What is Nevus Anemicus?
Nevus anemicus is a rare skin condition that a person can be born with. It appears as lighter skin spots or patches. The lighter color is due to a localized increase in a type of hormone called catecholamines. This leads to the narrowing of blood vessels or vasoconstriction, which thus makes the skin look pale.
This condition was first noted by a scientist named Vorner in 1906. One unique feature of nevus anemicus is that it doesn’t turn red when injured or exposed to hot or cold temperatures, unlike regular skin. This skin condition is often confused with other conditions such as vitiligo, a disease that causes the loss of skin color in patches, or nevus depigmentosus, another type of skin disorder. Hence, diagnosing nevus anemicus can be a special challenge in the field of skin health, known as dermatology.
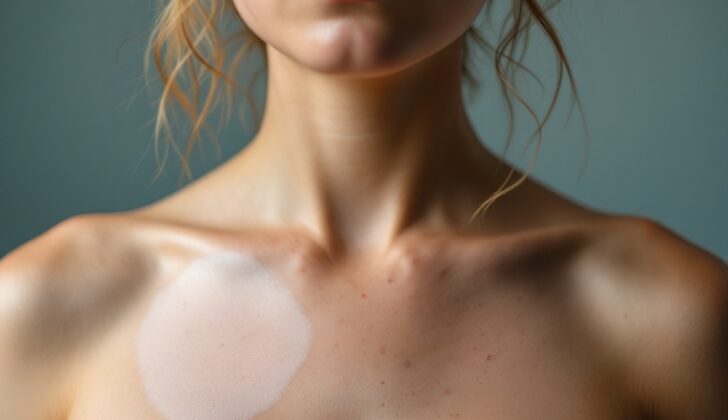
Generally, individuals with this condition have a pale spot or patch that doesn’t cause discomfort. This spot or patch has been there since birth, grows with the person, and stays symptom-free throughout their life. These spots are usually found during skin check-ups. They might have smaller, lighter-colored spots around them. Nevus anemicus can involve a single area or multiple areas and often appears on the upper chest, though it can occur anywhere on the body.
Knowing and understanding about nevus anemicus is vital for correct identification. Knowledge about this condition helps avoid inappropriate treatments and leads to better results in managing skin health.
What Causes Nevus Anemicus?
Nevus anemicus is a skin condition that usually appears as a single spot and doesn’t tend to cause any other symptoms. It’s not certain if this condition is genetic if it appears on its own. However, it seems to be linked with certain genetic syndromes like neurofibromatosis type 1 (NF1), tuberous sclerosis, and phakomatosis pigmentovascularis types II to IV.
Each type of phakomatosis pigmentovascularis has a characteristic birthmark known as nevus flammeus, or a port-wine stain. Nevus anemicus has been seen near these port-wine stains, which may suggest a connection between the two. Phakomatosis pigmentovascularis type II is associated with “Mongolian spots” (birthmarks caused by pigment cells in the skin), type III is linked with nevus spilus (a speckled birthmark), and type IV is associated with both nevus spilus and Mongolian spots.
People with NF1 tend to develop nevus anemicus at a younger age than those without the condition. However, having nevus anemicus does not increase the risk of other NF1 complications, like optic gliomas (a type of brain tumor). On the other hand, Legius syndrome, which is similar to NF1 and characterized by light brown spots on the skin and freckling in areas where the skin folds, does not include nevus anemicus.
Nevus anemicus has also been rarely connected with other skin conditions like telangiectatic nevus (a condition where the blood vessels widen abnormally) and Becker nevus. When nevus anemicus and reticular telangiectatic vascular malformations (a network-like pattern of widened blood vessels) appear together, they form a condition called nevus vascularis mixtus or mixed vascular nevus. There have also been cases where nevus anemicus is associated with Dyke-Davidoff-Masson–type brain abnormalities, which involve underdevelopment of the middle and large blood vessels in the brain.
Risk Factors and Frequency for Nevus Anemicus
Nevus anemicus is a skin condition that isn’t always easy to spot, particularly in people with lighter skin types. Because of this, it might be more common than we realize. Research estimates that it affects about 1% to 2% of people. It can be present from birth or show up in early childhood. People of all ethnicities can get it. While early research suggested it was more common in females, recent studies have found that it affects males and females equally, when considering its occurrence with NF1, another genetic disorder.
- Nevus anemicus is often harder to detect in people with lighter skin.
- About 1% to 2% of people have nevus anemicus, based on research.
- It can be present from birth or appear in early childhood.
- It affects people of all ethnicities.
- Early studies thought it was more common in females, but recent research shows it affects males and females equally when considering its association with NF1.
Signs and Symptoms of Nevus Anemicus
Nevus anemicus is a skin condition that appears as light-colored patches with clear edges. These harmless patches usually show up on the upper body but can sometimes be on the face or arms and legs. The condition doesn’t affect hair distribution, sweat production, or skin feeling. A typical nevus anemicus patch is between 5 to 10 cm, but in some instances, it can cover large areas of the body. This is known as “giant nevus anemicus.” The patches can have spots of regular skin within them or tiny light-colored spots around them. The patches can also take different shapes such as lines or clusters that look like grapes. A less common type of the condition causes many nevus anemicus patches that present a mesh-like pattern.
To diagnose nevus anemicus, doctors rely on the medical history and a physical check-up because there are no specific laboratory findings. The history of when the patches appeared is essential because nevus anemicus often shows up at birth, unlike other skin conditions like vitiligo, which typically develops later in life.
