What is Pressure Injury?
Pressure injuries are damages to the skin and underlying soft tissue, usually found over bony parts of your body or caused by medical devices. These injuries happen from too much pressure on one area over time, made worse by rubbing or shearing forces. These types of injuries are a major problem in hospitals and long-term care facilities. They can lead to a lower quality of life, cause high costs for patients and the healthcare system, and increase the risk of illness and death. In fact, pressure injuries are often used to measure the quality of a healthcare facility. If they don’t take the right steps to prevent or treat these injuries, they might face legal action. Knowing what can cause pressure injuries can help identify patients at risk and take steps to prevent them.
Different treatments for pressure injuries have been examined to different extents, so it’s not completely clear what the best treatment options are.
The top layer of skin is usually less likely to be impacted by a pressure injury. However, a physical exam might not show the full extent of the injury. Patients who can’t move around much, like those who are bed-ridden or confined to a chair, are usually more at risk of pressure injuries. But, pressure injuries can also be caused by things like ill-fitting casts, other medical equipment, devices, and implants. Medical devices can also cause pressure injuries inside the body.
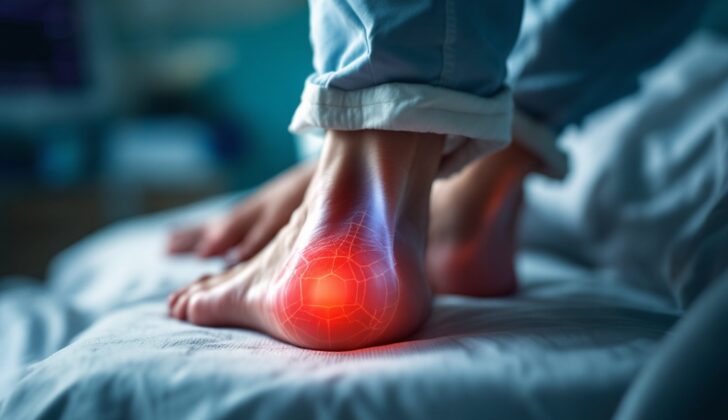
Pressure injuries are seen as localized skin with or without damage to the underlying tissue. They normally occur over a bony area. The starting factors are often pressure or pressure along with shear stress. The most common locations for these injuries include the tailbone, heel, and hips. Dampness-induced injuries on the skin surface, skin tears, burns from medical tape, skin inflammation in the genital area, or skin damage should be told apart from pressure injury-induced lesions.
According to the National Pressure Injury Advisory Panel, the term “pressure injury” is preferred over “pressure ulcer.” The reason for this is because small amounts of skin damage from pressure might not necessarily lead to an ulcer and can be classified as a stage 1 pressure injury. Also, a deep tissue pressure injury might happen without a noticeable ulcer on the skin.
What Causes Pressure Injury?
Pressure sores, also known as pressure injuries, can occur when the weight of someone’s body or a medical device is putting too much pressure on their skin for a long time. This is especially likely in people who have lost their sense of feeling, as they may not realize the pressure is causing a problem, leading to skin damage. Several things can add to the risk of getting these sores, including high blood pressure in the small blood vessels, scraping or pulling on the skin, excess sweat or dampness, and poor nutrition.
Risk Factors and Frequency for Pressure Injury
Pressure injuries or sores affect about a million to three million people in the US every year. These injuries are wounds that develop on your skin and underlying tissues due to prolonged pressure. The likelihood of getting these injuries varies based on the environment. For instance, 5% to 15% of patients in hospitals experience pressure injuries, but this percentage can be much higher in long-term care facilities or intensive care units.
In general, there are several factors that increase the risk of developing these injuries:
- Inability to move about
- Poor blood flow
- Poor nutrition
- Loss of sensation
- Having brain or heart disease
- Having a recent leg fracture
- Having diabetes
- Struggling with involuntary urination or bowel movements
Additionally, elderly patients are at a higher risk because as skin ages, it gets thinner, making it less resistant to pressure and shearing forces.
Signs and Symptoms of Pressure Injury
When a patient has skin breakdowns, it’s crucial to measure their length, width, and depth, and carefully check for certain features. This includes the presence of sinus tracks (small, abnormal channels in the body), dead tissue, fluid leakage, and whether new tissue is forming.
