check for several possible related health conditions. These may include conditions that result in blood clotting more easily than normal, such as factor 5 Leiden mutation and hyperhomocysteinemia; disorders that affect fibrin – a protein that helps form blood clots – such as protein C and protein S deficiency; diseases that cause harm to your body’s connective tissue, such as lupus and scleroderma; and a condition where proteins build up in your body, known as paraproteinemia.
Treatment Options for Livedoid Vasculopathy
The treatment for livedoid vasculopathy mainly aims to prevent the formation of new skin ulcers, help existing ulcers heal faster, and manage pain. Here’s a simplified explanation of the general ways to manage the condition:
– Pain Management: Over-the-counter drugs known as nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain. Certain antidepressants and antiepileptic medications can also be used, as they can help alleviate nerve-related pain.
– Intravenous Immunoglobulin (IVIG): IVIG is a blood product that can quickly relieve pain. This is because it can stop certain substances in your blood from limiting the blood flow to your skin.
– Wound Care: Taking good care of any skin wounds you have can help them heal faster.
– Quitting Smoking: If you smoke, quitting can help improve your skin’s health and blood flow.
– Compression Therapy: This therapy involves wearing a snug garment to help improve blood flow.
While there are no set treatment guidelines for livedoid vasculopathy, a mixture of blood-thinning medications, medications to stop blood clots, treatments to break down blood clots, and medicines often used by bodybuilders have been found to help. Here are some examples of each type:
– Antiplatelet Agents: These medications, including Aspirin, work to stop blood clots from forming.
– Anticoagulants: Medications like low molecular weight heparin can prevent your blood from clotting.
– Fibrinolytic Therapies: These agents can dissolve existing blood clots.
– Immunomodulatory and Immunosuppressive Agents: These medicines can regulate or suppress your immune system to prevent it from damaging your blood vessels.
– Vasodilators: Medications like nifedipine, which can widen your blood vessels, can also be beneficial.
Other treatments, like receiving high levels of oxygen in a pressurized chamber (hyperbaric oxygen therapy), may also be used.
What else can Livedoid Vasculopathy be?
When it comes to diagnosing livedoid vasculopathy, doctors look at several possible conditions. The following are some of the main ones they consider:
- Livedo Reticularis With Ulceration: This active stage often gets confused with cutaneous polyarteritis nodosa (PAN). Cutaneous PAN is recognized by special skin patterns, under-skin lumps, and another kind of skin pattern known as starburst livedo. It’s a type of issue affecting the medium-sized blood vessels in the skin. The presence of under-skin lumps, occasional digital gangrene (dead tissue due to lack of blood flow), and certain findings when looking at a tissue sample under a microscope helps doctors diagnose this condition.
- Atrophie Blanche: In this condition, porcelain-like white scars get noticed. These kinds of scars are also seen in sickle cell disease, hydroxyurea ulcers, and malignant atrophic papulosis.
- Other: Other conditions that seem like livedoid vasculopathy include: ANCA-associated vasculitis (a group of diseases where the body’s own immune cells attack the small blood vessels), cutaneous small-vessel vasculitis (inflammation of the skin’s small blood vessels), cryoglobulinemia (an abnormal protein that can clump together in the cold), and Sneddon syndrome (a condition with a particular skin pattern, livedo racemosa, and strokes).
As with any diagnosis, the physician must consider these possibilities and conduct detailed examinations to get an accurate diagnosis.
What to expect with Livedoid Vasculopathy
The future course or outlook of livedoid vasculopathy, a skin disorder caused by changes in the small blood vessels, can differ greatly from person to person. It is affected by a number of things including the root cause of the condition, how the patient responds to treatment, and any other health issues they may have.
Important Things To Remember
The Long-Lasting Nature of the Condition
Livedoid vasculopathy typically follows a pattern of ups and downs over a long period of time. This means that people suffering from it may experience episodes of painful skin sores or ulcers that come and go.
Finding the Root Cause
One of the most important factors in determining how the condition progresses is identifying and dealing with any underlying issues. Livedoid vasculopathy can be a primary condition, meaning it happens on its own, or secondary, meaning it occurs as a result of other conditions such as blood clotting disorders, inflammation of blood vessels, or problems with connective tissue. If the root cause can be effectively managed, the outlook for the patient tends to be better.
Possible Complications
Complications like ulcers that don’t heal, skin getting thinner, or secondary infections, can influence the outlook of the condition. It’s important to catch and manage these complications early to prevent long-term issues.
How Well the Patient Responds to Treatment
How a patient responds to treatment can greatly impact the outlook of the condition. Treatments for livedoid vasculopathy can include blood thinners, medications to suppress the immune system, and wound care. Finding the most effective treatment often involves some amount of trials to find what works best
The Need for a Team of Doctors
Managing livedoid vasculopathy often requires collaboration between different specialists, including skin, rheumatology, and blood disorder doctors. This teamed approach can lead to a more thorough evaluation and treatment plan, potentially improving the future outlook of the condition for the patient.
Possible Complications When Diagnosed with Livedoid Vasculopathy
Livedoid Vasculopathy, a condition affecting blood vessels, commonly displays in the form of ulcer-like lesions on both lower legs. Patients can also experience additional local issues such as secondary skin infections which cause classic signs of inflammation. Other symptoms of Livedoid Vasculopathy may include:
- Pain, which is usually due to lack of oxygen reaching tissues in the leg and the body’s inflammatory response.
- Darker patches of skin, caused by red blood cells leaking from vessels, and iron deposits in the skin.
- Mononeuritis multiplex, a type of nerve disease, brought about by blood clots in the nerves’ blood vessels.
- Skin scarring that has a sunken appearance.
Preventing Livedoid Vasculopathy
Learning about your disease is a crucial part of effectively managing it. One important aspect of this is understanding the need to quit smoking. Following other general recommendations, such as wearing support stockings and taking care of any wounds, is also extremely important. Lastly, it’s essential to know when you need to seek urgent medical attention. If you notice that your symptoms are getting worse, you should immediately contact your doctor. This anticipation helps to avoid further complications and assists you in managing your health better.