Skin with nevus anemicus doesn’t turn red in response to heat, cold, or injury. Doctors can test this by rubbing the patch and the normal skin around it or by applying ice or heat. This will make the skin around the patch turn red while the patch itself will stay pale. Another test is diascopy, which involves pressing a glass slide on the edge of the patch. This will make the patch blend with the normal skin around it. In some instances, other vascular anomalies, such as port-wine stains, may be seen close to the patches.
Testing for Nevus Anemicus
A Wood lamp, which shines UV light with a particular wavelength, is often used to help diagnose a skin condition called nevus anemicus. This type of lamp won’t make the lighter patches of nevus anemicus appear more pronounced, but it will make the lighter areas seen in other conditions like nevus depigmentosus and vitiligo stand out.
Also, a skin biopsy can be done. In this test, the doctor takes a small sample of your skin to look at it more closely. If the skin sample looks normal, it could help rule out other skin conditions that cause lighter patches like vitiligo.
If we look at the same skin sample under an electron microscope, we would expect to see normal results for someone with nevus anemicus. However, in nevus depigmentosus, while the number of cells producing melanin (the pigment that gives skin its color) is normal, there is less melanin being produced.
If the doctor suspects a fungal skin infection called tinea versicolor, they would perform a test using potassium hydroxide on the affected skin. This test would show the characteristic “spaghetti and meatballs” appearance of the fungus Malassezia furfur, which shows up as thread-like structures and round spores.
Nevus anemicus is known to develop due to a lack of blood vessels at the center of the lesion. This is often seen with an increase in blood flow in the surrounding skin, and it merges with the surrounding skin when viewed through a dermoscope (a tool that allows doctors to look at the skin closely). Such distinctive characteristics as seen from dermoscopy can help doctors diagnose the condition earlier.
Treatment Options for Nevus Anemicus
Nevus anemicus is generally not dangerous and doesn’t cause any symptoms, so most people don’t need treatment for it. The most critical part of dealing with this condition is making sure it’s not mistaken for other skin conditions that cause light spots, to prevent patients from undergoing treatments they don’t need. If you have nevus anemicus, it’s important to know that the condition is harmless. Special makeup that matches your skin color can be used to cover up the spots if they’re on your face and you’re uncomfortable with how they look.
In some rare instances, people may want to treat nevus anemicus for cosmetic reasons. However, treatments are somewhat limited because the condition is related to the blood vessels underneath the skin. Laser therapy, which is often used to treat other skin color issues, doesn’t work for nevus anemicus. Education about the condition and support for any emotional issues caused by the appearance of the skin are an important part of managing nevus anemicus effectively.
What else can Nevus Anemicus be?
When diagnosing nevus anemicus, a condition that creates pale patches on the skin, healthcare professionals need to consider other conditions that could be mistaken for it. These conditions might include:
- Vitiligo
- Pityriasis alba
- Nevus depigmentosus
- Tinea versicolor
- Tuberous sclerosis
- Halo nevus
- Piebaldism
- Hansen disease (also known as leprosy)
- Physical leukodermas (caused by mechanical, chemical, or thermal factors)
- Achromic nevus
- Postinflammatory hypopigmentation
- Progressive macular hypomelanosis
- Scarring
A technique called “diascopy” can help distinguish nevus anemicus from other conditions. This involves applying pressure to the skin with a glass slide. Unlike other disorders, nevus anemicus doesn’t become more apparent under a Wood lamp examination, and the spots don’t change with friction, heat, or cold.
For example, if you scratch a line across the lesion and normal skin, only the normal skin will become red.
Other conditions have different characteristics. For instance, Vitiligo creates distinct white marks with irregular borders that may have rims of increased skin pigment or redness, and even white hairs within the lesion. Nevus depigmentosus appears as light patches early in life but doesn’t lack redness when exposed to trauma, heat, or cold like nevus anemicus does. Pityriasis alba is usually found in patients with atopic dermatitis, while tinea versicolor shows up as light patches after instances of excessive sweating. These two conditions, as opposed to nevus anemicus, don’t generally start at birth.
What to expect with Nevus Anemicus
The outlook for nevus anemicus, a kind of birthmark, is very good. It’s harmless and usually doesn’t cause any symptoms. This birthmark stays the same throughout a person’s life and doesn’t turn into cancer or any other serious skin problems. While these lighter patches of skin may last a lifetime, they don’t cause any discomfort or interfere with normal body functions.
Possible Complications When Diagnosed with Nevus Anemicus
People with a skin condition called nevus anemicus generally don’t face any additional health issues or complications related to this discoloration. But, if a child with many coffee-colored skin spots (café-au-lait macules) also has nevus anemicus, it could suggest they have Neurofibromatosis Type 1 (NF1). According to two different studies, nevus anemicus is found in approximately 50% of those with NF1.
Some Important Points:
- Nevus anemicus on its own doesn’t lead to more health problems
- When a child with many coffee-colored skin spots also has nevus anemicus, it might indicate NF1
- About half of the people with NF1 also have nevus anemicus according to two studies.
Preventing Nevus Anemicus
If you have nevus anemicus, it’s crucial for you to know that this skin condition is harmless. Despite common misconceptions, nevus anemicus is not harmful and does not come with health risks. It is a benign condition which means it’s not cancerous, and it remains stable, not getting worse over time.
Doctors and health workers have a vital role in making sure patients understand this. They can explain that there’s no need for treatment unless you’re concerned about how it looks. Methods like laser therapy don’t usually work and can unnecessarily complicate things. By avoiding needless treatments, you can prevent unwanted side effects, save money, and reduce stress or anxiety about the condition.
Knowing about the gentle signs of nevus anemicus can also help healthcare professionals identify and handle it correctly. Recognizing and managing this condition properly is crucial to avoid misdiagnosis and undiagnosis. As a result, you can be reassured that you’re getting the right care and advice.