The severity of skin breakdowns, or pressure injuries, can be categorized using the National Pressure Injury Advisory Panel’s stages:
- Stage 1: The skin is still whole, but there’s a red spot that doesn’t blanch (turn white) under pressure, and lasts for over an hour after pressure is relieved.
- Stage 2: Formation of blisters, boils, or some skin breakdown. At this stage, there might be partial-thickness loss of skin layers, and there may or may not be signs of infection.
- Stage 3: A deep wound with full-thickness skin loss. Subcutaneous fat may be visible, there may be damage to the muscle layers, and the wound may feature undermining and tunneling.
- Stage 4: A very deep wound with full-thickness skin loss that also involves bone, tendon, or joint.
- Unstageable: The base of the wound is covered with sloughed-off tissue or a scab, so the extent of the injury isn’t clear.
- Deep tissue pressure injury: The skin shows localized discoloration, which is usually purple or maroon, due to a pressure or shear injury and a blood-filled blister.
Knowing a patient’s medical history can also help identify risk factors for developing wounds and difficulties in healing. Useful information includes prior history of wounds, their cause, location, duration, and treatment. It’s especially important to ask about conditions that impair healing such as diabetes, kidney disease, peripheral artery disease, immune deficiency, or malnutrition.
Patients can also provide important information about their current wound, like its location, duration, causes, changes in size, and pain details, and any previous treatment.
It’s important to assess certain parts of the body for pressure injuries, which commonly occur on the sacrum, greater trochanter (part of the hip bone), ischial tuberosity (sitting bone), lateral malleolus (outer ankle), and heel.
When assessing a pressure injury, the clinician should check the:
- Location
- Length, width, and depth
- Presence of undermining or tunneling
- Presence of dead tissue
- Signs of infection such as redness, tenderness, heat, pain, and any fluid drainage (including its amount, type, smell, and color).
It’s essential to document all these findings to fully understand the patient’s condition and provide the appropriate treatment.
Testing for Pressure Injury
All pressure injuries should be evaluated using a specific system. Although there isn’t a universal system, many health professionals use a scheme recommended by the National Pressure Injury Advisory Panel. This system identifies different stages of a pressure injury:
* Stage 1: Skin redness that doesn’t disappear within an hour after pressure is relieved
* Stage 2: Partial skin loss that reveals the under-layer of skin
* Stage 3: Full skin loss; under-layers of skin and muscle may be seen
* Stage 4: Full skin loss; parts such as tendons, bones, and joints may be visible
* Unstageable: Full skin loss where the wound is hidden by dead tissue
* Deep tissue: Persistent dark red or purple skin that doesn’t change color when pressed
Doctors might also perform lab tests to identify underlying issues that could prevent the healing of these injuries. These issues may include infection, anemia (lack of healthy red blood cells), poor nutrition, and diabetes.
The tests could include:
* Comprehensive metabolic panel (a series of blood tests that measures your sugar level, kidney function, and electrolyte balance)
* Complete blood count with differential (a test that helps diagnose conditions which can affect the blood cells, such as infection, anemia, and other diseases)
* Albumin and pre-albumin tests (to assess nutritional status)
* Hemoglobin A1C (a test for diabetes)
Infections in pressure injuries are typically deep within the wound. Swabbing the surface of the skin for a culture (a lab test) may not be very helpful because it usually just shows what bacteria are on the skin’s surface rather than what bacteria might be causing an infection deeper in the wound. Bone or deeper tissue cultures also should not be the only way a doctor determines if there is an infection. Those results need to be considered alongside the details of the patient’s condition and other lab test results.
Treatment Options for Pressure Injury
Taking care of pressure injuries involves relieving pressure on the affected area and making sure the patient is comfortable. This can be achieved by changing the patient’s position regularly, and using specific support surfaces such as special foam mattresses, medical-grade sheepskin, or devices that alternate pressure. Although all these methods can help reduce the risk of developing pressure injuries, it’s not clear which one is the most effective for treating existing injuries.
Another important aspect of caring for pressure injuries involves managing pain, which can be quite severe especially when changing dressings. Pain can be managed with a plan that may include different types of pain medication. In addition, eating a diet rich in calories and protein can be beneficial, especially for more serious injuries. High-protein foods or supplements may help reduce wound size in patients with pressure injuries, although the evidence to support this is limited.
Wound care is crucial in managing pressure injuries. This involves keeping the wound clean, removing dead or damaged tissue (a process known as debridement), applying dressings, monitoring the wound’s progress, and possibly using other treatments. The treatment used can depend on how severe the pressure injury is. For instance, mild pressure injuries may be protected with a certain type of dressing, and more severe ones may need a different approach, including debridement or the use of absorbent dressings.
While different dressings and topical treatments are available to manage pressure injuries, no one treatment has been proven superior. The choice of dressings may be based on the specifics of the wound, cost, or the patient’s preference. These can include foam, hydrogel, film, or alginate dressings. Additionally, there are extra therapies such as negative-pressure wound therapy, electromagnetic therapy, light therapy, ultrasound, and reconstructive surgery, but their effectiveness is not entirely clear.
Other therapies, including electrical stimulation, ultrasound, hyperbaric and topical oxygen, may also be used in managing pressure injuries, but their efficacy varies. Evidence is lacking on the benefits of hyperbaric oxygen therapy and ultrasound therapy for treating wounds. However, high-frequency ultrasound, which penetrates deeper into tissues, may help reduce wound size. Some studies suggest that applying electricity around the wound might speed up healing, but the evidence is not clear.
What else can Pressure Injury be?
When treating pressure injuries, it’s crucial for doctors to also consider other conditions that may show similar symptoms. These could include:
- Ulcers caused by poor blood flow due to venous insufficiency
- Ulcers related to diabetic neuropathy
- Ulcers caused by inadequate blood supply to the skin, called arterial or ischemic ulcers
- Ulcers that are associated with cancer
- Ulcers caused by high blood pressure
What to expect with Pressure Injury
Having a pressure injury can suggest that a patient’s overall health outlook may not be good. Studies suggest that both elderly and patients in intensive care with pressure injuries have a higher risk of death. This may reflect the seriousness of their underlying condition rather than the injury being a direct cause of death. There may also be other unseen health conditions contributing to the higher illness and death rates seen in patients with pressure injuries.
Possible Complications When Diagnosed with Pressure Injury
Infections are a serious issue that can occur with pressure injuries. These infections can take many forms. They can start off as an infection at the spot of the injury, or even spread to soft tissue, the bone (which is called osteomyelitis), and even your bloodstream. When osteomyelitis occurs, it usually shows up as a wound that won’t heal, but often it does not lead to whole body symptoms such as sepsis or a high white blood cell count. Bacteremia, infection of your bloodstream, is usually easier to spot since it typically goes hand-in-hand with signs that indicate your body is fighting an infection. It can sometimes be complicated to determine if a pressure injury has become infected. This will typically require both sound professional judgement and a clinical assessment, as well as specific tests such as a microorganism and tissue damage examination and imagery scans. In terms of controlling the infection, the main goals are to stop the germs from spreading to other patients, staff, and the environment around them, and also to avoid promoting the creation of superbugs that are resistant to treatment.
Common Infection Risks and Control Goals:
- Local wound infection
- Soft tissue infection
- Osteomyelitis (bone infection)
- Bacteremia (bloodstream infection)
- Using professional judgement and assessments to evaluate pressure injuries
- Preventing the spread of germs to other patients, healthcare workers, and the surroundings
- Avoiding the creation of drug-resistant germs
Preventing Pressure Injury
Preventing pressure sores involves identifying patients who are at risk, improving their overall health, reducing physical stress, and educating about pressure sores. According to the ACP (American College of Physicians) clinical guidelines from 2015, it’s recommended to perform a risk assessment to identify patients at risk of developing pressure sores.
Several systems have been created to estimate who is at the risk of pressure sores. These systems help to figure out which patients should be given preventative measures or early treatments. The most commonly used systems for this are the Braden and Norton scales.
Reducing physical stress involves lessening factors that can cause pressure sores, such as friction, shear (sideways force), pressure, and moisture. It’s essential for preventing the development of pressure sores. Research has shown that educating healthcare providers and patients can reduce the occurrence of pressure sores and improve their management.